CHRONIC NECK PAIN ACCORDING TO THE LATEST RESEARCH



A study from May’s issue of Medicine (Trends in Diagnosis of Painful Neck and Back Conditions...) said this about CHRONIC NECK PAIN.
“In a national population, the prevalence rate for diagnosis of neck and back pain grew 1.8 to 2.3 times faster than the incidence rate. This suggests that the average duration of episodes of care is increasing. Neck and back pain problems are pervasive and associated with chronic pain, disability, and high healthcare utilization. At any given time 10% to 20% of adults will report neck pain symptoms.
The vast majority of back and neck pain complaints are characterized in the literature as non-specific and self-limiting, but with a high frequency of recurrence. This suggests that what happens during the first or incident episode may have a significant influence on the occurrence and severity of subsequent episodes and the development of long-term disability.”
What does this really mean in terms of chronic neck pain?
In plain English it means that you ignore neck pain at your own peril. A failure to deal with your neck issues today means that you’ll likely be dealing with them tomorrow, only it will be worse, with incidents coming closer together and lasting longer, until it all runs together, becoming constant and chronic. This is why the term “self limiting,” while true for colds, FLU, WHOOPING COUGH, CHICKEN POX, and most other infectious diseases, may not be a good descriptor of musculoskeletal problems, including neck pain.
Although statistics have shown that just under a third of all Americans deal with some sort of CHRONIC PAIN ISSUE, a recent article from the American Pain Society (NIH Study Shows Prevalence of Chronic or Severe Pain in U.S. Adults) revealed that according to peer-review, “Nearly 50 million American adults have significant chronic pain or severe pain, according to a new study prepared by National Institutes of Health’s National Center for Complementary and Integrative Health (NCCIH).”
A study from the July/August issue of the Brazilian Journal of Physical Therapy (Prevalence and Factors Associated with Neck Pain: A Population-Based Study) painted a similar picture.
Neck pain is one of the major musculoskeletal disorders in the adult population; its prevalence in the world ranges from 16.7% to 75.1%. This condition has a complex etiology, including a number of factors: ergonomic (strenuous physical activity, use of force and vibration, inadequate posture, repetitive movement), individual (age, body mass index, genome, musculoskeletal pain history), behavioral (smoking and level of physical activity), and psychosocial (job satisfaction, stress level, anxiety, and depression).
In the United States, neck pain was associated with women and people who suffered from some morbidity (respiratory, cardiovascular, and gastrointestinal diseases, among others) and psychological alterations (depression, difficulty falling asleep, and insomnia).
What does this paragraph tell us? For starters it shows us how intimately neck pain is related to inflammation (most of the physical problems listed above can be found filed under “INFLAMMATORY DISEASES“).
This means that a failure to address inflammation means a greater likelihood of failure in addressing your pain — the reason that we’ll see momentarily that “best evidence” says most interventions for chronic neck pain are of little help (the drugs used to treat inflammation cause major problems with the healing of connective tissues such as LIGAMENTS, FASCIA, and TENDONS —- HERE).
With both incidence and prevalence exploding; how badly are our collective wallets being affected?
According to last December’s issue of the Journal of the American Medical Association (US Spending on Personal Health Care and Public Health, 1996-2013), DIABETES and HEART DISEASE were the number one and two costliest diseases facing Americans. Guess what number three was?
“US health care spending has continued to increase, and now accounts for more than 17% of the US economy. with estimated spending of $88.1 billion, low back and neck pain accounted for the third-highest amount. Spending on low back and neck pain and on diabetes increased the most over the 18 years, by an estimated $57.2 billion and $64.4 billion respectively.”
By the way, this was “across all age and sex groups and types of care.” It’s another proof that our healthcare system is “UNSUSTAINABLE“.
Earlier this year, Sarah Boseley of The Gaurdian wrote about this study in an article titled Epidemic of Untreatable Back and Neck Pain Costs Billions, Study Finds. Listen as she echos the futility of most treatments as shown by decades of scientific studies.
“Injections, electrical nerve stimulation, opioid drugs and a whole host of other interventions are not recommended for lower back and neck pain. The Cochrane group have found no evidence in favour of using these or many other interventions; in the UK, guidance from the National Institute for Health and Care Excellence advises healthcare staff not to offer them. Low back and neck pain is an increasingly widespread and expensive condition worldwide, costing the US alone $88 billion a year – the third highest bill for any health condition – despite evidence most treatments do not work.”
She is talking mostly here about THE BIG FIVE, which you already know don’t work well. Let’s look, however, at some things that might be of benefit.
