HALF THE ADULT AMERICAN POPULATION HAVE DISC HERNIATIONS WITHOUT LOW BACK PAIN – ANOTHER PROOF FOR THE THORACO-LUMBAR FASCIA MODEL OF LOW BACK PAIN
“Spinal pain, and especially low back pain (LBP), represents the second cause for a medical consultation in primary care setting and a leading cause of disability worldwide. The clinical assessment of pain source can be a challenge because of the complex anatomy and function of the spine; the advanced imaging methods are often not sufficient for a definitive diagnosis because similar findings could be present in either asymptomatic and symptomatic subjects”. From the May 2015 issue of the European Journal of Radiology (Spinal Pain)
“In clinical medicine since some years overdiagnosis is giving rise to growing attention and concern. Overdiagnosis is the diagnosis of a “disease” that will never cause symptoms or death during a patient’s lifetime. It is a side effect of testing for early forms of disease which may turn people into patients unnecessarily and may lead to treatments that do no good and perhaps do harm. Overdiagnosis occurs when a disease is diagnosed correctly, but the diagnosis is irrelevant. The National Insurance for Occupational Diseases regularly recognizes less than 50% of the notified diseases; this might suggest overdiagnosis and possibly overattribution in reporting.” Cherry-picked from the abstract of the December 2014 issue of the Giornale Italiano di Medicina del Lavoro Ed Ergonomia (Overdiagnosis and Defensive Medicine in Occupational Medicine)
A number of years ago, the world’s foremost sports surgeon, Dr. James Andrews, did an informal study with big league pitchers who were visiting him for problems not related to their throwing shoulders. He ran throwing-shoulder MRI’s in these “asymptomatic” individuals and discovered that over 90% of the 31 pitchers he looked at had serious enough issues on their MRI that he could have recommended surgery and been completely justified in doing so. He concluded something along the lines of, If you want an excuse to operate, just run an M.R.I.
Not only does my brother, AN ER PHYSICIAN, verify this fact (he says the problem is so bad as to not to bother with an MRI for musculoskeletal problems until you are to the point where you are willing to have surgery), so does mountains of research. And the kicker is that the same phenomenon of OVERDIAGNOSIS & OVERTREATMENT is seen not only with shoulders, but with spines as well.
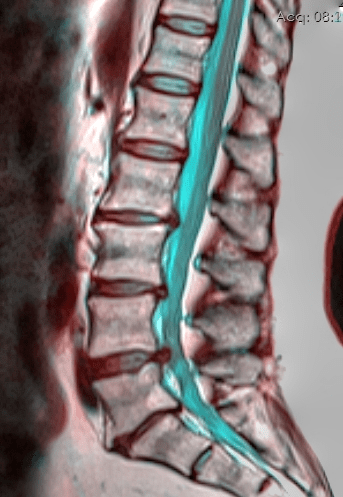
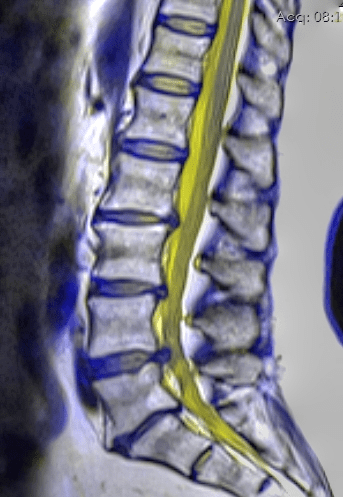
Like Dr. Andrews in the quote above, many of you have found out the hard way that MRI examinations are not all they’re cracked up to be. Most people already realize that x-rays will not show a Disc Herniation, but they are typically under the impression that an MRI will show anything and everything that might be wrong with you. But if you have followed my blog for any length of time, you are already aware that this is frequently not the case (the same thing is true for SPINAL DEGENERATION as well).
Spend any amount of time researching Disc Herniations and you are likely to come across something known as “Asymptomatic Disc Herniations” (it’s why I wrote the post, TELL ME AGAIN WHY YOU WANT AN MRI? several years ago).
Buckle your seat belts and hold on to your hats because this is going to start getting interesting. Depending upon whose research you believe to be the most accurate, as many as 3 of 4 American adults have Asymptomatic Disc Herniations. What does this mean? Only that the majority of our nation’s adult population is walking around with Disc Bulges / Disc Herniations —– but have no idea since they do not have back pain or leg pain.
FUN FACTS ABOUT DISC HERNIATIONS

- Herniated Discs are not necessarily painful — in fact much of the time they are “asymptomatic”.
