CHRONIC NECK PAIN: THREE DECADES OF RESEARCH STUDIES ON FORWARD HEAD POSTURE (FHP)

“Neck pain accounts for 15% of all soft tissue problems seen in general practice.” From the October 2013 issue of the Journal of Clinical and Diagnostic Research.
“Most attempts to correct posture are directed toward the spine, shoulders and pelvis. All are important, but, head position takes precedence over all others. The body follows the head. Therefore, the entire body is best aligned by first restoring proper functional alignment to the head.” Dr. Rene Cailliet from 1987’s Rejuvenation Strategy
“Despite considerable evidence that posture affects physiology and function, the significant influence of posture on health is not addressed by most physicians. In fact, neither comprehensive postural nor structural evaluation is a routine part of training in physical diagnosis, and most osteopathic physicians do not describe postural/spinal mechanics in their usual patient evaluations.
Observation of the striking influence of postural mechanics on function and symptomatology have led to our hypothesis that posture affects and moderates every physiologic function from breathing to normal hormonal production. Spinal pain, headache, mood, blood pressure, pulse, and lung capacity are among the functions most easily influenced by posture.
The most significant influences of posture are upon respiration, oxygenation, and sympathetic function. Ultimately, it appears that homeostasis and autonomic regulation are intimately connected with posture.” Taken from the January 1994 issue of the AJPM (American Journal of Pain Management). Dr. Norman Shealy of Springfield, MO (M.D. / Ph.D / neurosurgeon) was a co-author of this study.
“The observation of the influence of postural mechanics on physiologic functions and pain has led researchers to conclude that posture plays a significant role in the development of pain and is critical to pain management. The most significant influences of posture are upon respiration, oxygenation, and sympathetic function, which is a major component of perceived pain.
Ultimately, it appears that homeostasis and autonomic regulation are intimately connected with posture. Many symptoms, including pain, may be moderated or eliminated by improved posture.” From the April, 2011 issue of the journal Practical Pain Management (The Role of Body Posture In Musculoskeletal Pain Syndromes)
“Forward head posture is a clinical entity that has been identified by multiple authors as a significant factor in a variety of musculoskeletal pain syndromes. Although some reports are essentially anecdotal, several reports use sophisticated statistical analyses and healthy controls versus painful subjects to establish forward head posture as a real clinical entity with significant musculoskeletal consequences.” Drs. Seaman and Troyanovich from the April 2000 issue of Dynamic Chiropractic (The Forward Head Posture). Dr. Seaman is a Functional Neurologist, for whom I have covered many articles (HERE).
It’s not really news that posture is important. And no posture carries worse connotations than that known as Forward Head Posture (FHP) and sometimes referred to as head forward posture — the posture where the head and shoulders are slouched / slumped forward. Not only does this posture look terrible, the implications for your health are far worse than you could have imagined. And none of this is new information. Over sixteen years ago, the March 2000 issue of the Mayo Clinic Health Letter said that, “long term forward posture leads to muscle strain, disc herniations and pinched nerves.” But it goes back much farther than this. The concept of Forward Head Posture was first proposed by the venerable Rene Cailliet over sixty years ago.
Dr. Cailliet (1917-2015) was a giant in the orthopedic rehab community, actually creating the field known today as Physical Medicine and Rehabilitation. Over the course of his long and illustrious career at both USC and UCLA, he authored books on WHIPLASH, NECK PAIN, SHOULDER PROBLEMS, CHRONIC PAIN, and SOFT TISSUE INJURIES. He was also a pioneer in postural research. It was Cailliet who said that…..
“Head in forward posture can add up to thirty pounds of abnormal leverage on the cervical spine. This can pull the entire spine out of alignment. Forward head posture (FHP) may result in the loss of 30% of vital lung capacity. These breath-related effects are primarily due to the loss of the cervical lordosis, which blocks the action of the hyoid muscles, especially the inferior hyoid responsible for helping lift the first rib during inhalation.”
