 |  |  |
I get a lot of website-related emails. Some are good, some are weird, and a few barely make any sense at all. Here is a friendly email from Ruth in the U.K. taking exception to something I wrote on my CHRONIC ANKLE SPRAINS webpage about injured ligaments, “Your ankle will never be the same after a Grade III sprain“.
How can you say that your ankle will never be the same after a Grade III ankle sprain? Not everyone is the same and I made a great recovery from mine. The ligament in my ankle had completely torn. We are all different 🙂
Let me start by saying how glad I am that Ruth has thus far not had any pain or re-injury with her ankle. Furthermore, I am not sure how long ago she injured herself, how old she is, how heavy she is, whether or not this is a first time injury, if she is a competitive athlete, etc, etc. Neither do I know how her doctors came to the conclusion that her sprain was a Grade III as opposed to a Grade II. All of these things play into the equation.
Any way we choose to slice it, the issue of whether or not a severely injured ankle will ever be the same, is not the same as whether or not the ankle has any pain in it at this particular moment. When I injured my ankle several times over several years, I never developed pain until a couple years or so after the final avulsion (yeah; it was basketball every single time — I no longer play competitively).
Dr. Moshe Solomonow is Emeritus Professor and director of the Bioengineering Division and Musculoskeletal Disorders lab in the University of Colorado’s orthopedics department. His Masters is in Electrical Engineering (Cal) and his Ph.D. is in Engineering Systems and Neuroscience (UCLA — back in 1976). Pay attention to what he wrote in the 2009 issue of the Journal of Bodywork and Movement Therapies (Ligaments: A Source of Musculoskeletal Disorders)
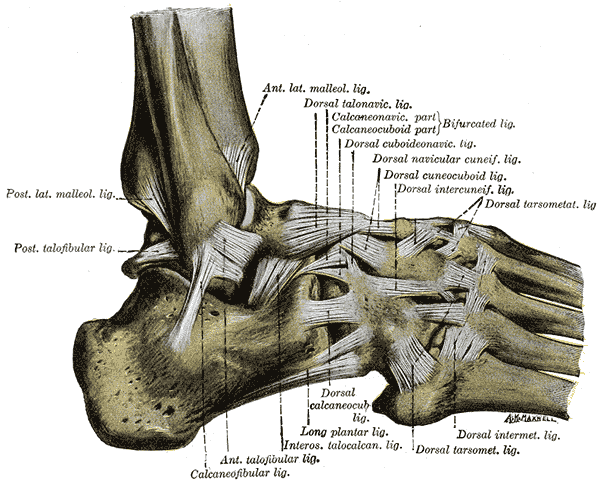
“There are several ligaments in every joint in the human skeleton and they are considered the primary restraints of the bones constituting the joint. Ligaments are also sensory organs and have significant input to sensation and reflexive/synergistic activation of muscles. The muscles associated with any given joint, therefore, also have a significant role as restraints. In some joints, such as the intervertebral joints of the spine, the role of the muscles as restraints is amplified.
The role of ligaments as joint restraints is rather complex when considering the multitude of physical activities performed by individuals in routine daily functions, work and sports, the complexity of the anatomy of the different joints and the wide range of magnitude and velocity of the external loads. As joints go through their range of motion, with or without external load, the ligaments ensure that the bones associated with the joint travel in their prescribed anatomical tracks, keep full and even contact pressure of the articular surfaces, prevent separation of the bones from each other by increasing their tension, as may be necessary, and ensuring stable motion.
Joint stability, therefore, is the general role of ligaments without which the joint may subluxate, cause damage to the capsule, cartilage, tendons, nearby nerves and blood vessels, discs (if considering spinal joints) and to the ligaments themselves. Such injury may debilitate the individual by preventing or limiting his/her use of the joint and the loss of function.”
The problem with Grade II and III sprains has to do with the way that ligaments heal. Ligaments heal with much less strength and elasticity than the original tissue. In fact, most pathology texts will tell you that the very best an injured ligament can heal, is about 60% — maybe 70% in rare cases. This fact alone tells me that range of motion must be affected. And whenever joint motion is affected, MECHANORECEPTION / PROPRIOCEPTION is affected as well.
Although we are talking about an ankle, this is true for every joint in the body including the spine (actually far greater for the spine). In fact if you were to look at all the x-rays of the necks in the above link, I would venture to guess that despite severe degeneration, many of these people went for years — or even decades —- after their initial injury, before having pain (HERE’S WHY).