- GENERAL RISK FACTORS FOR NECK PAIN: Less than three weeks ago, a team of five researchers from Duke looked at almost 900 articles and concluded in the journal Musculoskeletal Science and Practice (Identifying Risk Factors for First-Episode Neck Pain: A Systematic Review) that, “Because of the tendency for neck pain to become a chronic issue, it is important to identify risk factors that could encourage prevention and early diagnosis. The strongest psychosocial risk factors were depressed mood, high role conflict, and perceived muscular tension. The most commonly reported physical risk factor was work in awkward/sustained postures. Protective measures found included high perceived empowering leadership, high perceived social climate, leisure physical activity, and cervical extensor endurance. Most risk factors found for neck pain were related to psychosocial characteristics, rather than physical characteristics.” If you are struggling with Depression, make sure to read these amazing posts (HERE).
- NECK PAIN FREQUENTLY STARTS IN THE WORKPLACE: In October, the International Journal of Occupational Medicine and Environmental Health (Determination of Pain in Musculoskeletal System Reported by Office Workers and the Pain Risk Factors) said that risk factors for spinal pain in office workers (52% of the 528 workers quizzed had neck pain) include, “sitting at the desk for a long time without a break, working sitting on a chair that supported only the lumbar area and the arms, having the computer mouse at a distance from the keyboard, having the head inclined at 45° when working, working holding both forearms above the level of the desk, not taking exercise in daily life, and having a moderate or extremely stressful workplace.” The next month the same journal looked at risk of neck pain for all workers in a study titled Risk Factors for Episodic Neck Pain in Workers: A 5-Year Prospective Study of a General Working Population. The biggest factor here were things like work pace, sustained/repeated arm abduction (raising your arms to the side), and high physical exertion.
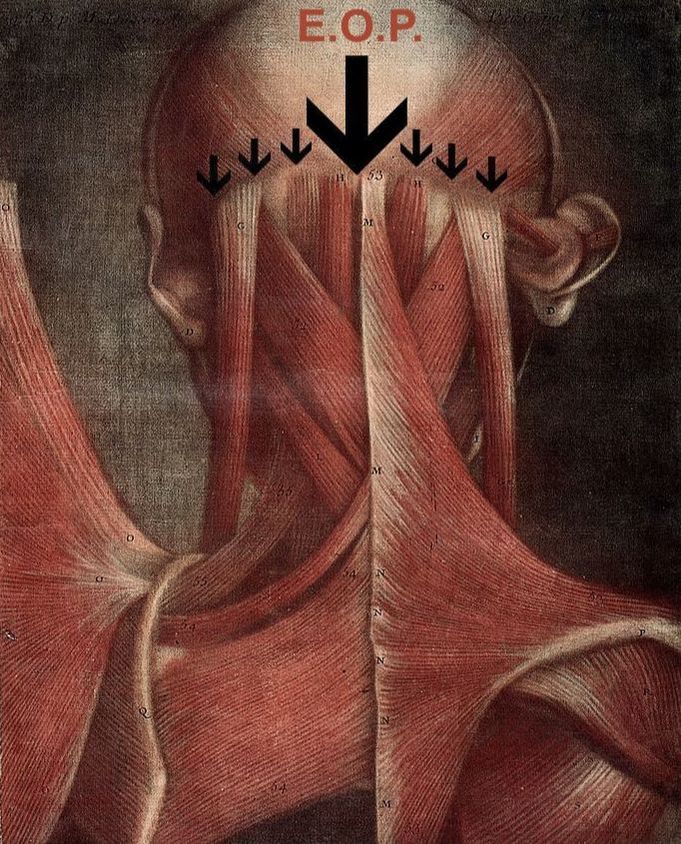
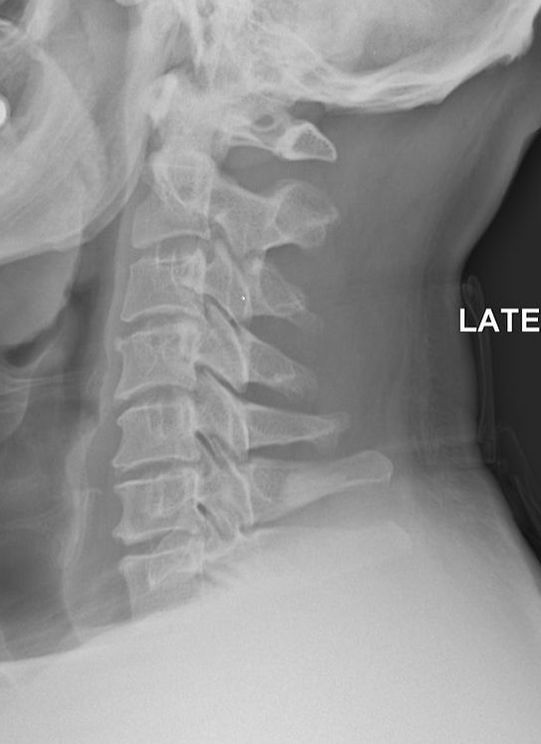
- CHRONIC NECK PAIN TIED TO OCCIPITAL BONE SPURS: If you reach back to the back of your head, halfway between your ears, you can feel a knob of bone called the EOP (External Occipital Protuberance), which is the point where lots and lots of muscles attach. WOLF’S LAW says that bone grows in response to stresses put on it, whether that stress is normal or abnormal. So, if there is abnormal tension in the neck, it only makes sense that the EOP turns into what amounts to an oversized bone spur, which is by the way, a commonly seen occurrence in any chiropractic clinic. A study published in last week’s edition of the Journal of Craniofacial Surgery (An Anatomic Morphological Study of Occipital Spurs in Human Skulls) concluded that, “Occipital spurs are quite common; however, they are also the source of frequent discomfort to the patients. Their role has been implicated in causation of pain at the base of skull, which may extend to shoulder limiting the movement of the shoulder and neck.” The paper said that about 10% of the population has tight enough muscles to cause an occiptial bone spur. The x-rays at the top of the page all have an occipital bone spur (click pics to enlarge). In the middle pic, you can see not only the EOP, but the entire ridge of bone where muscles attach along the back of the skull. This should help you understand why I frequently work on the back of the skull when treating people with chronic neck pain, HEADACHES, or SKULL PAIN.