He even talked about the fact that one’s “GUT” (“Gastrointestinal System”) could be irritated by Forward Head Posture to the point of actually diminishing bowel function. Of course this is nothing new to chiropractors (HERE), but for the medical community to be making these sorts of correlations between the function of the organs and the structure / function of the musculoskeletal system is amazing — particularly the fact that it happened decades ago.
One of the books that was required reading back in my time in Chiropractic College was Dr. I.A. Kapandji’s Physiology of Joints. It was Kapandji who said that, “for every inch of forward head posture, it can increase the weight of the head on the spine by an additional 10 pounds.” Think about this for a moment. The average person has at least an inch or so of FHP, and with people spending their lives online staring at their smart phones and computer screens, it’s not uncommon to see people with as much as 3 or 4 inches of Forward Head Posture. As you will now see, the implications are staggering.
We cannot leave our introduction without mentioning Dr. Vladimir Janda and his “UPPER CROSS SYNDROME“. Like my FATHER IN LAW, in his youth, Janda (from Czechoslovakia) had developed Polio and the complications that went along with it. This drove him to find therapeutic solutions not only for post-polio syndrome, but a wide array of other musculoskeletal problems as well. As both a neurologist and physiatrist, as well as an author, teacher, and researcher, even long after his death in 2002, Dr. Janda’s work remains iconic in the field of postural rehabilitation.
FORWARD HEAD POSTURE AND CHRONIC NECK / UPPER BACK PAIN
What is the number one reason people come see me? That’s easy; pain. Chronic Pain— the sort of pain that you can’t get away from; the kind of pain that makes you understand how a wild animal could chew off its own leg to get out of a trap — is a huge motivator. Let me show you some of the studies that directly relate Forward Head Posture to pain and DIMINISHED CERVICAL ROM. Believe me when I tell you that these are only the tip of the iceberg (all conclusions are cherry-picked due to constraints on time and space). The first thing I want you to notice is that this is not a new concept.
- 24 years ago, a 1992 is of the journal Physical Therapy carried a study called Incidence of Common Postural Abnormalities in the Cervical, Shoulder, and Thoracic Regions and their Association with Pain in Two Age Groups of Healthy Subjects. In this study they divided people into two groups; those with pain and those without pain. Another group of researchers then studied their posture, not knowing which group they had been put into. “Subjects with more severe postural abnormalities had a significantly increased incidence of pain…. Subjects with kyphosis [hump back] and rounded shoulders had an increased incidence of interscapular pain, and those with a forward-head posture had an increased incidence of cervical, interscapular, and headache pain.“
- In 1995, the Journal of Orofacial Pain published a study called The Relationship Between Forward Head Posture and Temporomandibular Disorders. They determined that, “The only measurement that revealed a statistically significant difference was angle ear-seventh cervical vertebra-horizontal plane. This angle was smaller in the patients with temporomandibular disorders than in the control subjects. In other words, when evaluating the ear position with respect to the seventh cervical vertebra, the head was positioned more forward in the group with temporomandibular disorders than in the control group.“
- A Y2K study published in the Indian Journal of Environmental and Occupational Medicine (Forward Head Posture is the Cause of ‘Straight Spine Syndrome’ in Many Professionals) revealed something I have been harping about for two and a half decades. Nearly 400 people of numerous different professions, all with neck pain, were studied to see how much kyphotic distortion (a stooped forward posture) was par for their particular profession. After having their necks X-rayed, they were given, “exercise therapy and conditioning of affected musculature.” According to the researchers, “All the subjects had radiological loss of normal lordosis of cervical spine (straight spine) but reported as normal radiographs. On clinical examination, all of them had tender trigger points over trapezius, and other muscles of the neck. The common postural defect in all the subjects observed was the forward-head posture. Seventy eight percent of them got relieved of symptoms, and 67 percent of them attained their normal lordotic curvature of the cervical spine within 6 months. Forward head posture is the commonest defect found in variety of professionals. This leads to Straight Spine Syndrome, an early functional stage, and can lead to serious compression of cervical nerve roots.” All this in people who were told by their physician that their X-rays were either “normal” or showed a bit of arthritis.
