Hiatal Hernias’ Relationship to Pain, Dysfunction, and Disease
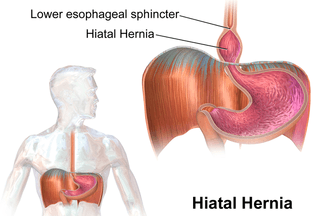
Hiatal Hernia has been called the “great mimic” because it mimics many disorders. A person with this problem can get such severe pains in their chest that they think they are having a heart attack. They may think they have an over acid stomach because they will regurgitate stomach acid after they eat, or their stomach may hurt so badly they will think they have an ulcer. This is just a sampling of the symptoms that may occur from this disorder. From Dr. Russ Tannebaum’s website (Hiatal Hernia: An Overlooked Cause of Disease)
As you might imagine, there are a number of risk factors for developing Hiatal Hernias. Although the biggest two are probably OBESITY and SMOKING, there are plenty of others, including ASTHMA (COUGHING), CONSTIPATION (constantly straining at the stool), regular vomiting (such as might be seen in bulimia), trauma, stress (ADRENAL FATIGUE or SYMPATHETIC DOMINANCE), constant bending, PREGNANCY, too much sitting, or heavy lifting. Let me show you the symptoms of an HH.
- HIATAL HERNIA CAN BE ASYMPTOMATIC: Remember that only about 10% of of Hiatal Hernias create any symptoms at all — not a unique situation when it comes to health and healthcare (HERE).
- HIATAL HERNIA AND ACID REFLUX: Although reflux can be caused by lots of things (TOO LITTLE OR TOO WEAK STOMACH ACID BEING THE MOST COMMON), I’ve shown you how HH causes reflux. Thus, if you are constantly experiencing regurgitation, there is a significantly increased chance you have a Hiatal Hernia.
- HIATAL HERNIA, ESOPHAGITIS AND ESOPHAGEAL STRICTURE: Although HH can cause stomach acid to reflux all the way up into the mouth (I’ve treated a number of patients who actually have rings of chapped redness around their mouths from being burned by their own acid at night), it’s the lower esophagus that bears the brunt of the damage. Stomach acid where it should not be (where it there is no mucous lining to protect it) can cause the formation of both scar tissue (FIBROSIS) and stricture / constriction / loss of elasticity in the lower esophagus. It can also cause something called Barrett’s Esophagus (precancerous lesions). As you might suspect, all of these increase the chances of developing full-blown cancer.
- HIATAL HERNIA, MOUTH & THROAT ISSUES: This could be dry mouth, bad breath, bleeding gums, chronic cough, rough or scratchy voice, hoarseness, and / or trouble swallowing. Speaking of trouble swallowing….
- HIATAL HERNIA & TROUBLE SWALLOWING: Known as dysphagia, it’s simple to see that with everything we’ve covered so far, trouble swallowing would be a natural sequelae. This was shown in a study from last August’s issue of Current Gastroenterology Reports (Hiatus Hernia as a Cause of Dysphagia). “Dysmotility because of impaired contractility and vigor can occur as a consequence of repeated acid exposure from the acid pocket within the hernia, and the resultant poor clearance subsequently worsens this insult. As such, dysphagia appears to be more common with increasing hiatus hernia size. Furthermore, mucosal inflammation can lead to fibrotic stricture formation and in turn obstruction.“
- HIATAL HERNIA & DIGESTIVE ISSUES: These are similar to what you get with other common digestive issues; post-meal bloating, gas, nausea, and even vomiting. Be aware that vomiting blood is never a good sign (copious amounts of blood in the stool will appear black). Also be aware that in many cases, indigestion will manifest as chest pain thanks to the stomach encroaching into the thoracic cavity.
- HIATAL HERNIA & TROUBLE BREATHING: Although it was mentioned as a risk factor, the November issue of the Clinical Respiratory Journal (Contribution of Hiatal Hernia to Asthma in Patients with Gastroesophageal Reflux Disease) concluded that “The patients with GERD with asthma have a high prevalence of Hiatal Hernia.”