- NECK PAIN AND TRAUMATIC BRAIN INJURIES IN CHILDREN: After looking at some of my posts on TBI (Traumatic Brain Injuries — HERE is one from just the other day showing how they cause any number of diseases via genetic mutations), make sure to glance at this study from last week’s issue of the Journal of Neurotrauma (A Review of Pain in Children Following Traumatic Brain Injury: Is There More than Headache?), which helped shed some light on this all too common problem by concluding “Headache is a common source of pain in children following traumatic brain injury (TBI). Pain assessment in children after TBI needs improvement, given that pain is linked to worse recovery, poorer quality of life, and can be long-lasting. More rigorous examination of non-headache pain and its role in impeding recovery in children following TBI is imperative, and has the potential to improve the care and management of children with TBI.” This means that if the only treatment your child gets for a CONCUSSION, WHIPLASH or TBI/MTBI is THESE DRUGS, noting is being done to address the problem.
- NECK PAIN AND CHOLESTEROL LEVELS: Three weeks ago the Journal of Orthopedic Science (Associations Between Neck Symptoms and LDL Cholesterol) found a relationship between CHOLESTEROL LEVELS (LDL — the so-called “bad” cholesterol) and chronic neck pain. “Studies have reported associations between neck pain and degenerative changes in the cervical spine in women, and between neck pain and obesity or metabolic syndrome. The 1122 volunteers who participated in this study included 426 men and 696 women. Each subject filled out a questionnaire about any neck pain or neck-shoulder stiffness experienced in the previous 3 months. We recorded the following laboratory results related to metabolic factors, including lipid profiles: total cholesterol, LDL and HDL cholesterol, triglycerides, free fatty acids, glucose, and hemoglobin A1c. The prevalence of neck and shoulder stiffness was significantly higher in women (60.3%) than in men (38.0%). Analyses showed a significant negative correlation between the prevalence of neck pain and LDL cholesterol. LDL cholesterol was correlated with neck pain in this cross-sectional population-based study.” I talked extensively HERE about the intimate relationship between cholesterol and inflammation.
- NECK PAIN AND THE RELATIONSHIP TO TACTILE SENSATION: Researchers from the University of Queensland’s Centre of Research Excellence in Recovery Following Road Traffic Injuries, published a study a few weeks ago in Musculoskeletal Science and Practice (Tactile Acuity is Reduced in People with Chronic Neck Pain). This isn’t surprising considering what we know about the neck as related to RADICULAR PROBLEMS, the authors stated that, “Tactile acuity deficits have been demonstrated in a range of persistent pain conditions and may reflect underlying cortical re-organisation. People with chronic neck pain demonstrated tactile acuity deficits in painful and non-painful regions when measured using the Two-Point Discrimination test, with the magnitude of deficits appearing greatest at the neck. The study also revealed a positive relationship between Two Point Discrimination and pain intensity/duration, further supporting the main study finding.” These findings are intimately related to PROPRIOCEPTION, which when lost, is a huge factor in developing DEGENERATIVE ARTHRITIS.