- In 2004, the Journal of the American Geriatric Society published a study called Hyperkyphotic Posture Predicts Mortality in Older Community-Dwelling Men and Women. In this fascinating piece of research, the authors looked at nearly 1,400 older folks (both men and women) who were being seen specifically for OSTEOPOROSIS. To measure how bad the kyphosis (stooped forward posture) was, they had the participants lay on their backs, while determining how many pillow blocks they had to put under the backs of their heads to get them to a neutral position. Listen to these shocking conclusions. “Hyperkyphotic posture was more common in men than women. In age- and sex-adjusted analyses, persons with hyperkyphotic posture had a 1.44 (144%) greater rate of mortality. In multiply adjusted models, the increased rate of death associated with hyperkyphotic posture remained significant. In cause-specific mortality analyses, hyperkyphotic posture was specifically associated with an increased rate of death due to atherosclerosis.” Not surprisingly, since my days in school I have heard it said that the top predictor of whether or not a person has hardening of the arteries is how stooped (humped) they are.
- A 2006 issue of Cephalalgia: An International Journal of Headache carried a study called Myofascial Trigger Points, Neck Mobility and Forward Head Posture in Unilateral Migraine. In this study, the authors determined that, “Migraine subjects showed a smaller cranio-vertebral angle than controls, thus presenting a greater FHP. Neck mobility in migraine subjects was less than in controls only for extension [this is your ability to tip your head backward]. However, there was a positive correlation between the cranio-vertebral angle and neck mobility [less CV angle means more FHP]. Nociceptive inputs [pain] from Trigger Points in head and neck muscles may produce continuous afferent [sensory] bombardment of the trigeminal nerve nucleus caudalis and, thence, activation of the trigeminovascular system [can anyone say “Trigeminal Neuralgia” AKA “Suicide Disease”?]. Active Trigger Points located ipsilateral [same side] to migraine headaches might be a contributing factor in the initiation or perpetuation of migraine.“
- In 2005, the Journal of Manipulation and Physiologic Therapeutics (JMPT) carried a study called Determining the Relationship Between Cervical Lordosis and Neck Complaints. In this study the authors looked at nearly 300 lateral cervical X-rays that had been divided into two categories — they either came from individuals who had neck pain or individuals that did not. The study, “found a statistically significant association between cervical pain and lordosis of less than 20 degrees, and a ‘clinically normal’ range for cervical lordosis of 31 degrees to 40 degrees. Maintenance of a lordosis in the range of 31 degrees to 40 degrees could be a clinical goal for chiropractic treatment.” Considering that the average person has no curve (or maybe even a reversed curve), this is a lofty goal. There is only one way to get there from here, which I will cover shortly.
- In 2006, the journal Headache published a study called Trigger Points in the Suboccipital Muscles and Forward Head Posture in Tension-Type Headache. The authors concluded that, “Suboccipital active trigger points and FHP were associated with chronic tension-type headache. Chronic tension-type headache subjects with active trigger points reported a greater headache intensity and frequency than those with latent trigger points. The degree of FHP correlated positively with headache duration, headache frequency, and the presence of suboccipital active trigger points.” This is why when it comes to TRIGGER POINTS, I am a stickler for getting your body into extension (more to come in a bit).
- A 2008 Chinese study that was published in Manual Therapy (The Relationship Between Head Posture and Severity and Disability of Patients with Neck Pain) measured FHP by looking at something they called the CV Angle. They concluded that, “The CV angle in subjects with neck pain is significantly smaller than that in normal subjects. Patients with small CV angle have a greater forward head posture, and the greater the forward head posture, the greater the disability.” We are not just talking pain here folks, we are talking pain severe enough to cause disability. Believe me when I tell you that the Chinese definition of disability is different than our definition over here.