- HIATAL HERNIA AND MIGRAINE HEADACHES: Although there are about a million potential causes of MIGRAINE HEADACHES, add one more to the list — Hiatal Hernia. In a study published in last July’s issue of the Middle East Journal of Digestive Diseases (Association of Gastrointestinal Functional Disorders and Migraine Headache: A Population Base Study), a group of physicians from Iran’s Shiraz University came to some interesting conclusions after looking at over 1,000 random patients with GI complaints. “This study revealed an association between migraine and gastrointestinal functional disorders including IBS, reflux and dyspepsia. Hiatal hernia was the only abnormal endoscopic finding in patients with migraine headache.“
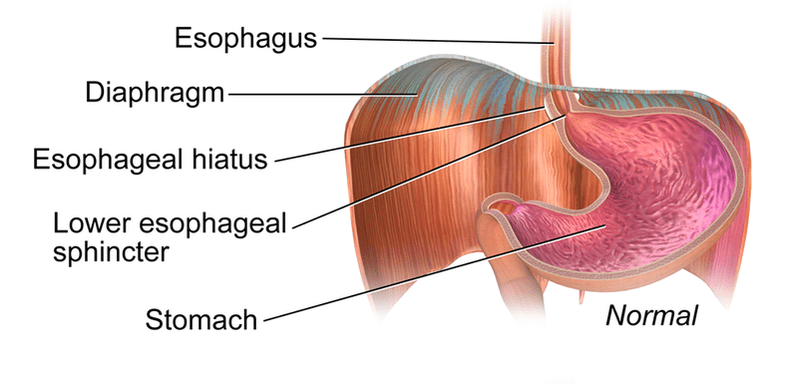
- HIATAL HERNIA AND HEART: Hiatal Hernias can mimic heart problems by causing chest pain. A case study from last July’s issue of BMJ Case Reports (Hiatal Hernia Mimicking Heart Problems) described heart attack-like symptoms in a 74 year old man whose stomach had worked its way from the abdominal cavity, through the diaphragm’s esophageal hiatus, and into the thoracic cavity with the heart. While not an everyday occurrence, neither are these massive HH’s uncommon.
- HIATAL HERNIA AND ANEMIA: Although there are numerous causes of ANEMIA, according to a 2015 study from the International Journal of Gastroenterology and Hepatology, one of them is “underappreciated” (An Underappreciated Cause of Intermittent Chest Pain, Asthma, and Iron Deficiency Anemia). Peer-review abounds with similar studies — not surprising considering loss of blood is the most common cause of anemia.
- HIATAL HERNIA, SEIZURES & SYNCOPE (FAINTING): The more the stomach is pulled upward into the thoracic cavity, the greater the chances it irritates the VAGUS NERVE. Because of it’s heavy parasympathetic action (see my earlier link on Sympathetic Dominance), stimulation of the Vagus can cause dizziness, fainting, and even seizures (or what appear to be seizures — HERE). July’s issue of the Baylor University Medical Center Proceedings (Deglutition Syncope) carried a case study on this very thing — “a 48-year-old man presenting with transient syncopal episodes that occurred while eating, caused by an intrathoracic stomach due to a hiatal hernia.” For the record, deglutition = swallowing.
- HIATAL HERNIA AND TROUBLE BENDING OVER: Because bending forward can cause the stomachs of those with significant Hiatal Hernia to enter the thoracic cavity, it’s on the the list as well.
Although you can see how bad things can get, it’s actually worse than that. As crazy as it may seem, Hiatal Hernias can actually kill you. That’s why doing whatever it takes to get better — hopefully without having to undergo surgery — is a big deal, and potentially a huge boost to your health.
RISK FACTORS & SYMPTOMS OF A HIATAL HERNIA
As you might imagine, there are a number of risk factors for developing Hiatal Hernias. Although the biggest two are probably OBESITY and SMOKING, there are plenty of others, including ASTHMA (COUGHING), CONSTIPATION (constantly straining at the stool), regular vomiting (such as might be seen in bulimia), trauma, stress (ADRENAL FATIGUE or SYMPATHETIC DOMINANCE), constant bending, PREGNANCY, too much sitting, or heavy lifting. Let me show you the symptoms of an HH.