- Many studies reveal that the majority of Herniated Discs are asymptomatic (they cause no pain).
- Surgery is not needed to fix most cases of Herniated Discs.
- Spinal Surgery frequently means poor outcomes for Herniated Discs.
- Herniated Discs do not typically get “more herniated” with time (however, they do end up degenerating).
- Although the pain may go away after a period of months or years, Herniated Discs do not resolve on their own.
- Herniated discs cannot be seen with an x-ray.
- Herniated Discs can happen without an overt injury.
- Herniated Discs can happen due to compensation caused by an abnormally rotated pelvis.
- Medical treatment is not necessary for most herniated discs.
- Many disc-like conditions are misdiagnosed (i.e. PIRIFORMIS SYNDROME)
In fact, according to the research I am about to show you, if I rounded up 100 people with an average age of 45, with no history of low back pain; and were to do MRI’s of the lumbar spine on all of them, the results would be as follows.
- 35% – 75% would have Disc Bulges
- Just under 40% would have Disc Protrusions (Disc Herniations contained within the Annulus)
- between one in ten and one in five would have Disc Extrusions (Disc Herniations where the Nucleus Pulposes is actually leaking out of the Annulus) — severe Disc Herniations.
How do I know this? Not only have I learned a thing or two in the twenty six years I have been taking care of patients, but there are numerous scientific studies on the subject that encompass six decades of research. Let’s look at just a few of them. I want you to note that some of the variations between studies has to do with the fact that there are no hard and fast definitions for terms like Disc Herniation, Disc Bulge, Disc Rupture, etc. These terms are often used interchangeably with each other and have the potential to create some confusion.
STUDIES ON ASYMPTOMATIC DISC HERNIATIONS
In one of the modern era’s first studies of its kind, George Washington University Medical Center Orthopedist, Dr. S.W. Wiesel, published his team’s findings in the September 1984 edition of the medical journal Spine (The Incidence of Positive CAT Scans in an Asymptomatic Group of Patients).
“In order to study the type and number of CAT scan abnormalities of the lumbar spine that occur in asymptomatic people, 52 studies from a control population with no history of back trouble were mixed randomly with six scans from patients with surgically proven spinal disease, and all were interpreted by three neuroradiologists in a blinded fashion. Irrespective of age, 35.4% were found to be abnormal. In the over 40-year-old age group, there was an average of 50% abnormal findings.”
In other words, 35 to 50% of the people without pain had overt disc pathology on their CT SCAN.
Six years later, in the March 1990 edition of the American Volume of The Journal of Bone and Joint Surgery, renowned orthopedic surgeon Scott Boden, also working at GWU Medical Center, followed up with a paper titled, “Abnormal Magnetic-Resonance Scans of the Lumbar Spine in Asymptomatic Subjects. A Prospective Investigation“. In it he concluded that,
“We performed magnetic resonance imaging on sixty-seven individuals who had never had low-back pain or sciatica. The scans were interpreted independently by three neuro-radiologists who had no knowledge about the presence or absence of clinical symptoms in the subjects. About one-third of the subjects were found to have a substantial abnormality.
Of those who were less than sixty years old, 20 per cent had a herniated nucleus pulposus. In the group that was sixty years old or older, the findings were abnormal on about 57 per cent of the scans: 36 per cent of the subjects had a herniated nucleus pulposus and 21 per cent had spinal stenosis. There was degeneration or bulging of a disc at at least one lumbar level in 35 per cent of the subjects between twenty and thirty-nine years old and in all but one of the sixty to eighty-year-old subjects.“
1994 saw yet another study published on this topic when Dr. Maureen Jensen’s Magnetic Resonance Imaging of the Lumbar Spine in People without Back Pain was published in the July 14 issue of the New England Journal of Medicine. In this study we learned that,
“Thirty-six percent of the 98 asymptomatic subjects had normal disks at all levels. 52 percent of the subjects had a bulge at at least one level, 27 percent had a protrusion, and 1 percent had an extrusion. Thirty-eight percent had an abnormality of more than one intervertebral disk. On MRI examination of the lumbar spine, many people without back pain have disk bulges or protrusions. Given the high prevalence of these findings and of back pain, the discovery by MRI of bulges or protrusions in people with low back pain may frequently be coincidental.”
Over 50% of asymptomatic individuals had Disc Bulges. But even more importantly, pay attention to that last word, “coincidental” as it relates to imaging findings.
