IS YOUR CHRONIC NECK PAIN AFFECTING YOUR BRAIN AND NERVOUS SYSTEM?
“According to an NIH study released last year, some 25.3 million American adults have experienced chronic pain every day for the past three months. Chronic pain is a poorly understood condition in which the nervous system consistently fires out pain signals for a long period of time, sometimes without an actual injury to trigger it, and it turns out that it might change our bodies on a genetic level. A new study out of McGill University is one of the first to find that chronic pain may change the DNA in our immune systems and brain.” From the January 28 issue of MedicalDaily.com (Chronic Pain Changes DNA In The Brain And Immune System) by Lecia Bushak
“Chronic musculoskeletal pain is one of the most intractable clinical problems faced by clinicians and can be devastating for patients. Perhaps no other symptom induces such fear and loathing as chronic pain. Most images of pain are focused on portraying negative emotions and the intrusive nature of the pain experience. Clinicians as people fear chronic pain, a symptom that demands attention and intrudes into every aspect of a person’s life.
Clinicians also loathe chronic pain, perhaps the symptom that brings more patients into our practices than any other but also the symptom most likely to make us feel helpless as healers” Dr. Leslie Crofford from a 2015 issue of the Transactions of the American Clinical And Climatological Association (Chronic Pain: Where the Body Meets the Brain)
“Some recent studies have also shown that chronic pain can actually affect a person’s brain chemistry and even change the wiring of the nervous system. Cells in the spinal cord and brain of a person with chronic pain, especially in the section of the brain that processes emotion, deteriorate more quickly than normal, exacerbating many of the depression-like symptoms.
It becomes physically more difficult for people with chronic pain to process multiple things at once and react to ongoing changes in their environment, limiting their ability to focus even more. Sleep also becomes difficult, because the section of the brain that regulates sense-data also regulates the sleep cycle. Untreated pain creates a downward spiral of chronic pain symptoms, so it is always best to treat pain early and avoid chronic pain.” Integrative Pain Center of Arizona (The Long-Term Effects of Untreated Chronic Pain)
“Chronic pain is certainly a difficult condition to live with, affecting everything from your activity levels and your ability to work to your personal relationships and emotional states. But did you know that it could also be affecting your brain and the way that it functions? Chronic pain doesn’t just affect a singular region of the brain, but in fact results in changes to multiple important regions, which are involved in many critical functions and processes.
Various studies over the years have found changes to the hippocampus, in addition to reduction of gray matter in the dorsolateral prefrontal cortex, amygdala, brainstem and right insular cortex, to name a few. Pain’s effects on the brain may seem overwhelming, but there’s good research to suggest that the changes are not permanent; they can be reversed when patients receive treatment for their painful conditions.
“Gray matter abnormalities found in chronic pain,” a 2009 study concluded, “do not reflect brain damage, but rather are a reversible consequence … which normalizes when the pain is adequately treated.” The 2011 study concurred, suggesting that “treating chronic pain can restore normal brain function in humans.”” From Brenda Poppy’s post (How Pain Can Seriously Affect Your Brain) on the Pain Management Resource Blog
We already know that about 1/3 of all Americans (about 100,000,000 million people) are dealing with some degree of Chronic Pain (HERE). And of these, according to the American Academy of Pain Medicine, not quite one third are coping with HEADACHES and CHRONIC NECK PAIN — tied for the number two cause of Chronic Pain behind LOW BACK PAIN.
If you are one of the millions of people dealing with Chronic Neck Pain, what do you do when THE MEDICATIONS no longer work? It’s a question that each and every one of you in this boat has or will be asking, if for no other reason, simply because of what the science says your pain is doing to your brain.
I showed you via the first link of the previous paragraph that those of you living with Chronic Pain are degenerating your brains at a rate 10 times higher than the general population. Unfortunately, that’s just the tip of the iceberg. Thanks to Chronic Neck Pain, some people wind up living with things like FIBROMYALGIA and CENTRAL SENSITIZATION. Allow me to show you how crazy the newest studies on this topic really are specifically for those of you struggling with Chronic Neck Pain.