- ASYMPTOMATIC: Remember that only about 10% of of Hiatal Hernias create any symptoms at all — not a unique situation when it comes to health and healthcare (HERE).
- REFLUX: Although reflux can be caused by lots of things (TOO LITTLE OR TOO WEAK STOMACH ACID BEING THE MOST COMMON), I’ve shown you how HH causes reflux. Thus, if you are constantly experiencing regurgitation, there is a significantly increased chance you have a Hiatal Hernia.
- ESOPHAGITIS AND ESOPHAGEAL STRICTURE: Although HH can cause stomach acid to reflux all the way up into the mouth (I’ve treated a number of patients who actually have rings of chapped redness around their mouths from being burned by their own acid at night), it’s the lower esophagus that bears the brunt of the damage. Stomach acid where it should not be (where it there is no mucous lining to protect it) can cause the formation of both scar tissue (FIBROSIS) and stricture / constriction / loss of elasticity in the lower esophagus. It can also cause something called Barrett’s Esophagus (precancerous lesions). As you might suspect, all of these increase the chances of developing full-blown cancer.
- MOUTH & THROAT ISSUES: This could be dry mouth, bad breath, bleeding gums, chronic cough, rough or scratchy voice, hoarseness, and / or trouble swallowing. Speaking of trouble swallowing….
- TROUBLE SWALLOWING: Known as dysphagia, it’s simple to see that with everything we’ve covered so far, trouble swallowing would be a natural sequelae. This was shown in a study from last August’s issue of Current Gastroenterology Reports (Hiatus Hernia as a Cause of Dysphagia). “Dysmotility because of impaired contractility and vigor can occur as a consequence of repeated acid exposure from the acid pocket within the hernia, and the resultant poor clearance subsequently worsens this insult. As such, dysphagia appears to be more common with increasing hiatus hernia size. Furthermore, mucosal inflammation can lead to fibrotic stricture formation and in turn obstruction.“
- DIGESTIVE ISSUES: These are similar to what you get with other common digestive issues; post-meal bloating, gas, nausea, and even vomiting. Be aware that vomiting blood is never a good sign (copious amounts of blood in the stool will appear black). Also be aware that in many cases, indigestion will manifest as chest pain thanks to the stomach encroaching into the thoracic cavity.
- TROUBLE BREATHING: Although it was mentioned as a risk factor, the November issue of the Clinical Respiratory Journal (Contribution of Hiatal Hernia to Asthma in Patients with Gastroesophageal Reflux Disease) concluded that “The patients with GERD with asthma have a high prevalence of Hiatal Hernia.”
- MIGRAINE HEADACHES: Although there are about a million potential causes of MIGRAINE HEADACHES, add one more to the list — Hiatal Hernia. In a study published in last July’s issue of the Middle East Journal of Digestive Diseases (Association of Gastrointestinal Functional Disorders and Migraine Headache: A Population Base Study), a group of physicians from Iran’s Shiraz University came to some interesting conclusions after looking at over 1,000 random patients with GI complaints. “This study revealed an association between migraine and gastrointestinal functional disorders including IBS, reflux and dyspepsia. Hiatal hernia was the only abnormal endoscopic finding in patients with migraine headache.“
- HEART: Hiatal Hernias can mimic heart problems by causing chest pain. A case study from last July’s issue of BMJ Case Reports (Hiatal Hernia Mimicking Heart Problems) described heart attack-like symptoms in a 74 year old man whose stomach had worked its way from the abdominal cavity, through the diaphragm’s esophageal hiatus, and into the thoracic cavity with the heart. While not an everyday occurrence, neither are these massive HH’s uncommon.