When Proprioception (the body’s ability to sense stretch, pressure, movement, and position in joints) is adversely affected, the result will always be degeneration of the affected joint. Understand that this degeneration is not an overnight process — even in people who have CHRONIC PAIN post-injury. Like I said, my pain did not show up until at least a couple years after my last (third) avulsion fracture. But show up it eventually did.
This is why rehab and restoration of ROM are so critical for the injured patient — whether we are talking about ankles, knees, backs, or necks (and let’s be honest, a neck is about twenty times more neurologically and mechanically complex than a knee or ankle). By restoring as much strength and motion as is humanly possible as quickly as possible, it improves proprioception, slows down the degenerative process, and helps prevent (or at least slow down) the onset of chronic pain.
I say “slows down” instead of stops or reverses because according to a 2013 issue of The Open Rehabilitation Journal (Ligament Injury and Healing: A Review of Current Clinical Diagnostics and Therapeutics) there is no way to completely stop the process of post-injury degeneration.
“Ligaments are the most frequently injured tissues within a joint. When an applied load causes all fibers to become nearly linear, the ligament continues to absorb energy until tensile failure or disruption of the tissue. Just as it does with overstretched ligaments, joint instability occurs with ligament disruptions or tears, often with more severity. When ligaments are stretched or elongated past a certain point for a prolonged period of time, they can lose their ability to retain their original shape.
When this occurs, the ligament becomes lax and unable to properly support the joint, leading to instability and pain, and eventually to OA [osteoarthritis aka Degenerative Arthritis] of the joint. Although research suggests that persisting collagen abnormalities may be the most critical aspect of regaining ligament tissue function, virtually all other tissue components are likely to play equally important roles in tissue function, either directly or indirectly “
What are these components? I have shown you several times (HERE and HERE come immediately to mind that Scar Tissue (FIBROSIS) is dramatically different than normal tissue. Listen to these authors spell out the way that Scar Tissue is different.
- The COLLAGEN FIBERS are smaller
- The Collagen Fibers are disorganized
- There are flaws between Collagen Fibers
- Lots of cellular and ECM turnover (probably due to cells injury and cell death — severely affects FIBROBLASTS)
- Lower ECM to Fibroblast ratio
- Higher cell density (dense tissue is inflexible tissue)
- Immature Collagen crosslinks (see my FASCIA PAGE)
- Too much Type III (immature) Collagen and not enough Type I Collagen (mature)
- And the list goes on and on and on
The real question, however, is how should these injuries be treated? In other words, even though study after study after study says that soft tissues (ligaments included — especially spinal ligaments) are extremely difficult to image with standard technology such as MRI, that’s what we continue to use. Just be aware that what will happen is that you are likely to be told that there is nothing really wrong with you except some “age-appropriate” arthritic changes. So, as long as you do not have a broken bone or other contraindication, controlled motion is the place to start.
“Overall, it appears that carefully controlled exercise plans promote healing of injured ligaments. Motion itself causes an increase in blood flow to the affected joint, providing the damaged tissue of the ligament with nutrients and metabolites necessary for its repair and healing. Under loading conditions, cells within the ligament sense tissue strains and respond by modifying the tissue.
Mobilization for the treatment of soft tissue damage has also been found to decrease muscle atrophy, osteoporosis, adhesions, and joint stiffness following injury. Studies have indicated that, even in healthy and diseased older adults, short-term high-intensity strength training is well tolerated and helps reduce proinflammatory cytokines and knee joint loads.”
But here, folks, is the rub. Standard medical fare is getting a lot of things bass-ackwards when it comes to treating these injuries effectively. Despite the fact that “motion is lotion,” the medical community continues on with their drugs — even though they frequently do not meet the current guidelines for standards of care. Need I give you an example? The easiest by far would be “THE BIG FIVE” — and most specifically NSAIDS and CORTICOSTEROIDS. The same authors in the same study go on to say that…
“NSAIDs have been a mainstay treatment in ligament injuries for many years, especially in the case of acute sports injuries, but new research has shown that these anti-inflammatory drugs are only mildly effective in relieving the symptoms of most muscle, ligament, and tendon injuries and are potentially deleterious to soft tissue healing. Corticosteroid injections have also been a long-standing treatment regimen for musculoskeletal disorders, including ligament injuries.
Although steroid injections have been shown effective in decreasing inflammation and pain in ligament injuries for up to six to eight weeks, they inhibit the histological, biochemical, and biomechanical properties of ligament healing. Mounting evidence has shown that corticosteroid injections into injured ligaments have an adverse effect on healing. For instance, corticosteroid injections into ligaments and tendons have also been known to inhibit fibroblast function and thus collagen synthesis, even to the extent of causing collagen necrosis [death] at the injection site.