- CHRONIC NECK PAIN AND CENTRAL SENSITIZATION: CHRONIC PAIN is bad enough on its own but when it becomes “learned,” locked into the brain and playing on a loop, it’s really bad news. This is because in the same way it is almost impossible to unlearn how to ride a bike, it’s likewise difficult to unlearn pain that has been creating neural pathways that can end up more aptly described as highways. A Belgian study published in last week’s issue of Pain Practice (Convergent Validity of the Dutch Central Sensitization Inventory: Associations with Psychophysical Pain Measures, Quality of Life, Disability, and Pain Cognitions in Patients with Chronic Spinal Pain) dealt with CENTRAL SENSITIZATION as related to chronic neck pain. “Symptoms of Central Sensitization have been described in patients with chronic spinal pain. Although a gold standard to diagnose Central Sensitization is lacking, psychophysical pain measures are often used. Moderate to strong associations were found with current pain intensity, quality of life, disability, and catastrophizing.” CATASTROPHIZING is freaking out over your situation. Because there is, as these authors said, no gold standard for diagnosing it, my opinion oon using TISSUE REMODELING on those with potential CS is let her rip — there’s nothing to lose (HERE).
- WHAT’S THE BEST WAY TO TEST FOR CHRONIC NECK PAIN: What would be really cool is if doctors had a way to test people in the same way mechanics hook up your car to their diagnostic computer to see what’s wrong. Unfortunately, the fact that pain is subjective is at least part of what’s led to the OPIOID EPIDEMIC. If you look at the final link in the “Tactile Sensation” bullet above, or better yet, THIS LINK on MRI’s, you quickly realize that imaging — at least in the sense that we currently use it today — isn’t necessarily much help. Thus, my opinion based on a number of studies is that RANGE OF MOTION is the best and easiest way to get a picture of how bad neck pain might be. Although there are a number of companies selling ROM-measuring devices for thousands, or even tens of thousands of dollars, a study from the October issue of JMPT (Intrarater and Inter-rater Reliability of Active Cervical Range of Motion in Patients With Nonspecific Neck Pain Measured With Technological and Common Use Devices: A Systematic Review With Meta-Regression) revealed that simple, low tech, inexpensive devices work just as well. “The use of expensive devices to measure active cervical range of motion in adults with nonspecific neck pain does not seem to improve the reliability of the assessment.“
- HOW BEST TO TREAT THOSE STRUGGLING WITH CHRONIC NECK PAIN: Back in July, eight PT’s wrote an 83 page position paper for their profession called Neck Pain: Revision 2017 Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability and Health From the Orthopaedic Section of the American Physical Therapy Association that was published in the Journal of Orthopedic and Sports Physical Therapy. Their conclusions could be boiled down to a few sentences. “For patients with chronic neck pain with mobility deficits, clinicians should provide a multimodal approach of thoracic manipulation and cervical manipulation or mobilization, mixed exercise for cervical/scapulothoracic regions (neuromuscular exercise, coordination, proprioception, postural training, stretching, strengthening, endurance training, aerobic conditioning, and cognitive affective elements), dry needling, laser, or intermittent traction“
In the words of YODA, correct they are. When treating people with chronic neck pain, the very first thing that must be accomplished is breaking the ADHESED FASCIA and SCAR TISSUE / FIBROSIS. This needs to be followed by “MANIPULATION” (not to be confused with mobilization — HERE). There are so many cool ways to improve PROPRIOCEPTION that can be combined with various forms of EXERCISE (both specific and non).
DRY NEEDLING, LASER THERAPY, and intermittent traction (otherwise known as SPINAL DECOMPRESSION THERAPY) all follow if needed. I have written about these in my PHASE I and PHASE II for dealing with people who have chronic neck pain. Don’t forget how important it is to deal with SYSTEMIC INFLAMMATION (or overabundance of local inflammation) that might be present.
