MOST DISEASES ARE JUST DIFFERENT MANIFESTATIONS OF THE SAME THING (THE GUT-MICROBIOTA-BRAIN AXIS)
Yesterday I talked about the “COMMON CAUSE” of sickness and disease, discussing things like Leaky Gut Syndrome and similarly related Gut Dysfunctions. Let me blow your mind a bit by giving you a practical application using the example of the gut-microbiota-brain axis. Earlier this year, one of the journals put out by the American Heart Association (Circulation Research) published a mind-bending study called Hypertension Opens the Flood Gates to the Gut Microbiota, in which they stated….
“In two different animal models of hypertension, there is decreased expression of several tight junction proteins in the gut and a concomitant increase in intestinal permeability. Furthermore, their data show that in the spontaneously hypertensive rat model, the increase in permeability is a result of increased sympathetic nerve activity before the development of hypertension.
They therefore conclude that there is a direct, causal link between the sympathetic nerve activity derived from the central nervous system and increased gut permeability. They further hypothesize that the changes in gut permeability result in hypertension and cause a shift in the types of bacteria that are present in the gut. Finally, they have shown that the changes in sympathetic activity resulting in increased gut permeability are also associated with an increase in inflammatory cells within the intestinal wall.”
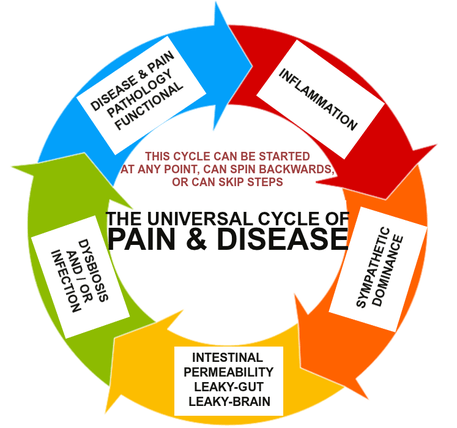
Catch what they are saying here (I have a very cool diagram I created down the page). Even though I had SYMPATHETIC DOMINANCE at the #4 position in my list from the link at the top of this page, the authors of this study — both cardiologists — are saying that it is actually the starting point. Furthermore, these changes in autonomic nervous system function lead to the INCREASED GUT PERMEABILITY (Leaky Gut Syndrome) that causes HIGH BLOOD PRESSURE. It’s the gut-microbiota-brain axis in action!
This is why I can say with authority that giving people high blood pressure medications is NOT ACTUALLY CHANGING HOMEOSTASIS, but instead covering the symptom (in this case, HBP) by forcing a short-term physiological change. How is this done? For starters, most people with hypertension are going to end up on drugs known as beta blockers.
Also known as beta-adrenergic blockers, these drugs block your adrenergic system. When you think adrenergic, think adrenaline. The thing to remember is that the medical community does not call adrenaline adrenaline any more, they call it by its other name, epinephrine. Whatever you decide to call it, when you block it, you block the sympathetic side (fight-or-flight) of the Autonomic Nervous System. While this will likely decrease your blood pressure, you automatically change the function of everything in your body (you slow it down).
While this might sound good on the surface (most health issues tend to hyper-stimulate the sympathetic side of the ANS), as you might imagine, the side effects of this drug (according to Mayo Clinic) frankly suck — tiredness, fatigue, weight gain, depression, and others. These authors also revealed that beta blockers actually increase your triglyceride levels, while decreasing your “good” cholesterol (HDL). Most people on these drugs complain of DIMINISHED LIBIDO as well.
The bottom line is that the drugs and vaccines we are consuming from cradle to grave, while in certain cases possibly adding years to our life, are not necessarily adding life to our years (HERE). To grasp what I am saying and how it’s intimately related to the gut-microbiota-brain axis, read between the lines of this study from the May 2013 issue of Trends in Neuroscience (Gut–Brain Axis: How the Microbiome Influences Anxiety and Depression).
“Within the first few days of life, humans are colonized by commensal intestinal microbiota. Here, we review recent findings showing that microbiota are important in normal healthy brain function…. the relation between stress and microbiota, and how alterations in microbiota influence stress-related behaviors. New studies show that bacteria, including commensal, probiotic, and pathogenic bacteria, in the gastrointestinal tract can activate neural pathways and central nervous system.”