Steroid-injected ligaments have been shown to be smaller in cross sectional area and weaker in integrity, as manifested by decreases in peak tensile strength and load (energy) to ligament failure. Given the inhibitory effects corticosteroid injections have on ligament healing, many experts now caution against their use for treating ligament injuries, especially in athletes.”
Did you catch that? Anti-inflammatory meds don’t cut muster. The thing is, none of it is new information. If you go back and look at THIS POST, I show you exactly the same thing. The link is to an article I did a year ago on the Inflammation / Scar Tissue / Fibrosis / Degeneration connection, that was written using my pathology text book — copyright 1987. It really is true — the more things change, the more they stay the same. The cold hard truth is that when ligaments do heal, there are often problems.
And when they don’t…. “Osteoarthritis is the long-term consequence of nonhealed ligament injuries and continues to be the most common joint disorder in the world.” Corticosteroids and NSAIDS (IBUPROFEN and others) only serve to hurry the process along. And while you will probably be told that ACETAMINOPHEN is safer, after doing a few minutes of research, you might be convinced otherwise.
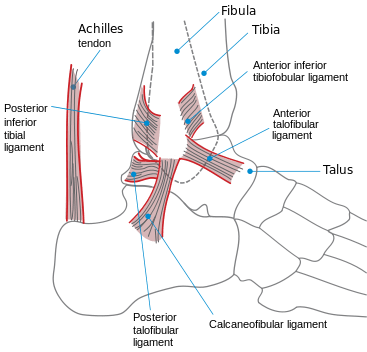
GRADING THE SEVERITY INJURED / SPRAINED LIGAMENTS
The thing I want you to grasp while going through this short section is that inflammation always (that is always as in always) leads to fibrosis — the medical name for Scar Tissue. Furthermore, firbrosis always (that is always as in always) leads to degeneration. HERE is the post on this subject. Also, while it’s relatively easy to grade a KNEE or ankle injury, it’s far more difficult to grade a neck injury in similar fashion.
GRADE I SPRAIN: There is damage to a small percentage of the collagen fibers that make up the ligament. This damage produces local INFLAMMATION (not the same as swelling, of which there will probably be some). There will be some degree of pain in the area, but even in the absence of rehab, there should be no significant long-term instability.
GRADE II SPRAIN: There are a greater number of the ligament’s collagen fibers damaged. This produces a greater inflammatory response with much greater pain and edema / swelling.
GRADE III SPRAIN: The damage to the collagen fibers that make up the ligament is so great that there is a complete tear / rupture of the ligament. Besides intense pain and swelling, this injury is marked by long-term joint instability. In some cases, surgery can be necessary to attempt to solve the joint stability issue. Just be aware that for an ligamentous injury to cause permanent symptoms, it does not have to be a Grade III
WHAT ARE LIGAMENTS?
Image by Nephron
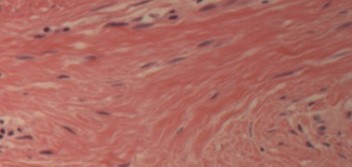
Image by DRDoubleB
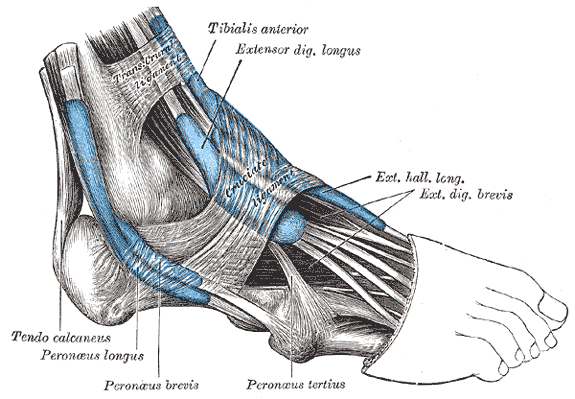
Ligaments are the connective tissue that attach bones to other bones. They also provide joint strength and stability. When ligaments are healthy, they should allow normal range of motion in a joint, while preventing movements or joint motion that could potentially injure the joint. In order to accomplish this, ligaments have to be both strong and elastic at the same time. Ligaments are both strong and elastic because they are made up of a protein called COLLAGEN. Healthy ligaments are made up of roughly
- 90% Type I Collagen
- 9% Type III Collagen
- 1% Fibroblasts (these are the cells that manufacture collagen)
Fortunately, the most abundant kind of collagen found in ligaments, Type I Collagen, is a mature collagen tissue. It provides the most strength and elasticity. This is important because Type III Collagen is immature collagen tissue and is neither strong nor elastic. Just remember this, once the Fibroblast cells have produced Type III Collagen fibers (something that they are continually doing), it takes about 100 days to mature them into Type I Collagen.