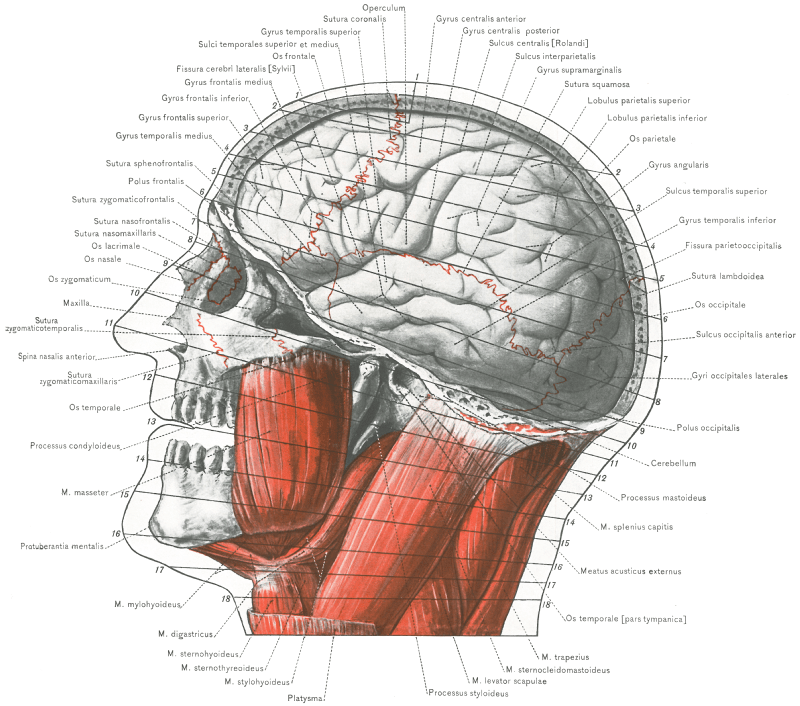
- ABNORMAL BRAIN ACTIVITY AND CHRONIC NECK PAIN: Sure, we’ve seen that generalized Chronic Pain leads to abnormalities in the brain, but what about Chronic Neck Pain specifically? A study from February’s issue of the Journal of International Medical Research (Abnormality of Spontaneous Brain Activities in Patients with Chronic Neck and Shoulder Pain) answers this question by saying, “Most chronic pain diseases are accompanied by structural and functional changes in the brain. This initial structural and functional MRI study of CNSP (chronic neck and shoulder pain) revealed characteristic features of spontaneous brain activity of CNSP patients.” Believe me when I tell you that spontaneous brain activity (activity that happens out of the blue for no good reason) is never a good thing.
- CONCUSSIONS, BRAIN ISSUES, AND CHRONIC NECK PAIN: Last month’s issue of Medicine (Concussion / Mild Traumatic Brain Injury-Related Chronic Pain in Males and Females) concluded that, “Of the 94 participants diagnosed with mTBI, head/neck and bodily pain were reported by 93% and 64%, respectively…… a primary complaint of head and/or neck, or bodily pain that persists long after concussion – one of the most common types of mild traumatic brain injury (mTBI) – represents an activation of brainstem structures.” Not only have I shown you that HEAD INJURIES are bad news in ways the general public CANNOT BEGIN TO COMPREHEND, but loss of consciousness (LOC) is a huge deal when it comes to Chronic Neck Pain. “Participants who experienced LOC during the concussive event and those who reported head and neck pain had significantly higher pain scores than those who did not experience LOC and those without head and neck pain.“
- CHRONIC NECK PAIN, NECK DYSFUNCTION, AND MIGRAINE HEADACHES: In a study from January’s issue of the European Journal of Physical and Rehabilitative Medicine (Musculoskeletal Disorders of the Upper Cervical Spine in Women with Episodic or Chronic Migraine), we see just how devastating this link between Chronic Neck Pain and MIGRAINE HEADACHES really is. The authors, a group of doctors and researchers from Spain and Brazil, concluded that, “Women with migraine showed reduced cervical rotation compared to healthy women. Significant differences for flexion- rotation test were also reported, suggesting that upper cervical spine mobility was restricted in both migraine groups. Referred pain elicited on manual examination of the upper cervical spine mimicking pain symptoms was present in 50% of migraineurs.” For more on the Upper Cervical Subluxation and its ability to adversely affect the brain, I talked a bit about it the other day (HERE).