What do we learn from the study’s abstract, that stress causes mental issues, and that mental issues cause stress (DEPRESSION falls under the massive category of “INFLAMMATORY DISEASE,” which is why SYMPATHETIC DOMINANCE always leads to some sort of stress — again, see link at top of page). Furthermore, with infants being “colonized” by mom’s good bacteria “Within the first few days of life,” should we be even slightly surprised that VACCINES given in these first few days can, in some cases, cause serious problems?
It helps explain why AUTISM is always concurrent with some sort of Gut / Bowel issue. Always. 100% of the time. Also be aware that what we are talking about today are “Axes,” and that an Axis cuts both ways (metabolic and neurological pathways are bidirectional). This is especially true of the gut-microbiota-brain axis.
Case in point is a study from a five year old issue of Psychoneuroendocrinology (Regulation of the Stress Response by the Gut Microbiota: Implications for Psychoneuroendocrinology), which shows that not only can inflammation cause Gut issues, Gut issues can cause stress, and stress causes inflammation (you could work it backwards as well). Mechanism? That durned leaky gut.
“Stress induces increased permeability of the gut allowing bacteria and bacterial antigens to cross the epithelial barrier and activate a mucosal immune response [inflammation], which in turn alters the composition of the microbiome and leads to enhanced HPA drive [HPA AXIS]. Increasing data from patients with irritable bowel syndrome and major depression indicate that in these syndromes alteration of the HPA may be induced by increased gut permeability.”
Here’s the crazy part of this. Give me ten minutes and I could show you a hundred studies showing the same thing (I’ll show you a few more momentarily).
Here’s what’s doubly crazy. If you you go back a century or so, you will find that there were many sanitariums (Clearview may have been the most well known) treating mentally ill people using CHIROPRACTIC ADJUSTMENTS as well as therapies like COLONIC IRRIGATION. Why? Firstly because the drugs for treating these conditions had not been invented yet (for instance, PEOPLE WITH SEIZURE DISORDERS WERE TREATED WITH KETOGENIC DIETS), and secondly, it worked. The adjustments (particularly UPPER CERVICAL SPECIFIC) toned down the sympathetic nervous system, thereby reducing inflammation; and the colonic irrigation worked to clean out the dysbiotic Gut.
All you have to do is look back at a 1932 issue of the New England Journal of Medicine to see an early example of leveraging the gut-microbiota-brain axis to treat mental illness (Colon Irrigation in the Treatment of Mental Disease). Furthermore, once you understand that about 90% of the body’s Serotonin and Melotonin are made in the Gut, this all begins to make more sense. But get ready because I am going to throw you a bit of a curve ball.
When people become inflamed, they end up with diseases on these two lists (HERE and HERE) as well as CHRONIC PAIN. Naturally, because their doctor, along with about a trillion TV commercials, told them drugs (medications) were the only way to roll, they tend to first reach for their medicine cabinet and pull out some OTC antiinflammatory medications.
Unfortunately, there are only about a jillion studies linking NSAIDS to intestinal permeability (Leaky Gut) — an almost universal component of chronic conditions and a great example of poor understanding of the gut-microbiota-brain axis. But they are not the only drugs that lead to Leaky Gut — not by a long shot.
Antibiotics always cause at least some degree of dysbiosis (HERE) — a problem that will always be found concurrently with increased intestinal permeability. Similarly, CORTICOSTERIDS — an extremely powerful class of anti-inflammation drugs — causes increased permeability as well, because they SUPPRESS THE IMMUNE SYSTEM. While this might not seem like a big deal on the surface, once you realize that 80% of your immune system is housed in your Gut, you can start to see the propensity for collateral damage.
And when we talk about AUTOIMMUNE DISEASES, no one can act shocked by the fact that extremely harsh chemotherapy drugs cause permeability as well (these include the “mab” class of biologics — monoclonal antibodies — used to treat autoimmune diseases). The truth is, in the same way that Dr. Art Ayers warned us years ago that all drugs have antibiotic properties (HERE), it is starting to appear that the same thing is true concerning intestinal permeability as well.
Other things that are known to cause intestinal permeability include coffee, GRAINS (yes, GLUTEN is a biggie, but any grain can be problematic), LECTINS, TOO LITTLE STOMACH ACID (far more common than the opposite), alcohol & SUGAR (they are metabolized along similar pathways and can both lead to dysbiosis and CANDIDA OVERGROWTHS — especially true of HFCS). If you have food allergies or PARASITES, you are at risk for increased permeability as well.
And here’s the rub.