- The April 2009 issue Archives of Physical Medicine and Rehabilitation (Head Posture and Neck Pain of Chronic Nontraumatic Origin: A Comparison Between Patients and Pain-Free) concluded that, “Younger patients with chronic nontraumatic neck pain were shown to have a more forward head posture in standing than matched pain-free participants.” It’s a theme we will see over and over again. Why? No one uses technology (computers, phones, video games, etc) more than young people.
- In June 2009, the Chinese journal Zhongguo Yi Xue Ke Xue Yuan Xue Bao carried a study called Association Between Cervical Curvature and Cervical Sympathetic Symptoms. In this study, the authors were trying to asses the relationship between the neck curvature of post-surgical patients and the propensity to develop something called SYMPATHETIC DOMINANCE. The authors concluded that, “The incidence of abnormal cervical curvature in the group with cervical sympathetic symptoms was 67.6%, which was significantly higher than that in group without cervical sympathetic symptoms (50.7%). Cervical curvature abnormality may be an independent factor that affects cervical sympathetic [dominance].“
- It’s not just physicians, chiros and therapists that are talking about this phenomenon of FHP. In early September of 2009, the Institute of Electrical and Electronics Engineers / Engineering in Medicine and Biology Society (IEEE EMBS) held their 31st annual meeting in Minneapolis, MN. One of the statements that came out of that meeting was that, “Over time poor posture results in pain, muscle aches, tension and headache and can lead to long term complications such as osteoarthritis. Physiological and biomechanical stress due to sustained postures limit important musculoskeletal stimuli that are essential for normal musculoskeletal development.“
- Later in 2009, the Journal of Orthopedics and Sports Physical Therapy looked at the relationship between Forward Head Posture and CARPAL TUNNEL SYNDROME (Increased Forward Head Posture and Restricted Cervical Range of Motion in Patients with Carpal Tunnel Syndrome). While careful not to declare causation, the authors determined that, “Patients with Carpal Tunnel Syndrome had a smaller craniovertebral angle (greater FHP) than controls in both standing and sitting. Additionally, patients with Carpal Tunnel Syndrome showed decreased cervical range of motion in all directions when compared to controls. A positive association between FHP and cervical range of motion was identified in both groups: the smaller the craniovertebral angle (reflective of a greater FHP), the smaller the range of motion. Patients with mild/moderate carpal tunnel syndrome exhibited a greater FHP and less cervical range of motion, as compared to healthy controls. Additionally, a greater FHP was associated with a reduction in cervical range of motion.“
- The April 2012 issue of Clinical Rehabilitation (The Efficacy of Forward Head Correction on Nerve Root Function and Pain in Cervical Spondylotic Radiculopathy) looked at the effect of Extension Therapy (restoration of the normal lordotic cervical curve) in people with SPINAL DEGENERATION causing pinched nerves in their neck, which resulted in pain running down an arm. Check this out. “Forward head posture correction using a posture corrective exercise programme in addition to ultrasound and infrared radiation decreased pain and craniovertebral angle and increased the peak-to-peak amplitude of dermatomal somatosensory evoked potentials for C6 and C7 in cases of lower cervical spondylotic radiculopathy.” In other words, these people did not simply feel better after improving their FHP, they were better according to electronic diagnostic testing (EMG).
