ARE YOUR HEARTBURN MEDS DESTROYING THE HEALTH OF YOUR GUT?
“In most hospitals, intravenous PPIs are routinely ordered for any patient who is not taking food or drink by mouth. There is not one shred of evidence that PPIs are indicated in this setting. Of course, PPIs are available over the counter (OTC) now, and although they are meant to be taken for only 3 weeks at a time and for no more than 3 such courses per year, there is really no limit to the number of PPIs purchased and used. I have no idea how to stop the wholesale use of PPIs by primary care MDs, gastroenterologists and people who self-medicate. It may be hopeless.”Cherry-picked (as are all quotes) from the June 26, 2012 Skeptical Scalpel blog over at Physicians Weekly. The author of this article (Overuse of Proton Pump Inhibitors is Expensive & Dangerous) is an anonymous surgeon.
“PPI prescribing rates among inpatients are high, and frequently not evidenced-based. There is also lack of consideration given to review of therapy and limiting provision to short courses. Proton pump inhibitors (PPIs) are widely used but commonly over-prescribed. A range of adverse effects are associated with their use, including susceptibility to C. difficile infection, fractures, pneumonia and electrolyte disturbances.” From the abstract of a 2014 issue of the medical journal Gut (Overuse Of Proton Pump Inhibitors And Strategies To Reduce Inappropriate Prescribing). This is yet another area where the medical community seems to be throwing the “EVIDENCE” out the window.
“As many as 70 per cent of PPI prescriptions in the United States have been inappropriately handed out by doctors, according to a study published in January in the journal JAMA Internal Medicine. German researchers found that people 75 or older who regularly take the medications had a 44 per cent increased risk of dementia, compared with seniors not using the drugs.” From the Feb 16, 2016 issue of CBCNews (Proton Pump Inhibitor Heartburn Drugs Linked to Dementia Risk)
“Proton-pump inhibitors (PPIs) are often given prophylactically to hospitalized patients even though they are known to increase the risk of serious conditions such as Clostridium difficile infection, osteoporosis, pneumonia, and more. Many patients are also on unneeded PPIs before they enter and after they leave the hospital, putting them at even greater risk of complications.” From the March 2016 issue of AHC Hospitalist (Reducing Unnecessary PPI Use May Help Save Lives)
“How VA patients are treated, — or potentially overtreated, — for gastroesophageal reflux disease (GERD) is coming under greater scrutiny. Veterans often are prescribed proton pump inhibitors (PPI) at much higher doses than recommended, then kept on the drugs far too long, according to the VA-funded study released this year.” From the May 2013 issue of U.S Medicine: The Voice of Federal Medicine (VA’s Overuse of GERD Treatment Under Scrutiny)
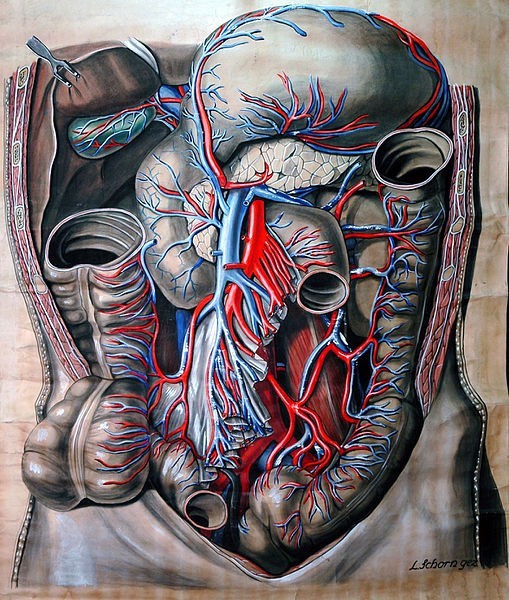
I’ve shown you (HERE) that not only is having lots of very strong stomach acid critical for your digestive health, it’s one of the primary barriers your body throws up against microbial invasion as well. Plainly stated, most bacteria have trouble thriving in a highly acidic environment such as the stomach should be. This is why among the NUMEROUS SIDE EFFECTS associated with Proton Pump Inhibitors (heartburn drugs otherwise known as PPI’S), one of the most common is Dysbiosis.
DYSBIOSIS is the name given to the condition of having incorrect ratios of bacteria in the Gut. Although it is way oversimplified, it is what happens when you have too many bad bacteria and not enough good (be aware that too many of a specific type of “good” bacteria can create Dysbiosis as well (HERE). Historically the medical community has not had much to say about Dysbiosis in its various forms (SYSTEMIC YEAST and C. DIFF are two common ones) because for the most part they are responsible for causing it. How? Through out-of-control prescription habits concerning ANTIBIOTICS. Once people have Dysbiosis it is fed by over-consuming sugar and starch (HERE). When you consider that 80% of your entire Immune System is made up of cells found in your Gut — much of it in the form of bacteria — you can begin to see how big this problem can potentially be. Allow me show you some studies.
- It’s not brand new news that PPI’s mess up GUT HEALTH. A November 2014 study in the journal Microbiome (Prolonged Use of a Proton Pump Inhibitor Reduces Microbial Diversity….) concluded that, “The role of the gut microbiome in arresting pathogen colonization and growth is important for protection against Clostridium difficile infection (CDI). Observational studies associate proton pump inhibitor (PPI) use and CDI incidence……. Our hypothesis that PPIs disrupt the healthy human gut microbiome is supported in this group. We conclude that decreases in observed species counts were reversible after cessation of PPI usage within 1 month. This finding may be a potential explanation for the association between prolonged PPI usage and CDI incidence.” The problem is that people are not using their PPI’s for one month (even though the box says no longer than two weeks). They are using them for years — even decades. Interestingly enough, two months prior to this, Obesity Surgery carried a study that concluded almost the same thing — only in individuals who had undergone lap band surgery for weight loss (those on PPI’s had significantly more trouble losing weight).
