FIBROSIS (SCAR TISSUE) AND SURGICAL IMPLANTS
I spend my days dealing with SCAR TISSUE, which the medical community refers to as FIBROSIS. Because of this, it’s not uncommon for me to see people with post-surgical Scar Tissue (HERE, HERE, HERE, HERE, HERE, and HERE are some examples). Many I help, some I don’t. When it comes to treating the people who COME FROM GREAT DISTANCES to see me, I try to be extra diligent to make sure their visit is as fruitful and productive as possible (HERE).
Each and every day, tens of thousands of surgeries are performed in the United States, with significant numbers of these involving some sort of implanted metal, plastic polymer, silicone, etc. Why is this potentially such a big deal? For one, the rates of infection are scary. In 2015, MedScape published an article about joint replacements called Arthroplasty-Associated Infections, which stated, “Infection of arthroplasty may be among the most devastating complications for the patient, as well as for the surgeon.”
In a 2013 study from Orthopedic Reviews dealing with BIOFILMS (Prosthesis Infections after Orthopedic Joint Replacement), the authors revealed,
“Prosthesis-related infection is a serious complication for patients after orthopedic joint replacement, which is currently difficult to treat with antibiotic therapy. Consequently, in most cases, removal of the infected prosthesis is the only solution to cure the infection. Biofilms are medically important, accounting for over 80% of microbial infections in the body, including prostheses and internal fixation devices.
Bacteria usually form biofilm on foreign bodies that are placed in patients for medical reasons, such as peripheral and central venous catheters, heart valves, ventricular assisting devices, coronary stents, arthro-prostheses, fracture-fixation devices, breast implants, intraocular lenses, dental implants, etc.“
The website of the American Academy of Orthopedic Surgeons says,
“Joint replacement infections may occur in the wound or deep around the artificial implants. An infection may develop during your hospital stay or after you go home. Joint replacement infections can even occur years after your surgery. Infections are caused by bacteria. Although bacteria are abundant in our gastrointestinal tract and on our skin, they are usually kept in check by our immune system.
For example, if bacteria make it into our bloodstream, our immune system rapidly responds and kills the invading bacteria. However, because joint replacements are made of metal and plastic, it is difficult for our immune system to attack bacteria that make it to these implants. If bacteria gain access to the implants, they may multiply and cause an infection.”
A study from the February 2011 issue of Injury (Unexpectedly Increased Rate of Surgical Site Infections Following Implant Surgery for Hip Fractures) further revealed that, “Surgical site infections (SSIs) are the most common nosocomial [IATROGENIC] infections after surgery.” Knowing this, it’s not surprising I received this comment / question from Lena over at my old DESTROY CHRONIC PAIN site on WordPress.
Hi!
I have recently been fused L4-L5-S1 (Posterior Lumbar Fusion) at the end of January and all went well. To begin with and after 3 weeks I was able to walk for 45-60 minutes. After 4 weeks I began to get excruciating stabbing muscle spasms at the fused area, which almost makes me fall as my legs fold. My surgeon sent me for another CT Scan and said everything looked perfectly fine. I feel he is only interested in the spine and the screws he placed there. I would like to know how the muscles and the fascia work after fusion and if there is anything I can do to prevent the spasms?I understand they cut through the fascia to reach the spine. How does this heal afterwards? I have been bedridden for 4 weeks now with only little improvement. As soon as I try walking as little as 1/5 of a mile I get flare ups and am back to square one. My back feels weak and the spasms keep me from moving even at snail speed. Would this be normal after a fusion? The surgeon removed my spinous processes and used them for the bone graft instead of getting bone from my hips.
If you could just shortly advise me if my muscle spasms are normal I would be very grateful! Neither the surgeon nor my PT has been able to give me an explanation for the stabbing spasms. I feel like I get stabbed to death several times a day…
Best regards, Lena
Let me first say that this is probably not an infection — at least not in the sense we think of overt infections. However, as you’ve already seen, it’s tough to know if there is a subclinical infection present (HERE is an example of an “Occult Infection”).
We have known since the earliest days of surgery that the simple act of installing foreign substances into people can sometimes — probably more often than anyone cares to admit (HERE and HERE) — cause serious problems. A brand new study from this month’s biomedical journal Nature Materials (Colony Stimulating Factor-1 Receptor is a Central Component of the Foreign Body Response to Biomaterial Implants) addressed this issue.
Twenty five specialists and researchers from the best medical facilities in Massachusetts and Illinois collaborated to learn more about the body’s response to the surgical implantation of “Foreign Body Biomaterials“. The authors admitted in the first sentence that, “immune-mediated foreign body response to biomaterials can compromise the performance of implanted medical devices.”
After looking at this problem in light of the two sides of the immune system — TH-1 & TH-2 — the authors determined that, “Macrophages, via CXCL13 [a CYTOKINE], lead to downstream B cell recruitment, which further potentiated fibrosis. Interestingly CSF1R is significantly increased following implantation of multiple biomaterial classes: ceramic, polymer and hydrogel.” Bottom line, inflammation always leads to fibrosis, which always leads to degeneration (HERE).
After discussing the many types of surgical implants done for a wide variety of health issues, the authors said of them (I put my links in their quote),
“The host senses these implants as foreign and mounts an immune-mediated rejection response. This sequence, known as the fibrotic cascade [FIBROSIS], includes tissue injury, immune recruitment [INFLAMMATION], adhesion [SCAR TISSUE FORMATION], myofibroblast induction [HERE & HERE], and fibrous capsule formation [still more scar tissue], preventing interaction with the surrounding microenvironment, including sensing biochemical stimuli such as pH [HERE], oxygen [HERE], blood glucose levels [HERE], and obstructing nutrient flux.”