- The February 2013 issue of Manual Therapy (Effects of Thoracic Kyphosis and Forward Head Posture on Cervical Range of Motion in Older Adults) determined that, “Greater thoracic kyphosis [a stooped forward posture] was significantly associated with lesser CVA [more Forward Head Posture] whereas greater CVA [less Forward Head Posture] was significantly associated with greater cervical flexion and general rotation ROM…. Analyses, adjusted for age, gender, weight and NDI, revealed significant indirect effects of thoracic kyphosis on cervical flexion and general rotation ROM through FHP. Our results show that FHP mediated the relationship between thoracic kyphosis and cervical ROM, specifically general cervical rotation and flexion. These results not only support the justifiable attention given to addressing FHP to improve cervical impairments, but they also suggest that addressing thoracic kyphosis impairments may constitute an “upstream” approach.“
- Pay attention to this December 2013 study (Musculoskeletal Physical Outcome Measures in Individuals with Tension-Type Headache) published in the journal Cephalalgia: An International Journal of Headache. The authors admit that even though, “Individuals with tension-type headache, in addition to headache pain, typically suffer from pericranial muscle tenderness and increased cervical muscle tone,” these findings are typically ignored in favor of crappy but common diagnostic tests such as MRI. Listen carefully as they reveal the brutal truth about said tests. “Physical and physiological outcomes related to musculoskeletal function are not commonly assessed in clinical studies and not systematically proposed as outcome measures in headache-related practice guidelines.” After reviewing hundreds of studies, “Twenty-six studies met selection criteria. Physiological outcomes typically reported in laboratory studies were trigger points, pressure pain threshold, range of motion and tenderness. A greater number of trigger points and lower pressure pain threshold were reported in patients with episodic tension-type headache in comparison with healthy subjects. Individuals with chronic tension-type headache, when compared with non-headache controls, consistently showed a greater number of trigger points, a lower value of pressure pain threshold and a more severe forward head posture. Musculoskeletal outcomes, such as trigger points, pressure pain threshold and forward head posture should inform tension-type headache pathophysiology, diagnosis and interdisciplinary patient care.” In other words, it’s no longer acceptable (as if it ever was) to simply run tests and prescribe drugs ad infinitum. But that is exactly what is still taking place today. It’s all because of that crazy CANYON.
- In the SUMMER OF 2014, the Brazilian Journal of Physical Therapy (Cervical and Shoulder Postural Assessment of Adolescents Between 15 and 17 Years Old and Association with Upper Quadrant Pain) looked at the relationship between Forward Head Posture and upper body pain. The authors concluded that, “Forward head and protracted shoulder are common postural disorders in adolescents, especially in girls. Neck pain is prevalent in adolescents, especially girls, and it is associated with forward head posture.“
- The December 2014 issue the the Annals of Rehabilitation Medicine (Radiologic Assessment of Forward Head Posture and its Relation to Myofascial Pain Syndrome) cut straight to the chase. After comparing X-rays of those with pain to those without, they determined that, “Forward head posture and reduced cervical lordosis were seen more in younger patients with spontaneous neck pain.“
- Just last year, the International Journal of Occupational Medicine and Environmental Health looked at the relationship to neck pain and Forward Head Posture (The Study of Correlation Between Forward Head Posture and Neck Pain in Iranian Office Workers). The authors concluded that, “office employees had a defective posture while working and that the improper posture was more severe in employees who suffered from neck pain.” What do office workers typically do all day long? They stare (down down down down down) at their computer screens.
- And finally, a few months ago the January issue of the Journal of Physical Therapy Science carried a study called Clinical Effects of Deep Cervical Flexor Muscle Activation in Patients with Chronic Neck Pain. The authors determined that, “Deep Cervical Flexor activation exercise was effective to alleviate pain, recover functions, and correct forward head posture in the patients with neck pain.“
Posture has a huge relationship to balance, and proprioception as well. When the vertebrae in your neck are either misaligned in relationship to each other (SUBLUXATION or POOR POSTURE) or are not moving freely on each other, the result will always be a loss of proprioception. PROPRIOCEPTORS (aka mechanoreceptors) sense things like stretch, pressure, tension, compression, and actually feed more information to your brain about balance than your vestibular system (inner ear).