Things that cause your Gut to become “Leaky” (increased permeability) have been shown by mountains of peer-review to cause other epithelial barriers to leak as well. These include, but are not limited to your brain (“Leaky Brain”), spinal cord (“Leaky Cord”), nervous system (“Leaky Nerve”), lungs (“Leaky Lung”), etc, etc, etc (HERE).
Oh, and for the record, to show you some of the evidence pointing to the fact that antidepressants themselves are likely contributing to the very issue that’s causing them in the first place — intestinal permeability — take a look at this study from the University of Michigan (Depression, Antidepressant Medications, and Risk of Clostridium Difficile Infection) that was published in BMC Medicine. A classic understanding of using pharmaceutical medications but not understanding how they affect the gut-microbiota-brain axis.
After looking at the medical records of nearly 17,000 individuals who had come down with C. DIFF, they determined that those with C. Diff were 37% more likely to have been diagnosed with Major Depression. “Our complementary studies reveal that adults with depression and those that use specific anti-depressants seem to be more likely to experience C. diff infections.” And we haven’t even touched on the fact that ALUMINUM also causes intestinal permeability — something we learned 20 years ago in a 1997 issue of the American Journal of Clinical Nutrition (Mechanisms of Aluminum Absorption…..).
The importance of knowing this comes into view when you realize just how much aluminum we (the American public) are being exposed to on a daily basis (see link). Interestingly enough, most SSRI ANTIDEPRESSANTS contain FLUORIDE — a toxic byproduct of the aluminum manufacturing process (i.e. Prozac’s official name is Fluoxetine).
THE GUT-MICROBIOTA-BRAIN AXIS: WHERE THE RUBBER MEETS THE ROAD FOR REAL HEALING!
“The CNS modulates the GI tract via the sympathetic and parasympathetic branches of the ANS, as well as the HPA axis. These influences can affect the microbiota indirectly by altering its environment and directly via a large number of signaling molecules. Both branches of the ANS regulate gut functions such as regional motility, secretion of acid, production of bicarbonates and mucus, maintenance of epithelial fluid, permeability of the intestine, and the mucosal immune response. The ANS also affects epithelial mechanisms involved in activation of the immune system by the gut.
For example, several preclinical studies have demonstrated that stressful stimuli can increase the permeability of the intestinal epithelium, facilitating translocation of luminal organisms [bacteria, yeast, virus, etc] and inducing an immune response in the intestinal mucosa. Current evidence suggests that multiple mechanisms, including endocrine and neurocrine pathways, may be involved in gut microbiota–to–brain signaling and that the brain can in turn alter microbial composition and behavior via the autonomic nervous system.
The gut microbiota appears to influence the development of emotional behavior, stress- and pain-modulation systems, and brain neurotransmitter systems.” Cherry-picked (as are most of the quotes I use) from the March 2015 issue of the Journal of Clinical Investigation (Gut/Brain Axis and the Microbiota)
If you did not grasp what this quote is really saying concerning the gut-microbiota-brain axis, go back and re-read it, as it gives you a “Big Picture” viewpoint of what you will see over and over again with any number of diseases. In other words, for the most part, diseases are simply different manifestations of the same basic pattern of aberrant physiology (I showed you this from a very cool OLD POST I totally reworked and put up on my Facebook Page just the other day).
Take a look at the circular diagram above. The order might change a bit (any one of these can cause or contribute to any other, and it might spin backwards, both directions at the same time, or skip steps), but the essentials are the same.
What you have to do is figure out how big a wrench it’s going to take to jam the gears and stop this vicious cycle. Remember, drugs might change your symptoms, but they never stop the cycle. What I would like to do right now is take a quick look at some of the studies that show this cycle, and how this gut-microbiota-brain axis dysfunction all works together in unison (I chose these particular studies because if you are interested, you can look them up and read them in their entirety). The point of doing this?
For those of you who are deep into these and other similar disease processes, you need to realize there is hope (stick around and I’ll prove it to you). One critical fact you must grasp before we begin is that it is not as likely as you have been led to believe that your children will be condemned to the same fate as you simply because of their genetics. Why not?
Science has given genetics way too much importance as far as the development of most diseases is concerned. What do I mean by this? If you don’t understand the difference between genetics and epigenetics as related to chronic inflammatory degenerative illnesses and autoimmune diseases, it is imperative that you take five minutes to read THIS POST on the topic. Also, if you are not sure what INFLAMMATION is (hint; it’s not swelling or infection), don’t bother continuing because it won’t make sense.