In 1995, Volvo’s award winning ‘Clinical Sciences Study of the Year’ (The Diagnostic Accuracy of Magnetic Resonance Imaging) was published in the December issue of Spine. The present study has presented evidence that…. asymptomatic patients show a high incidence rate of disc herniations (76%). Individuals with minor disc herniations (i.e., protrusion, contained discs) are at a very high risk that their magnetic resonance images are not a causal explanation of pain because a high rate of asymptomatic subjects (63%) had comparable findings.
More than three of four pain-free individuals in this study presented with Disc Herniations that could be seen via advance imaging techniques. I must make note of the fact that this study also found a whopping 85% of the asymptomatic subjects had class 3-5 disc degeneration on MRI as well.
A few years later, the December 1998 issue of the journal Radiology published a study by a group of prominent Swiss researchers and radiologists. These radiologists got their hands on 60 hospital employees with no history of back pain, and then ran all of them through MRI’s of the lumbar spine.
Even though the paper’s conclusion infers that MRI is a wonderful tool for diagnosing back pain in the under-50 crowd, reading between the lines leads one to a different conclusion. 40% of the volunteers had “Disc Protrusions” even though they did not have back pain. Even more amazing was that almost 1 in 5 of the asymptomatic test subjects had a “Disc Extrusion” (severe Disc Herniation).
In Y-2K, Dr. Michael Raskin (M.D. / Attorney) got into the mix with a paper he published in Applied Radiology. In the paper, whose topic pertained to the difficulty of accurately diagnosing personal injury clients, he exposed one of the dirty little secrets that millions of Americans on SSI Disability have known for years — essentially that back injuries are easily faked.
“Asymptomatic individuals with “abnormal” MRI–Recent literature has shown that many anatomical abnormalities of the back, including disc bulges and disc herniations, are quite common in people without back pain. Even prior to magnetic resonance imaging (MRI), the high incidence of disc abnormalities in the lumbar spine of asymptomatic individuals was quite well known.
In 1956, a study using postmortem examinations of the entire spine showed a 39% prevalence of posterior disc protrusions. In 1968, a study using myelography in 300 asymptomatic individuals demonstrated lumbar disc abnormalities in 24%.
Using computed tomography (CT), a 1984 study reported the prevalence of herniated discs in asymptomatic individuals to be 20% in those under the age of 40 years and 27% in those over the age of 40. Since MRI became a clinically available diagnostic imaging tool in the mid 1980s, multiple studies have confirmed that more than half of adults without symptoms have significant disc bulges or disc herniations. Furthermore, the prevalence of [asymptomatic] disc herniations increases with age.”
Did you catch that? We have known that there is a huge prevalence of asymptomatic Herniated Discs since 1956. The truth is that we have had an idea of this since a study published in a 1921 issue of the journal, Medical Times (HERE).
A study published one year later in a 2001 edition of the journal Spine came to similar conclusions. According to the University of Washington’s Department of Radiology, “Back pain is the second most common symptom-related reason for clinician visits in the United States. Up to 84 percent of adults have low back pain at some time in their lives.”
But despite this, as well as the incredible numbers of MRI’s being done here in the United States, the authors concluded that, “Many MRI imaging findings have a high prevalence in subjects without low back pain. These findings are therefore of limited diagnostic use.” Read the previous two sentences again. This is referring to those “coincidental” findings we discussed earlier — a common feature. Because of the crazy numbers of false positives, MRI is often rendered useless (limited diagnostic use).
In 2010, the Indian Journal of Orthopedics published a study called Correlation Between Clinical Features and Magnetic Resonance Imaging Findings in Lumbar Disc Prolapse, where the authors determined that the only finding that was easily correlated was a “centrolateral protrusion or extrusion with gross foramen compromise.”
In other words, if a bulge is just lateral of center, and so big that it pushes on the nerve as it exits the cord through the IVF (Intervertebral Foramen — the small windows on either side of the spine that let the spinal nerves exit the cord), pain correlates well to what’s seen on the MRI. On the other hand, “central bulges and disc protrusions correlate poorly with clinical signs and symptoms… The type of disc herniation (bulge, protrusion, or extrusion) correlates poorly with clinical signs and symptoms.“
How does this phenomenon relate to back surgery? A 2006 study published in Clinical Neurology and Neurosurgery (Symptomatic and Asymptomatic Abnormalities in Patients with Lumbosacral Radicular Syndrome: Clinical Examination Compared with MRI) looked at patients with lower extremity radicular findings (sciatica — leg pain) and tried to see how well it correlated to their MRI.