- CHRONIC NECK PAIN, CATASTROPHISING, AND DEPRESSION: When it comes pain, there are catastrophizers (it’s the worst ever — SOCCER FLOPPERS) and minimizers (it’s no big deal, I’m fine — MONTY PYTHON’S BLACK KNIGHT). Two studies from 2016, one from Medicine (Factors Associated with Increased Risk for Pain Catastrophizing in Patients with Chronic Neck Pain) and the other from the Pan African Medical Journal (Chronic Neck Pain and Anxiety-Depression: Prevalence and Associated Risk Factors) had some things to say about ANXIETY / DEPRESSION and their link to Chronic Neck Pain. Even though doctors want to way over-emphasize Depression’s causal role in Chronic Pain, I’ve always argued that the opposite is a far more accurate description of what’s really going on — pain is causing the Depression. “Chronic neck pain is a frequent reason for consultation. It’s a highly prevalent condition with about two thirds of the adult population affected at some time in their lives. 10% neck pain recurs or persists with consequences which are responsible for physical disability and high health care cost. In our study which concerned eighty patients with chronic neck pain, a state of anxiety was found in 68.4% cases, and 55.7% patients had depression. High pain intensity, clinical insomnia, and a high level of depression/anxiety were strongly associated with high pain catastrophizing in patients with chronic neck pain. Depression was the strongest predictor of high pain catastrophizing. In conclusion, poor psychological states should be addressed as an important part of pain management in chronic neck pain patients…” You’ll see how this is done shortly.
- CHRONIC NECK PAIN, CHRONIC TRIGGER POINTS, AND ABNORMAL NERVOUS SYSTEM FUNCTION: There are two sides of the “Myofascial” coin; TRIGGER POINTS and FASCIAL ADHESIONS. Both can be brutal, and while in most cases intimately linked to each other, are not the same thing. A year ago in June, the journal Pain Medicine published a study called Prevalence of Myofascial Pain Syndrome in Chronic Non-Specific Neck Pain. “Chronic non-specific neck pain is a frequent complaint. In recent years, case reports about myofascial pain syndrome (MPS) are emerging among patients suffering from pain. MPS is a regional pain syndrome characterized by myofascial trigger points (MTrP) in palpable taut bands of skeletal muscle that refer pain to a distance, and that can cause distant motor and autonomic effects. All participants presented with MPS. MTrPs of the trapezius muscles were the most prevalent, in 93.75% of the participants. Furthermore, active MTrPs in the levator scapulae, multifidi, and splenius cervicis muscles reached a prevalence of 82.14%, 77.68%, and 62.5%, respectively. MPS is a common source of pain in subjects presenting chronic non-specific neck pain.” Now check this out. A study from a 2011 issue of Chinese Medicine (Myofascial Trigger Points: Spontaneous Electrical Activity and its Consequences for Pain Induction and Propagation) stated, “Active MTPs contribute significantly to the regional acute and chronic myofascial pain syndrome apart from localized pain conditions, such as chronic tension type headache and migraine, myofascial low back pain, chronic prostatitis/chronic pelvic pain syndrome in men, lateral epicondylalgia [HERE], headache, mechanical neck pain, whiplash syndrome and fibromyalgia. Current evidence shows that spontaneous electrical activity at myofascial trigger point originates from the extrafusal motor endplate. The spontaneous electrical activity represents focal muscle fiber contraction and/or muscle cramp potentials depending on trigger point sensitivity. Active myofascial trigger points may play an important role in the transition from localized pain to generalized pain conditions via the enhanced central sensitization, decreased descending inhibition and dysfunctional motor control strategy.” Although there is a lot here, suffice it to say that TP’s usually indicate that something is fouled up in the nervous system. Read my link on Trigger Points above to see how to successfully address them.