Stop and think about this for a moment. This isn’t what’s happening just in the people who have problems with their implant; it’s what is happening in every single case. It’s the norm. How do doctors deal with this problem? They SUPPRESS THE IMMUNE SYSTEM.
“Current approaches for immune system suppression or management of long-term biomedical device often involve broad spectrum antiinflammatories. The major immunosuppressive agents used as standard care for implantation procedures are rapamycin, tacrolimus, everolimus, cyclosporine, and corticosteroids. However, many of these antiinflammatory drugs are not specific to individual immune populations, having multiple targets and differential effects…. Additional T-Cell loss made fibrosis worse, perhaps due to the regulatory T-Cell subset important for suppressing over-reaching immune reactions.”
In English, this means that TREGS (T-Regulatory Cells that train your immune system what to attack, while likewise training it not to attack itself — AUTOIMMUNITY), which are responsible for attenuating the fibrosis cascade, are affected by the process.
It also means that the drugs used to suppress the immune system (see earlier link) are not very specific, driving any number of ADVERSE EVENTS (side effects) — side effects that peer-review says are reported, on average, less than 5% of the time (HERE). Some of these were the same drugs used to suppress the immune system in kidney, liver, and heart transplants, so that the body will not “reject” them. And don’t forget the CORTICOSTEROIDS. In many cases, there are prophylactic ANTIBIOTICS given as well (an extremely controversial issue when you start looking at studies). Even when necessary, they are harsh drugs one and all.
Fortunately, there’s a better way to take care of many cases of degenerative joints. You’ve got nothing to lose by going this route. Why not? Because firstly — as I’ve shown you many times — it doesn’t matter whether we are using MRI / CT / X-RAY or DIAGNOSTIC ULTRASOUND (or for that matter, examining someone for a POTENTIAL DISC HERNIATION) — it’s all but totally impossible to match the patient’s symptoms with their imaging findings. Secondly, be aware that clinics are springing up all over the place to take advantage of this information. What are they doing?
While many are doing some very cool things to help people with degenerative joints avoid surgery, the great thing is that YOU CAN’T GO WRONG by doing at least some of the basics on your own — provided for you free of charge on our site (HERE). Worst case scenario, you get healthier and lose some weight in the process, and then go get the joint replaced — with less systemic inflammation and a better chance of healing the right way.
If you’ve been told you need to get a joint replacement, what do I recommend you do first? Firstly, get your weight under control. With almost 80% of our citizens either OBESE or METABOLICALLY OBESE, this is not only a massive driver of inflammation, it compromises your joints, whether your own or replaced. People tend to say that they can’t lose weight because they can’t exercise due to their degenerative knee or hip. I disproved this myth years ago (HERE).
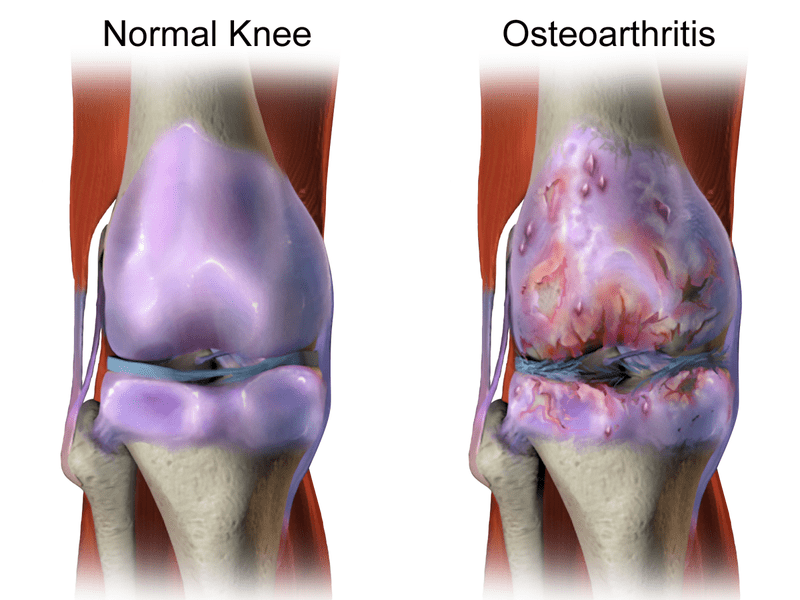
If you simply start addressing the potential drivers of the inflammation, you might be surprised at what happens with your OSTEOARTHRITIS. I have personally seen this approach work for dozens of patients (not all of them mine). One last thing I would consider would be to purchase a COLD LASER to treat yourself with post-surgery. No, I can’t tell you where to get it, but I can tell you that as the technology improves, it gets cheaper and easier to find for the general public.
And as for Lena; while muscle spasms are certainly common — especially after certain injuries or procedures — they are never normal. It is very difficult to say what might be causing this situation — at least in part because it is all but impossible image Fascia with standard imaging tests (even though there is at least one non-standard test that’s been proven quite effective — HERE). But the bigger problem may be; even if you could see it, what are you (or whatever doctor, therapist, chiro, etc you are seeing) going to do about it? The good news is that there are people out there with the solution to your problem — it’s just a matter of finding them.