- What is the mechanism for this phenomenon? Not surprisingly, INFLAMMATION. Last August’s issue of the Journal of Infectious Diseases (Proton-Pump Inhibitor Exposure Aggravates Clostridium difficile-Associated Colitis) had this to say on the subject. “Clostridium difficile is currently the leading cause of infectious diarrhea in hospitalized patients. A mouse model of antibiotic-associated clostridial colitis was established to examine the role of PPIs for CDI. Mice with CDI that were exposed to PPI exhibited greater losses of stool consistency and body and cecal weights than those that were not exposed to PPI. Further, more neutrophilic infiltrations, epithelial damage, and inflammatory cytokine expression were noted in colon specimens of the mice with PPI exposure. More-evident inflammatory responses were detected by in vivo imaging of NF-κB reporter mice with CDI that were exposed to PPI. Gut barrier permeability was increased to a greater extent…… Our mouse model demonstrates that PPI exposure increases the severity of intestinal inflammation in mice with C. difficile-associated colitis.” Did you catch the “GUT PERMEABILITY” thing (Leaky Gut Syndrome)? Once again folks, we see Inflammation at the root of the problem — in this case being driven by the very meds used to “cure” people — not as uncommon as you might believe (HERE).
- Two months later, the October 2015 issue of PLoS One (Reduced Gut Acidity Induces an Obese-Like Phenotype in Drosophila Melanogaster and in Mice) related PPI’s not only to Dysbiosis, but to OBESITY as well. “….This deficit is likely to induce altered metabolism and contribute to accelerated aging, since vha16-1 mutant flies are short-lived and display increases in body weight and lipid [fat] accumulation. Similar phenotypes were also induced by pharmacological treatment, through feeding normal flies and mice… proton pump inhibitor (PPI, lansoprazole) to suppress gut acid production. Our study may thus provide a useful model for investigating chronic acid suppression in patients.” These findings are not surprising knowing what we know about the relationship between Obesity and Gut Health (HERE, HERE, and HERE are some relevant examples).
- A month after this, the November 13 issue of Clinical Correlations (Are We Overusing Proton Pump Inhibitors?) revealed that, “Proton pump inhibitors (PPIs) are one of the most widely used medications in the US. Last year, esomeprazole was ranked as one of the top three best-selling drugs in the nation, with 17.8 million prescriptions. Physicians use empiric PPI therapy to diagnose GERD, one of the most common gastrointestinal diseases. If symptoms improve with empiric therapy, PPIs are then continued, often indefinitely. However, PPI use can have potentially serious medical consequences, including an increased risk of infections, malabsorption, and adverse drug-drug interactions. Prolonged PPI use can have serious infectious risks. Reduced acid production due to PPIs compromises the sterility of the gastric lumen, thus making it easier for pathogens to colonize the upper gastrointestinal tract and subsequently alter the colonic microbiome. The best-documented enteric infection linked to PPI use is Clostridium difficile, which is the leading cause of gastroenteritis-associated death in the US.“
- More recently (this month, May of 2016) we were hit with it again. The journal Gut carried a study aptly named Proton Pump Inhibitors Affect the Gut Microbiome. Their conclusions are interesting on many levels; especially considering there are other “things” (drugs / vaccines) that can also affect the Microbiome. In fact, I wrote about one of them just the other day (HERE). But I regress. This study concluded that, “Proton pump inhibitors (PPIs) are among the top 10 most widely used drugs in the world. PPI use has been associated with an increased risk of enteric infections, most notably Clostridium difficile. The gut microbiome plays an important role in enteric infections, by resisting or promoting colonization by pathogens. PPI use is associated with a significant decrease in Shannon’s diversity and with changes in 20% of the bacterial taxa. The differences between PPI users and non-users observed in this study are consistently associated with changes towards a less healthy gut microbiome. These differences are in line with known changes that predispose to C. difficile infections and can potentially explain the increased risk of enteric infections in PPI users. On a population level, the effects of PPI are more prominent than the effects of antibiotics or other commonly used drugs.” This last sentence is hugely important, as historically CDI was virtually always associated with Antibiotics. In other words, if you are one of the millions of Americans taking a PPI and happen to go on Antibiotics, your odds of screwing up your Gut increase dramatically.
- Not to be outdone, this month’s issue of Alimentary Pharmacology & Therapeutics said almost the same thing in a study called A Comparison of the Gut Microbiome Between Long-Term Users and Non-Users of Proton Pump Inhibitors. “Proton pump inhibitor (PPI) use is associated with an increased risk of Clostridium difficile infection (CDI). We used a population-based database to identify individuals with 5 or more years of continuous PPI use along with non-PPI using controls. Stool samples were subjected to microbiological analysis…. Long-term PPIs use has an effect on the gut.“
Hopefully this post has left you wanting to get off of your PPI drugs. Although I would certainly recommend that you talk to your doctor about this, as you can tell from some of the quotes at the top of the page, they are not always as helpful as you think they should be. Thus, make sure to go back up to the first two links in this post and read them. They will show you that everything you thought you knew about your chronic heartburn is probably wrong, and probably helping perpetuate the problem.