- WHIPLASH WILL SCREW YOU UP IN WAYS YOU COULD NOT HAVE IMAGINED UNTIL YOU WERE REARENDED: After talking extensively about how medicine was on the cusp of solving the WHIPLASH PROBLEM, the authors of last October’s issue of the Journal of Orthopedic and Sports Physical Therapy (Whiplash Continues it’s Challenge) had to admit that, “management of whiplash, especially the challenge of lessening the rate of transition to chronicity, has yet to be achieved.” A 2015 issue of BMC Public Health echoed that thought with a study (Five Years After the Accident, Whiplash Casualties Still Have Poorer Quality of Life in the Physical Domain than Other Mildly Injured Casualties) that let us know that, “Defined as an acceleration-deceleration mechanism in the neck, whiplash is the most common injury in road accidents, particularly for motorist. Considered a minor injury, whiplash is reported to generate both short and long-term consequences, such as neck pain, headache, dizziness, sensory disorder and reduced neck mobility. In most studies described in the international literature, more than half of whiplash casualties reported non-recovery one year after the accident. Five years after the accident, whiplash casualties were twice as likely to report pain as non-whiplash casualties (40.7 % vs. 22.2 %). Whiplash casualties suffered from neck pain.” Furthermore, after looking at just under 400 studies on the topic, Belgian researchers writing in last April’s Manual Therapy (Does Muscle Morphology Change in Chronic Neck Pain Patients?) revealed that muscles can be so screwed up by whiplash injury that they sometimes turn to fat. “Increasing evidence suggests that morphological muscle changes, including changes in cross-sectional area (CSA) or fatty infiltration, play a role in chronic neck pain. Fatty infiltration, which could be accountable for an increased CSA, of both cervical extensors and flexors seems to occur only in patients with WAD.” By the way, WAD stands for Whiplash Associated Disorders (HERE).
- WHIPLASH, NECK PAIN, AND BLOOD FLOW TO THE BRAIN: Last August’s issue of EBioMedicine (Altered Regional Cerebral Blood Flow in Chronic Whiplash Associated Disorders) said that, “There is increasing evidence of central hyperexcitability in chronic whiplash-associated disorders (cWAD). WAD includes neck pain and headache as the most frequent symptoms. Although WAD includes regional neck symptoms, the common presence of psychological manifestations suggests the involvement of central nervous system processes in WAD symptom presentation.” What could possibly be causing some of this mess? Among other things, researchers have discovered that, “The present study shows that, compared with healthy volunteers, chronic WAD patients have increased perfusion of the right posterior cingulate gyrus and right precuneus, and decreased perfusion of the right superior temporal gyrus, right parahippocampal gyrus, left inferior frontal gyrus, right dorsomedial thalamus, and in the bilateral insular cortex.” In other words, with WAD, the blood flow to the brain is all kinds of screwed up. The real problem is that this is known to lead to “LEAKY BRAIN / NERVE / CORD SYNDROME“.
- YOU CAN’T FIX WHIPLASH ASSOCIATED DISORDERS (INCLUDING CHRONIC NECK PAIN) WITH DRUGS: Get in a whiplash accident and I promise you will be prescribed drugs — probably lots of drugs (PAIN MEDS, NSAIDS, MUSCLE RELAXERS, and if chronic, CORTICOSTEROIDS and ANTI-DEPRESSANTS. The thing is, I’ve shown you over and over again via peer-review that this approach does not only not work, it’s DOWNRIGHT DANGEROUS. “Whiplash-associated disorder (WAD) is a group of symptoms and clinical manifestations resulting from rear-end or side impact. Despite the wide use of medications in WAD, the published research does not allow recommendations based on high evidence level. In chronic WAD, the use of nonsteroidal anti-inflammatory drugs is more concerning due to potential gastrointestinal and renal complications with prolonged use and lack of evidence for long-term benefits. Antidepressants can be used in patients with clinically relevant hyperalgesia, sleep disorder associated with pain, or depression. Anticonvulsants are unlikely first-choice medications, but can be considered if other treatments fail. The use of opioids in patients with chronic pain has become the object of severe concern, due to the lack of evidence for long-term benefits and the associated risks. Extreme caution in prescribing and monitoring opioid treatment is mandatory. As for any chronic pain condition, concomitant consideration of rehabilitation and psychosocial interventions is mandatory.” In other words, since all the medical community has to offer you is THE BIG FIVE, you might want to take a rain check and look into something that actually addresses the underlying problem instead of merely covering the symptoms.