When your joints don’t work right, your proprioception doesn’t work right either. Although there are any number of consequences of this (see previous link) the end result is always DEGENERATION. But remember that FHP is not only about musculoskeletal symptoms.
This concept was cemented by a 2012 study published in the Annals of Rehabilitation Medicine called The Effect of The Forward Head Posture on Postural Balance in Long Time Computer Based Worker. The authors concluded that,
“Group One (work with computers for over 6 hrs per day) had a relatively more protruded head with extensive neck posture. The center of gravity of group I tended more toward the anterior than that of group II (rarely work with computers). Postural imbalance and impaired ability to regulate movement in forward and backward direction were also found. The results of this study suggest that forward head postures during computer-based work may contribute to some disturbance in the balance of healthy adults. These results could be applied to education programs regarding correct postures when working at a computer for extended periods of time.”
Stay tuned because I am going to give you my number one tricks for helping you if you spend lots of time at a computer.
Furthermore, in searching the peer-reviewed literature for this post, I found that Forward Head Posture is intimately related to any number of health problems. Not surprisingly I found numerous studies linking increased FHP to a decreased ability to breathe (including ASTHMA). But there were other studies as well — studies on athletic performance, one’s ability to sing, BLOOD PRESSURE, DIGESTION, and any number of others.
There are even studies linking happiness and self esteem to posture. For instance, a 2011 issue of the journal Procedia: Social and Behavioral Sciences (Relationship of Self Esteem with Forward Head Posture and Round Shoulder) actually explored this link, as did a 2009 study published in the European Journal of Social Psychology (Body Posture Effects on Self-Evaluation).
And finally, for my good friend Jack — a 20 year Navy combat helicopter pilot who now flies for Air Evac — a study just for you. One of the things I’ve learned from Jack in the years since his combat flying is that due to the added weight of the night vision, targeting devices, navigation, and other electronic equipment, the helmets worn by today’s combat pilots are heavy — really heavy. This added weight dramatically increases the mechanical loading of the cervical spine that occurs in combat.
Case in point, a study from the September 2012 issue of the Journal of Biomechanics (Simulation of the Effects of Different Pilot Helmets on Neck Loading During Air Combat). “New generation pilot helmets with mounted devices enhance the capabilities of pilots substantially. However, the additional equipment increases the helmet weight and shifts its center of mass forward.” Forward???? Can anyone say FHP? When you read the next paragraph Jack, think of yourself in relationship to the “T1-C7 level” (lower neck / upper back) area that has been your “spot” for as long as I’ve known you.
“The increased weight and the forward shift of the center of mass of a new generation helmet lead to higher muscle activations and higher joint reaction loads over a wide range of head and neck movements. The muscle activations required to balance the head and neck in extreme postures increased the compressive force at the T1-C7 level substantially… The lateral neck muscles can reach activations of 100% and cause compressive joint forces up to 1100N during extensive rotations and extensions at high ‘vertical’ accelerations.”
WHAT CAN I DO TO HELP SOLVE MY FORWARD HEAD POSTURE?
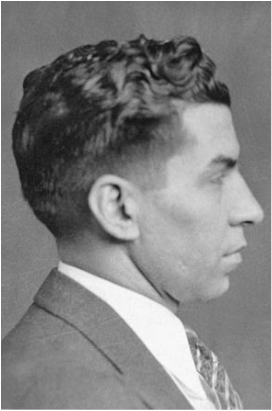 LUCKY LUCIANO: 1931 GOOD POSTURE | 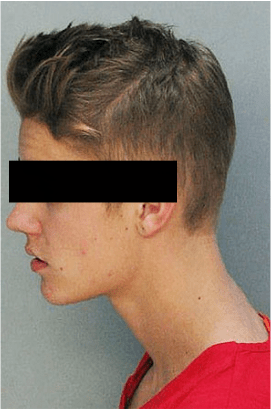 THE UNKNOWN CELEB: 2014 FORWARD HEAD POSTURE |
As a Chiropractor, my first question is which con above has the better hair; Luciano on the left, or the “unknown celebrity” on the right? Secondly, I want to know if the scientific literature has anything to say about adjustments being able to help structurally change Forward Head Posture. Last May’s issue of the Journal of Physical Therapy Science addressed this issue in a study called The Effects of Cervical Joint Manipulation, Based on Passive Motion Analysis, on Cervical Lordosis, Forward Head Posture, and Cervical ROM…..