- ANEMIA: Although there are numerous causes of ANEMIA, according to a 2015 study from the International Journal of Gastroenterology and Hepatology, one of them is “underappreciated” (An Underappreciated Cause of Intermittent Chest Pain, Asthma, and Iron Deficiency Anemia). Peer-review abounds with similar studies — not surprising considering loss of blood is the most common cause of anemia.
- SEIZURES & SYNCOPE (FAINTING): The more the stomach is pulled upward into the thoracic cavity, the greater the chances it irritates the VAGUS NERVE. Because of it’s heavy parasympathetic action (see my earlier link on Sympathetic Dominance), stimulation of the Vagus can cause dizziness, fainting, and even seizures (or what appear to be seizures — HERE). July’s issue of the Baylor University Medical Center Proceedings (Deglutition Syncope) carried a case study on this very thing — “a 48-year-old man presenting with transient syncopal episodes that occurred while eating, caused by an intrathoracic stomach due to a hiatal hernia.” For the record, deglutition = swallowing.
- TROUBLE BENDING OVER: Because bending forward can cause the stomachs of those with significant Hiatal Hernia to enter the thoracic cavity, it’s on the the list as well.
Although you can see how bad things can get, it’s actually worse than that. As crazy as it may seem, Hiatal Hernias can actually kill you. That’s why doing whatever it takes to get better — hopefully without having to undergo surgery — is a big deal, and potentially a huge boost to your health.
WHAT CAN BE DONE TO HELP REDUCE HIATAL HERNIA SYMPTOMS WITHOUT RESORTING TO SURGERY?
If you are diagnosed with reflux, whether from Hiatal Hernia or not, the very first thing that will happen is that you will be prescribed an H2 BLOCKER, or far more likely, a PPI (Proton Pump Inhibitor). All you have to do is follow the links to see that these drugs (especially the latter) have been in the news for the past several years — and none of it is good. As far as medical care of an HH is concerned, the other option is surgery to repair the hiatus.
Although it appears that most people do well with the surgery, peer-review abounds with studies dealing with those who don’t (so do internet message boards and Facebook groups). Bottom line, if there are ways to avoid having the surgery, by all means use them. If you have one of those massive Hiatal Hernias where the stomach is in the thoracic cavity, I’m not sure there’s really another option.
- DO WHATEVER YOU CAN TO GET OFF PPI’S: In researching this post, I came across any number of message boards where people were trading information on getting off of PPI drugs, many of whom had been on them for decades (plural). There is actually a school of thought that PPI’s, over time, actually lead to HH. Regardless, these drugs are bad news because they have a myriad of side effects, are meant to be used no more than six weeks a year, and are extremely hard to get off of (addictive) for people who have been on a long time.
- QUIT SMOKING: Nuff said. Along these same lines, be aware that alcohol is a common cause of reflux as well.
- CHANGE YOUR CRUDDY DIETARY HABITS: Not surprisingly, Hiatal Hernia is largely a disease of the Westernized world. Correct eating will not only allow you to reduce what might be the single largest risk factor (obesity) by LOSING WEIGHT, but not eating junk both reduces inflammation and helps with the whole GERD thing. Bear in mind that the official stance of the medical community (I’ve seen the studies and GUIDELINES) is that changing one’s diet has little to no bearing on a HH. My stance is that you never go wrong cleaning up your diet. After you’ve done an ELIMINATION DIET to see what foods you might be reacting to, get them out of your life. Oh; and for heaven’s sake, don’t eat shortly before going to sleepytown (within three or four hours of bed or nap time). And as if I really need to say it; don’t overeat. If I have to define “overeating” for you, you may be a bigger problem than your HH.
- SLEEP HABITS: As we’ve seen, Hiatal Hernias affect breathing. So does SLEEP APNEA. The number one risk factor for both is obesity (see previous bullet). Also, many people with HH will prop the head of their bed up on books or blocks to prevent the stomach from pulling upward into the diaphragm, as well as helping prevent acid from making its way upward as well.
- DRINK PLENTY OF WATER: One of the single best regulators of STOMACH ACID is water. The average person does not drink nearly enough.