- CHRONIC NECK PAIN AND ABILITY TO BREATHE: Remember that the level of C1 (Atlas) has the potential to affect breathing via the part of the brainstem known as the Medulla Oblongota. A brand new review of almost 80 studies from this month’s American Journal of Physical Medicine and Rehabilitation (The Association Between Neck Pain and Pulmonary Function) concluded that, “Significant difference in maximum inspiratory and expiratory pressures were reported in patients with chronic neck pain compared to asymptomatic subjects. Some of the respiratory volumes were found to be lower in patients with chronic neck pain. Muscle strength and endurance, cervical range of motion, and psychological states were found to be significantly correlated with respiratory parameters. Lower Pco2 in patients and significant relationship between chest expansion and neck pain were also shown. Respiratory retraining was found to be effective in improving some cervical musculoskeletal and respiratory impairment. Functional pulmonary impairments accompany chronic neck pain.” The truth is, breathing is one of the most-affected (in a good way) arenas when it comes to chiropractic adjustments (HERE).
- VISUAL EFFECTS AND VERTIGO: A study from January’s issue of Frontiers in Neurology (Inaccurate Saccades and Enhanced Vestibulo-Ocular Reflex Suppression during Combined Eye–Head Movements in Patients with Chronic Neck Pain: Possible Implications for Cervical Vertigo) determined about Chronic Neck Pain and VERTIGO that, “In patients with chronic neck pain, the internal commands issued for combined eye–head movements have large enough amplitudes to create accurate gaze saccades; however, because of increased neck stiffness and viscosity, the head movements produced are smaller, slower, longer, and more delayed than they should be. VOR suppression is disproportionate to the size of the actual gaze saccades because sensory feedback signals from neck proprioceptors are non-veridical, likely due to prolonged coactivation of cervical muscles. The outcome of these changes in eye–head kinematics is head-on-trunk stability at the expense of gaze accuracy. In the absence of vestibular loss, the practical consequences may be dizziness (cervical vertigo) in the short term and imbalance and falls in the long term.” By the way, saccades (a normal eye movement) are defined as quick (ballistic) movement of both eyes simultaneously between two or more points in the same direction.
- CHRONIC NECK PAIN AND DHEA: You may have heard of DHEA before as a nutritional supplement. The reason is that (according to a well known online encyclopedia), DEHA is “also known as androstenolone and is an endogenous steroid hormone. It is the most abundant circulating steroid hormone in humans, in whom it is produced in the adrenal glands, the gonads, and the brain, where it functions predominantly as a metabolic intermediate in the biosynthesis of the androgen and estrogen sex steroids.” In other words, no DHEA, and you can count on FEMALE PROBLEMS, INFERTILITY, LOW T, and SEXUAL DYSFUNCTION. Another study —- this one from the August issue of Pain Medicine (Different DHEA-S Levels and Response Patterns in Individuals with Chronic Neck Pain, Compared with a Pain Free Group) compared groups of “persons with chronic neck pain and controls without present pain.” The authors, all Swedish doctors and researchers, concluded that, “the plasma DHEA-S levels appeared to be lower among the persons with chronic neck pain, compared with the control group.“
- CHRONIC NECK PAIN AND INSOMNIA: INSOMNIA sucks (as does SLEEP APNEA) and is frequently a function of something called SYMPATHETIC DOMINANCE. The November 2015 issue of Pain Physician (Factors Associated with Increased Risk for Clinical Insomnia in Patients with Chronic Neck Pain) concluded that, “Insomnia is highly prevalent among people with chronic pain conditions. Because insomnia has been shown to worsen pain, mood, and physical functioning, it could negatively impact the clinical outcomes of patients with chronic pain. Neck pain development; 22.9% of patients met the criteria for clinically significant insomnia. In analysis, high pain intensity, the presence of musculoskeletal pain, and a high level of depression were strongly associated with clinical insomnia in patients with CNP. Among these factors, a greater level of depression was the strongest predictor of clinical insomnia. This study was conducted in a single clinical setting including a selected study population with a homogeneous racial background. Insomnia should be addressed as an indispensable part of pain management in CNP patients with these risk factors, especially depression.” The problem is, the medical community is going to address it with one of the most dangerous drugs on the market — SLEEPING PILLS.