- YOGA IS HELPFUL FOR THOSE WITH CHRONIC NECK PAIN: I have spoken of YOGA on my site previously. The October issue of Complementary Therapies in Clinical Practice (Effects of Yogic Exercise on Nonspecific Neck Pain in University Students) concluded that at least in college students, “The yoga group showed significantly decreased neck pain scores compared with those of the control group.” Last month’s issue of the Journal of Rehabilitative Medicine (Effects of Pilates and Yoga in Patients with Chronic Neck Pain: A Sonographic Study) looked at the effects of neck pain on one of those new imagining technologies mentioned earlier (DIAGNOSTIC ULTRASOUND) determining that although yoga did not change the ultrasound itself, “All 3 types of exercise (yoga, Pilates, and isometrics) had favorable effects on pain and functional scores.” Two weeks ago today, Clinical Rehabilitation (Effects of Yoga on Chronic Neck Pain: A Systematic Review and Meta-Analysis) concluded that, “Yoga has short-term effects on chronic neck pain, its related disability, quality of life, and mood suggesting that yoga might be a good treatment option.”
- WHAT ABOUT THOSE ADJUSTMENTS? I’ve shown you repeatedly that repeated adjustments in and of themselves are a waste (HERE). A study from last month’s issue of Chiropractic and Manual Therapies (The Chiropractic Profession: A Scoping Review of Utilization Rates, Reasons for Seeking Care, Patient Profiles, and Care Provided) looked at hundreds of studies and determined that neck pain is the second most common reason people visit the chiro (LBP is first). Fortunately, the second most common treatment used on these folks (behind manipulation) was soft tissue therapy. But what about the question of when you should be adjusted if you are injured? It was answered by a group of European osteopaths in last month’s issue of Alternative Therapies in Health and Medicine (Immediate Effects of Osteopathic Treatment Versus Therapeutic Exercise on Patients With Chronic Cervical Pain) who concluded that, “Although both interventions were associated with immediately improved ROM and pain after treatment, high velocity, low amplitude manipulation was more effective than craniocervical flexion exercise in improving ROM and visual analog scales (1-10 pain diagrams) during ROM.” Please note the word “immediately“. Very cool, but what I am looking for in my clinic are LONG TERM RESULTS. It’s ironic that as groups of American chiros pine for prescription rights, European physicians are taking courses to learn how to manipulate the spine. In a study published in last week’s issue of BMC Musculoskeletal Disorders (Physicians Using Spinal Manipulative Treatment in The Netherlands: A Description of Their Characteristics and their Patients) a team of four Dutch physicians, chiros, and other similar, were starting to use manual techniques to treat patients.
- WHAT THE HECK IS ACOPOTOMY? According to Qiao Jinlin, the director of China’s Naval General Hospital’s Department of Rehabilitation, “Soft tissue trauma includes muscular pain, fascia and tendon injury, as well as articular cartilage, joint capsule [ligaments] and bursa.” What’s one of the hottest methods of dealing with these problems? I mentioned it earlier —- NEEDLING. I have said for a very long time that while super cool, acupuncture needles are often too small to affect the needed change (which is why I usually use hypodermics). A relatively recent treatment known as Acopotomy (“a non-invasive acupuncture/ micro surgery using a small needle-scalpel invented by Professor Zhu Hanzhang around 30 years ago in China“) is being used to break deeper tissue adhesions. HERE is a super cool video of Dr. Steven Woo of the OG Pain Clinic fixing a shoulder problem. And while there are actually a fair number of studies on acopotomy, a group of six Chinese physicians published a study back in August called Acupotomy Therapy for Chronic Nonspecific Neck Pain: A Systematic Review and Meta-Analysis. After looking at results of ten trials involving 433 patients, the authors concluded that, “Acupotomy therapy may be beneficial to chronic nonspecific neck pain patients.” What’s doubly cool is that these authors also reported that the procedure, used by 360,000 people a day in China, saves over ten billion dollars annually in surgery and other medical services. Take a look at the previous link to see why.
As I have been telling people for nearly three decades, if you want to solve your chronic issues, you’re going to have to step out of the box. In a nation where we account for less than 5% of the world’s population, but are, according to our own government (HERE), using 75% of the world’s medication, it’s clear that we are not as adept at this as we should be.
After all, big pharma, corporate medicine, our government, and the insurance industry, all want to keep you in the box. That way you can be a MONEY-MAKING COMMODITY for decades to come. That way no one upsets the status quo. That way the people at the top of the pyramid make obscene amounts of cash.
If you are looking to step outside the box, I’ve given you some information to help you get started. Nope, it’s not meant to diagnose, treat, or cure diseases — that’s what the FDA says can only happen if you stay in the box. THIS POST is meant to give you a starting point as far as doing your own research. Because after everything shakes out in the wash, your health is up to you.