In this study, they not only quoted from previous studies on the effectiveness of various Chiropractic techniques, but concluded that, “manipulation three times a week for four weeks… was effective in increasing the cervical lordosis, cervical extension ROM, and ranges of flexion and extension motion, and in decreasing FHP.” Below are some more posts on this topic.
- REVERSE CERVICAL CURVES
- WHIPLASH & THE REVERSE CERVICAL CURVE
- THE LINK BETWEEN CHRONIC NECK PAIN, LOSS OF THE CERVICAL CURVE, AND SPINAL DEGENERATION
- CHRONIC NECK PAIN AND THE RELATIONSHIP TO NECK EXERCISES / NECK STRETCHES
- SOLVING CHRONIC NECK PAIN: PHASE I
- SOLVING CHRONIC NECK PAIN: PHASE II
- TRIGGER POINTS, CHRONIC PAIN, AND THE REVERSE CERVICAL CURVE
When it comes to the Chiropractic technique best suited for restoring normal cervical curves, hands down it’s CBP (Chiropractic Bio-Physics). Interestingly enough, every CBP practitioner I’ve ever met, readily admits that adjustments alone are not enough to restore the proper curvature to the cervical spine. There will need to be some sort of EXTENSION THERAPY.
I do not do any of this “in house,” choosing instead to have the patients do it at home. My go-to tool is the DAKOTA TRACTION DEVICE. I love it because it’s super cheap, super easy to use, and it’s safe —- and most importantly, it works well for most people (I have a “floor model” I use to show people how it works, and to see if they can tolerate extension — just make sure you are SPENDING ENOUGH TIME IN EXTENSION TO MAKE CORRECTION).
Beyond the stretching of the SCM’s, PLATYSMA, and other muscles that the Dakota Traction Device will help you accomplish, you’ll need to do some exercises to strengthen your neck muscles. HERE is a picture of all of it put together.
If you are interested in looking at some studies that are directly related to reversing Forward Head Posture and helping restore one’s normal curve via neck stretches and exercises, PubMed is a great starting point. I found numerous studies, including one showing that restoration of the neck’s normal curve helps those dealing with sciatica due to degenerative lumbar (low back) discs.
The March 2015 issue of JMPT published a study whose conclusions stated, “The addition of forward head posture correction to a functional restoration program seemed to positively affect disability, 3-dimensional spinal posture parameters, back and leg pain, and S1 nerve root function of patients with chronic discogenic lumbosacral radiculopathy [sciatica due to spinal degeneration].“
As is always the case, never leave out dealing with inflammation. Lots of people are willing to deal with the biomechanical aspect of their pain, but are either not willing or simply not informed, when it comes to taking care of the underlying INFLAMMATORY PROCESS (I actually talked about this the other day — HERE). This is critical to understand not only from the perspective of pain, but because Inflammation always leads to Fibrosis / Scar Tissue (HERE).
A WEIRD LITTLE TRICK FOR HELPING MAINTAIN GOOD NECK CURVATURE EVEN THOUGH YOU SPEND YOUR LIFE IN FRONT OF A COMPUTER
Set your screen (monitor) up slightly higher than eye level (a box, a shelf, a small cabinet, etc should do the trick) you can actually induce some lordotic curve into the neck while you work and prevent the “slump” or heightened kyphosis in the mid back. I started doing this a few years ago and the difference to my CHRONIC UPPER TRAP TRIGGER POINTS has been significant.