“On the asymptomatic side, MRI showed abnormalities in 33%, while 23% had asymptomatic root compression. In more than two-thirds of the patients with unilateral LRS there was no exact match between the level predicted by clinical examination and MRI findings. These discrepancies complicate the decision whether or not to operate.”
So, even though other studies say that leg symptoms with a disc bulge is the best indicator a surgery might be warranted, it’s erroneous at least one third of the time — something that was largely confirmed in the December 2015 issue of Biomed Central Musculoskeletal Disorders (Back Pain Less Explained than Leg Pain….).
What if you are one of those people who has already had a back surgery? In December of 2011, a group of six researchers working at Vanderbilt University Medical Center in Nashville, Tennessee, concluded their study on post-surgical asymptomatic Disc Herniations by saying that, “Nearly one-fourth of patients undergoing lumbar discectomy demonstrated radiographic evidence of recurrent disc herniation at the level of prior surgery, the majority of which were asymptomatic….. Clinically silent recurrent disc herniation is common after lumbar discectomy.”
Their findings were reported in the December 2011 issue of Spine. BTW, this was not new information when it was published half a decade ago.
A 1995 offering by a team of physicians and researchers from South Australia’s Department of Orthopedics and Trauma, Royal Adelaide Hospital, had this to say in that March’s edition of Spine. “The findings of this study indicate that long-term improvement of a patient’s symptoms after treatment of disc herniation may occur with or without resolution of the herniation. This and the similar findings in the different groups is consistent with the 10-year clinical results after the treatment of disc herniation reported by Weber.”
This was the conclusion after looking at groups that were treated for their herniated discs in various ways, and noticing that after a decade, 37% of the people in the study still showed herniated disc on MRI. Interestingly enough, there was no rhyme or reason for who hurt and who did not simply by looking at their MRI. Between 25% – 37% of post-surgical asymptomatic patients showed Herniated Discs after their surgeries.
And as crazy as it may sound, there were actually several studies dealing with disc bulges with contralateral symptoms. In other words, even though the disc bulge was on the right, irritating or pinching nerves on the right, the patients had all their symptoms (pain, numbness, weakness, atrophy, etc) on the left, or vise versa.
YOU’RE CONVINCED, BUT WHY DOES IT MATTER?
Great question. Why does it matter? Who really cares if you have Disc Herniations as long as they don’t hurt? Let me give you a couple reasons why, beyond the previous link. For one, research is now saying that if you have Asymptomatic Disc Bulges, they will likely not stay symptomatic forever, probably because they greatly speed up the degenerative process.
Secondly, the inability to correlate disc pathology to physical findings reiterates the importance of understanding the THORACOLUMBAR MODEL OF PAIN as it relates to something known as “DENSIFICATION“. Thus, it will be in your best interest to take a peek at the Top Ten Ways to Fix Your Own Back Problem on my THORACOLUMBAR FASCIA POST. Knowing this DIY information could prove invaluable at some point in your life. Let me give you another example — one that I see several times a week in my clinic.
Let’s say that you start having all the SIGNS OF A HERNIATED DISC. After trying several things that did not help you, you had an MRI. The MRI showed that you have degenerative disc disease at all levels of the lumbar spine, as well as two levels with disc herniations. Your doctor wants you to do CORTICOSTEROID INJECTIONS (along with other members of the “BIG FIVE“).
Once those are proven ineffective, he wants you to visit a Spinal Surgeon. Even if you do not happen to be the sharpest knife in the cupboard, you know one thing —– you know that people that have SPINAL SURGERIES frequently report poor long-term outcomes. All you have to do is ask them.
Be warned, if you do not realize what it really means that many — maybe even most — Disc Herniations are asymptomatic, and that it is frequently impossible to correlate one’s symptoms with what your MRI shows, you will be taken advantage of. How do I know this? Because more than ever, it’s all about the money, and there is big money in Spinal Surgery (see previous link).
One of the ways that I personally try to combat this effect clinically is by prior to starting a regimen of Spinal Decompression Therapy on anyone who’s Sciatica originates in the butt / hip instead of the low back, I make good and sure that they are not dealing with PIRIFORMIS SYNDROME first.
Why is this issue of Asymptomatic Disc Herniation occurring with such regularity? Although I am going to sound like a broken record, we are literally the INFLAMMATION NATION. if you don’t deal with underlying inflammation — not just COVERING IT, but actually addressing it (HERE) — your chances of truly getting better plummet.
This is because inflammation is not only the root cause of most disease processes, but the root cause of disc issues as well (HERE). If you are really interested in getting off of the medical merry-go-round and getting your life back, at least take a look at THIS GROUP OF POSTS.