- MASSAGE THERAPY, CHIROPRACTIC, AND OSTEOPATHIC MANIPULATION: There are tricks to manually push the top of the stomach down from the thoracic cavity to it’s natural home in the abdominal cavity, many of which can be done on your own (YouTube abounds with such videos)
- THE HEEL DROP: This is my favorite “trick,” and involves drinking a significant amount of water quickly (I’ll not debate here whether the water needs to be warm or cold), and then rise up on your toes, dropping sharply onto your heels. Repeat. The force of the heel strikes cause the stomach that’s already been weighted down by water, to “drop” downward out of the diaphragm and into the abdominal cavity. I’ve been using this technique for patients for thirty years — very simple and super effective for many of them. In similar fashion, I’ve often wondered if REBOUNDING ON A TRAMPOLINE could accomplish the same thing in healthier individuals (anyone with experience here, feel free to chime in).
- DEAL WITH SIBO, LEAKY GUT, DYSBIOSIS, H. PYLORI, AND CANDIDA: Although I could have covered a number of others here, this should give you a starting point. Just bear in mind that all of these “GUT ISSUES” (SIBO, LGS, and DYSBIOSIS —- including but not limited to CANDIDA and H. PYLORI) have the ability to magnify HH symptoms.
- CHANGE THE WAY YOU GO #2: By this I mean that some of you might benefit from a squatty potty. There is a fantastic article over at Nature’s Platform on the subject, called Health Benefits of the Natural Squatting Position (the back half of the article has some very cool material from peer-review).
- LOOK AT YOUR MEDICATIONS: Be aware that there are any number of PRESCRIPTION DRUGS that are known to cause reflux.
In some cases, surgery to reduce the Hiatal Hernia and repair the torn hiatus is inevitable — almost always the case with huge HH’s. For those of you who have tried everything else, it is something to at least look into. Bear in mind, however, that according to a large study published just a few months ago in the Journal of the Society of Laproendoscopic Surgeons (Long-Term Patient-Reported Outcomes of Paraesophageal Hernia Repair), five thoracic surgeons from Cambridge and Tufts concluded… “
Long-term patient-specific outcomes showed comparable, encouraging results between open and laparoscopic repair of PEH without mesh reinforcement. However, half of those undergoing laparoscopic repair required the use of medication for symptom control.”
Did you catch that? Having your HH repaired only reduces your chances of needing ongoing GERD meds by 50%.
In another study, this one from the Annals of Surgery (Paraesophageal Hernias: Operation or Observation?), researchers and physicians answer the question of whether people would be better off to just go ahead and have the HH surgery and get it over with. After comparing “watchful waiting” (WW) to “elective laparoscopic paraesophageal hernia repair” (ELHR), the authors, three surgeons from Harvard University, concluded….
“The mortality rate of ELHR was 1.4%. The annual probability of developing acute symptoms requiring emergency surgery with the WW strategy was 1.1%. If ELHR is routinely recommended, it would be more beneficial than WW in fewer than one of five patients. WW is a reasonable alternative for the initial management of patients with asymptomatic or minimally symptomatic paraesophageal hernias, and even if an emergency operation is required, the burden of the procedure is not as severe as was thought in the past.“
In most cases, following a WHOLE-BODY HEALTH PROTOCOL is going to help with the chief symptom of Hiatal Hernia; GERD or acid reflux. If you do end up needing a surgery, always go into that surgery PREPPED AND READY. Oh, and if you are enjoying the mountains of free information on our site, be sure to pass it on to those you love and care about most. Sure you could just send a link. But it’s easier to simply like, share or follow on FACEBOOK!

4 Responses
what about some discomfort in right breast Not always just sometimes. Dose taking prozale cause this or is it the same thing i am feeling
when i have pain from the hernia?
Hi Mary, did you ever get a response to this? I am curious too.
That is a side-effect, but impossible for me to say in your particular case. Sincerely, Dr. Russ
Is there a connection with the psoas muscle?