- THE GUT-MICROBIOTA-BRAIN AXIS; PARKINSON’S DISEASE: Listen to the conclusions from a two year old issue of the World Journal of Gastroenterology (Brain-Gut-Microbiota Axis in Parkinson’s Disease). Make sure to look for all five entities mentioned in the cycle above (BTW, this is quoted word-for-word). “Parkinson’s disease (PD) is characterized by alpha-synucleinopathy that affects all levels of the brain-gut axis including the central, autonomic, and enteric nervous systems. Recently, it has been recognized that the brain-gut axis interactions are significantly modulated by the gut microbiota via immunological, neuroendocrine, and direct neural mechanisms. Dysregulation of the brain-gut-microbiota axis in PD may be associated with gastrointestinal manifestations frequently preceding motor symptoms, as well as with the pathogenesis of PD itself, supporting the hypothesis that the pathological process is spread from the gut to the brain. Excessive stimulation of the innate immune system resulting from gut dysbiosis and/or small intestinal bacterial overgrowth and increased intestinal permeability may induce systemic inflammation, while activation of enteric neurons and enteric glial cells may contribute to the initiation of alpha-synuclein misfolding.” Why am I at least somewhat concerned about this nasty creature named by doctor Parkinson? I undoubtedly carry the gene (HERE). And for those who are not sure what GLIAL CELLS are (you’ll see them come up time and time again), just click the link.
- THE GUT-MICROBIOTA-BRAIN AXIS; NEUROPSYCHIATRIC DISORDERS: This collaboration (Gut-Microbiota-Brain Axis and Effect on Neuropsychiatric Disorders with Suspected Immune Dysregulation) between Greek and American scientists / physicians was published in HHS Public Access, and is one of the most amazing put-it-all-together studies I have yet to see on this topic. “Brain function and psychological make-up are now increasingly considered to have a reciprocal relationship with the gut. Disruption of the gut microbiota (dysbiosis) is known to contribute, among others, to the pathogenesis of GI diseases, and reported to directly induce inflammation and pain. Accumulating evidence suggests that the gut microbiota maintain bidirectional interactions with critical parts of the central nervous system (CNS) and the immune system through direct and indirect pathways. These involve the endocrine (hypothalamic-pituitary-adrenal (HPA) axis), immune (chemokines, cytokines), autonomic nervous system (ANS), and enteric nervous systems forming the microbiota-gut-brain axis. Antibiotics, environmental and infectious agents, intestinal neurotransmitters / , sensory vagal fibers, cytokines, essential metabolites, all convey information about the intestinal state to the CNS. Such interactions appear to influence the pathogenesis of a number of disorders in which inflammation is implicated such as mood disorder, autism-spectrum disorders (ASDs), attention-deficit hypersensitivity disorder (ADHD), multiple sclerosis (MS) and obesity (Obesity has been called a psychiatric disease) and is associated with depression and other neuropsychiatric disorders). Neuro/immune-active substances derived from the intestinal lumen can penetrate the gut mucosa, be transported by blood, cross the blood-brain-barrier (BBB) and affect the CNS. Acute stress increased GI and BBB permeability. Moreover, chronic stress disrupted the intestinal barrier and permitted penetration of luminal antigens, microflora metabolites, toxins and lipopolysaccharide (LPS) into the systemic circulation and the CNS.” Did you notice that all five aspects of the cycle were present in full-blown Technicolor and Dolby Surround Sound?
- THE GUT-MICROBIOTA-BRAIN AXIS; MULTIPLE SCLEROSIS: So, in light of everything that I’ve shown you, should we be even bat an eye when articles like STAT’S Gut Germs Play Role in Multiple Sclerosis, are published? No way! While it’s certainly good to know (I’ve discussed this link at least twice before — HERE and HERE), the real question remains; what are you doing about this since your doctor isn’t doing much of anything other than prescribing more drugs? In the first of two brand new studies, both from last month’s issue of PNAS, researchers compared the MICROBIOMES of 71 people with MS and 71 without MS. What they found was that “specific bacterial taxa were significantly associated with MS” (dysbiosis). But interestingly enough, they also found that there was a certain strain of bacteria that was “reduced in MS patients.” Because the researchers believed this bacteria was associated with antiinflammatory properties, they introduced feces from the MS group into mice that had been genetically raised to be “germ free“. The result was mice with fewer TREGS (T-suppressor cells that dampen immune system responses as to prevent autoimmunity) and fewer antiinflammatory cytokines, leaving them with symptoms of MS (“experimental autoimmune encephalomyelitis“). In the second study, the authors took identical twins, where one had MS and the other did not. They noticed that when they transplanted feces of the MS twin into mice that had been genetically raised to express “spontaneous brain autoimmunity,” those mice were much more likely to develop an “MS-like autoimmune disease.” I need to note to you; one major difference in MS patients is that they tend to have low sympathetic function (as opposed to high), which often results in heart, bladder, and bowel issues. By the way, I found studies over two decades old (Digestive Diseases and Sciences — Multiple Sclerosis Patients Have Increased Intestinal Permeability) that showed this link via their title. The moral of this story is NEVER underestimate the importance of GUT HEALTH in dealing with chronic conditions!