- BRAIN, MEMORY, AND CHRONIC NECK PAIN: I’ve shown you how in people with TYPE III PAIN, their pain plays on a loop — sort of like the cassette tape of a bad memory going around and around and around on auto-reverse (anyone older than 35 will understand). A study from January’s edition of Pain Physician (Neural Correlates of Maladaptive Pain Behavior in Chronic Neck Pain – A Single Case Control MRI Study). “Functional magnetic resonance imaging (fMRI) showed distinct brain activation patterns that depended on the side of rotation (pain-free versus painful side) and the kind of movement (distracted versus non-distracted head rotation). Interestingly, brain areas related to the processing of pain such as primary somatosensory cortex, thalamus, insula, anterior cingulate cortex, primary motor cortex, supplementary motor area, prefrontal cortex, and posterior cingulate cortex were always more strongly activated in the non-distracted condition and when turning to the left. In the patient, maladaptive pain behavior and the activity of pain-related brain areas during imagined head rotations were task-specific, indicating that the activation and/or recall of pain memories were context-dependent.“
- CORRECTING FORWARD HEAD POSTURE AFFECTS BRAIN: I’ve shown you a bunch of studies revealing how bad FHP (Forward Head Posture) really is — not to mention the fact that it’s intimately associated with Chronic Neck Pain (HERE). Not surprisingly, a study from last October’s issue of Physical Therapy Science (Effects of Neurofeedback Training on the Brain Wave of Adults with Forward Head Posture) showed that it affects the brain as well. “Owing to the prevalence and popularity of computers, students and workers are increasingly experiencing musculoskeletal abnormalities in their neck and shoulders. Using computers and smart phones for many hours, coupled with lack of exercise, may cause stiffness of the muscles in the neck and shoulders, inducing weakness in the soft tissues. Such postural and lifestyle habits lead to forward head posture (FHP), which can cause relative compensation such as increased lordosis in the junction of the skull and neck [a hump] consistent muscular contraction inducing changes in the craniocervical junction. Posture affects people in terms of psychological, physical, structural, and functional changes. Specifically, bad posture is thought to increase the possibility of a decline in learning efficiency, attention, and memory. The column and the brain, in particular, are closely situated in terms of anatomical structures. According to previous research, FHP may induce a reduction in proprioceptive sensibility, in addition to interference between the nerves and the muscles. These problems may, in turn, affect an individual’s mind and emotions. It is thought that neurofeedback training, a training approach to self-regulate brain waves, enhances concentration and relaxation without stress, as well as an increase in attention, memory, and verbal cognitive performance. Therefore an effective intervention method to improve neck pain and daily activities.” While this is well and good, there are ways to deal with FHP that actually help correct it — not just manage it. But………
- FHP CANNOT BE CORRECTED WITH ADJUSTMENTS ALONE: The December 2015 issue of the journal, Chiropractic and Manual Therapies published a study called Does Cervical Lordosis Change After Spinal Manipulation for Non-Specific Neck Pain? In this study, the authors (a group of European chiros and research scientists) looked at sixty volunteers who underwent several weeks of chiropractic adjustments. Not surprisingly, and as I have told you time and time again, adjustments alone never solve the reverse cervical curve (FHP). “This study found no difference in cervical lordosis (sagittal alignment) between patients with mild non-specific neck pain and matched healthy volunteers. Furthermore, there was no significant change in cervical lordosis in patients after 4 weeks of cervical spinal manipulation.” The good news is, there are things you can do to help reverse the reversed cervical curve, and most of them can be done at home under the supervision of a competent chiropractor (HERE).
- NECK ADJUSTMENTS AFFECT BRAIN AND METABOLIC PATHWAYS: Knowing the numerous ways that CHIROPRACTIC ADJUSTMENTS AFFECT THE NERVOUS SYSTEM, we should not be surprised to find a study showing us that adjustments affect metabolic pathways as well. The January 2017 issue of Evidence-Based Complementary and Alternative Medicine (Glucose Metabolic Changes in the Brain and Muscles of Patients with Nonspecific Neck Pain Treated by Spinal Manipulation Therapy) looked at PET Scans — remember that PET Scans are used to find cancer by finding areas of increased sugar uptake (HERE) — of people with Chronic Neck Pain, determining that, “Glucose uptake in skeletal muscles showed a trend toward decreased metabolism after SMT (spinal manipulative therapy)… Other measurements indicated relaxation of cervical muscle tension, suppression of sympathetic nerve activity, and pain relief after SMT. Brain processing after SMT may lead to physiological relaxation via a decrease in sympathetic nerve activity.” Again, why is this a big deal? Can anyone say “SYMPATHETIC DOMINANCE“? Chiropractic adjustments have been shown time and time again to help down-regulate the Sympathetic Nervous System (the “fight or flight” response) that so frequently ruins people’s lives when it is flipped to the “on” position.