If we look at ligaments under the microscope (see “Healthy Connective Tissue” image above) we notice something very important. The individual Collagen Fibers are arranged in a parallel fashion to each other. This provides both strength and elasticity and enables ligaments to resist the incredible tensile forces they continually face on a day-to-day basis. After ligaments are injured, the healing process frequently occurs in a random and unorganized pattern (Scar Tissue).
The individual Collagen Fibers, instead of being aligned to each other in a parallel fashion, are tangled, twisted, mangled, and wadded up in all three dimensions —- SORT OF LIKE A HAIRBALL. You can see this phenomenon when you look at the picture of “Injured Connective Tissue” above.
THE PHASES OF HEALING AND REPAIR
Although my COLLAGEN SUPER PAGE talks about 4 stages of healing and repair, we are only going to talk about three of them today —- the Inflammatory Phase, the Repair Phase, and the most importantly, the Remodeling Phase.
- THE INFLAMMATORY PHASE: This first phase lasts about 72 hours and is caused by cellular death. When cells are injured, they die. And when they die, they rupture their contents into the fluid (extracellular fluid) surrounding the tissue. The contents of the cell contain compounds that cause LOCAL INFLAMMATION (not to be confused with ‘Systemic Inflammation’ — click the link to see the difference) Inflammation is not itself synonymous with swelling, but instead attracts swelling to it. Use R.I.C.E. during this phase of the injury process — Rest, Ice, Compression (Ace Bandage), and Elevation (the injured area must be above the heart to be considered to be ‘elevated’). It is important to remember that anti-inflammatory meds are said to cause injured tissues to heal with as much as 1/3 less strength and elasticity. This is why ICE is so important during this initial phase.
- THE REPAIR PHASE: The Repair Phase of healing is characterized by INCREASED FIBROBLASTIC ACTIVITY. In other words, the body kicks the collagen manufacturing machinery into high gear. Between the Fibroblasts and blood platelets, a sort of “scab” is created. This phase is over within six short weeks (90+% of it takes place with the first three weeks). Just remember that the collagen that is laid down during this phase of healing is Type III (immature). Fibroblastic activity can be increased by ‘loading‘ the injured ligament (various types of massage, tissue work, adjustments — if tolerable, etc). Many in the medico-legal arena (insurance attorneys — think MVA here) will argue that healing of injured ligaments should be complete within 6-8 weeks. This is true, depending on what the definition of healing is. The tissue is all there, it just has not been matured. This happens in the final phase.
- THE REMODELING PHASE: Interestingly enough, every study on tissue remodeling is saying that this phase lasts longer than the study that came before it. For a long time, The Remodeling Phase was said to last up to a year. I am now seeing studies that are doubling that estimate. This phase is characterized not only by the maturation of Type III Collagen into Type I Collagen, but by tissue organization. By “Tissue Organization” I mean that the tangled, web of scar tissue is remodeled over time into tissue that is much more organized and parallel. This is why STRETCHING, STRENGTHENING, and functional training is so critical for the long term health of any injured joint.
WHAT HAPPENS WHEN THE
HEALING PROCESS FAILS?
Using the word ‘fail’ in this context might not be completely accurate. Like I said earlier, the very best you can hope for a severely injured ligament to heal is about 70%. This means that even though you might not be having pain at the moment, the injured joint is going to be less stable and have some degree of abnormal joint motion. This causes diminished PROPRIOCEPTION, which always leads to Degenerative Arthritis.
Sure, arthritis might not show up today, and it might not show up tomorrow — it is a process that often takes some time to rear it’s ugly head. But if all the ingredients are present, eventually it will make an appearance. Fortunately, any time that scar tissue is present, TISSUE REMODELING may be a treatment option. Just be aware that ligamentous scarring can cause abnormal tissue loading that can wind up leading to SUBLUXATIONS, FASCIAL ADHESIONS, TENDINOSIS, or even CHRONIC MUSCLE STRAINS. It is always nice to be able to intervene prior to severe degeneration taking place.
For more information on the ways that Tissue Remodeling for the microscopic adhesions that tend to form in Connective Tissues that have been injured either chronically or acutely, visit the link above. I would also suggest that you view our PATIENT TESTIMONIALS as well. And for those of you struggling with chronic conditions of all sorts, it would benefit you to take the ten minutes it will take to read THIS POST. Oh, be sure to like, share or follow on FACEBOOK since it’s still a great way to reach the folks you love and value most.