- THE GUT-MICROBIOTA-BRAIN AXIS; CHRONIC “LEARNED” PAIN: This two year old study was done at St. Louis’ Washington University and published for the International Anesthesia Research Society (Identification and Treatment of New Inflammatory Triggers for Complex Regional Pain Syndrome: Small Intestinal Bacterial Overgrowth and Obstructive Sleep Apnea). “Complex regional pain syndrome (CRPS), formally known as reflex sympathetic dystrophy, is a neuropathic pain disorder that may fail to respond to current therapy… There is a known relationship of CRPS and the gastrointestinal tract. Dysbiosis (alterations of the microbiome) and increased intestinal permeability (which is present in SIBO) have been reported in CRPS, and these two conditions also cause chronic systemic inflammation. IBS is common in CRPS although the relationship has hitherto not been elucidated. In multiple studies, SIBO was found to be present in up to 50% of IBS-d patients.” IBS and IBD are both known to be autoimmune, while SIBO is typically the result of a sensitivity to FODMAP-CONTAINING carbohydrates. And as you might imagine from its old name (Reflex Sympathetic Dystrophy), the sympathetic side of the ANS is hyped to the max in those with CRPS.
- THE GUT-MICROBIOTA-BRAIN AXIS; INTENSE EXERCISE: Just ten short months ago, the Journal of the International Society of Sports Nutrition published a study called Exercise-Induced Stress Behavior, Gut-Microbiota-Brain Axis and Diet: A Systematic Review for Athletes. The European authors concluded that “The demands during intense exercise can initiate a stress response activating the sympathetic-adrenomedullary and hypothalamus-pituitary-adrenal (HPA) axes, resulting in the release of stress and catabolic hormones [these break your body down], inflammatory cytokines and microbial molecules. The gut is home to trillions of microorganisms that have fundamental roles in many aspects of human biology, including metabolism, endocrine, neuronal and immune function. The gut microbiome and its influence on host behavior, intestinal barrier and immune function are believed to be a critical aspect of the brain-gut axis. Recent evidence in murine models shows that there is a high correlation between physical and emotional stress during exercise and changes in gastrointestinal microbiota composition. Diet is known to dramatically modulate the composition of the gut microbiota. Due to the considerable complexity of stress responses in elite athletes (from leaky gut to increased catabolism and depression), defining standard diet regimes is difficult.” There are the five; together again for what hopefully turns out to only be a ‘limited engagement’.
So, what are you supposed to do if you have these or other inflammatory, degenerative, or autoimmune disease? The first thing you must is learn everything you can about it you can and make yourself an expert. Thanks to the internet; some diligent study on your particular condition (use PubMed or other databases of medical studies, as well as message boards), and a large percentage of you will be as knowledgeable as your doctor(s) on your particular issue.
Face it; the gap between the cool stuff coming out of medical research (the stuff I showed you today concerning the gut-microbiota-brain axis) and the standard fare of CRAPPY DRUGS or WORTHLESS TESTS you get at your doctor visits makes the Grand Canyon look like the tiny ditch in your front yard. Be willing to step out of the box just a bit and watch what happens!
Secondly, using said information, sit down and create yourself a top-to-bottom EXIT STRATEGY. Although you may have to modify your plan along the way for any number of different reasons (including new information coming available) purpose in your heart to stick with it and work it as though your life depends on it — because it probably does. Fortunately, I have created an extremely generic template for making this happen (HERE).
For many of you, this is all you’ll need. For the rest, there are people out there versed in FUNCTIONAL NEUROLOGY and FUNCTIONAL MEDICINE that can likely help. One last thing. If you are chronically ill, DO NOT go to sleep tonight without learning the basics of one of the hottest topics in the medical research field right now — FECAL MICROBIOTA TRANSPLANTS — something that may sound gross but makes a great deal of sense if you grasp the gut-microbiota-brain axis. If you enjoyed this post be sure to like, share or follow on FACEBOOK.