- STRESS MANAGEMENT AND COGNITIVE BEHAVIORAL THERAPY FOR THOSE WITH CHRONIC NECK PAIN DRAMATICALLY IMPROVES OUTCOMES: Last May’s respective issues of the Journal of Back and Musculoskeletal Rehabilitation (Effect of a Stress Management Program on Subjects with Neck Pain) and Clinical Rehabilitation (Group-Based Multimodal Exercises Integrated with Cognitive-Behavioral Therapy Improve Disability, Pain and Quality of Life of Subjects with Chronic Neck Pain) concluded that, “A group-based multidisciplinary rehabilitation program including cognitive-behavioral therapy was superior to group-based general physiotherapy in improving disability, pain and quality of life of subjects with chronic neck pain. The effects lasted for at least one year. Stress management has positive effects on neck pain patients.” This is not really anything new as the venerable Hans Seleye (AN ENDOCRINOLOGIST) was discovering the General Adaptation Syndrome and HPA-Axis back in the 1930’s and 40’s.
Knowing this information is great. After all, knowledge really is power (HERE). However, the real rubber-meets-the-road question is what are you who are struggling going to do with it? In other words, how can you, the Chronic Neck Pain sufferer, use this information to help your cause, decrease your pain, and increase your ability to function on a day to day basis? Glad you asked.
- FIRSTLY: You must understand the difference between acute inflammation and chronic inflammation, and control the latter (HERE). Diet plays a huge roll in this, and the diet I recommend to my patients helps control CHRONIC INFLAMMATION like nothing you’ve ever seen before (HERE).
- SECONDLY: You will need to read a bit about PHASE I and PHASE II of solving the underlying physical / mechanical basis of your neck pain. If you fail to address these, or address them out of order, I promise that your results will be compromised — especially in people with the more severe problems. For those of you who are really struggling, this can be difficult (HERE).
- THIRDLY: You are going to have to learn how to control your thoughts and fears, get active, and develop strategies to cope with the situation. While formal group CBT (Cognitive Behavioral Therapy) mentioned earlier can be fantastic, many of you will find the same level of therapeutic benefit by becoming part of a community on an internet message board. I don’t really care how you go about it, but you are going to need some sort of sounding board and support group, possibly someone with letters behind their name.
- FOURTHLY: Purchase your own pain aids and modalities. There are any number of great “gizmos” that have amazing potential modulate / down-regulate Chronic Neck Pain. COLD LASER is amazing as is WHOLE BODY VIBRATION. Electric massagers, Theracanes or similar, FOAM ROLLERS, EXTENSION AIDS and EXERCISE BALLS, cervical pillows, home traction devices (over-the-door, DAKOTA, or any number of others), heat lamps, and even ULTRASOUND as long as you use it correctly / safely…… And that’s just for starters. There are almost an infinite number of things out there that can help you help yourself. The tough part is trying to wade through the sales pitches by those individuals and companies PREYING ON PEOPLE WITH CHRONIC PAIN.
- FIFTHLY: Educate yourself. As I said earlier, knowledge is power. Find people or sites and study. What makes my site different than most others is that I’m not trying to sell you anything. My goal is to weed through the sales pitches and BS so that you can have the facts, the whole facts and nothing but the facts. Just realize that when it comes to science, the facts are (FOR ANY NUMBER OF REASONS) constantly changing.
Don’t kid yourself. This list could be infinite if I had the time to sit down and write a book. HERE is a bit more in-depth information on how you might accomplish some of these things. And as I always suggest to people, after studying the situation, sit down and create a personalized EXIT STRATEGY for yourself — a way to take your life back and start living again. If you want to see some examples of this in action, take a look at some of our CASE HISTORIES.
