THORACIC OUTLET SYNDROME
|
“Actually it [TOS] is not widely known and it is also a controversial issue for some physicians. Moreover, it is sometimes strongly denied by those who have not had the opportunity of identifying it as a disease or even when they have not dealt with TOS patients.… We are confronted with a disease that is commonly undiagnosed by the majority of physicians.” — Cardiothoracic Surgeons, Dr. Raul Poblete Silva MD F.A.C.S. Emeritus Assistant Professor, Department of Surgery, University of Chile, former Head Department of Vascular Surgery at the Military Hospital of Santiago, Chile. Carlos A. Selmonosky MD, F.A.C.S., F.A.C.C.P. Department of Medicine, Inova Fairfax Hospital, Falls Church VA.
|
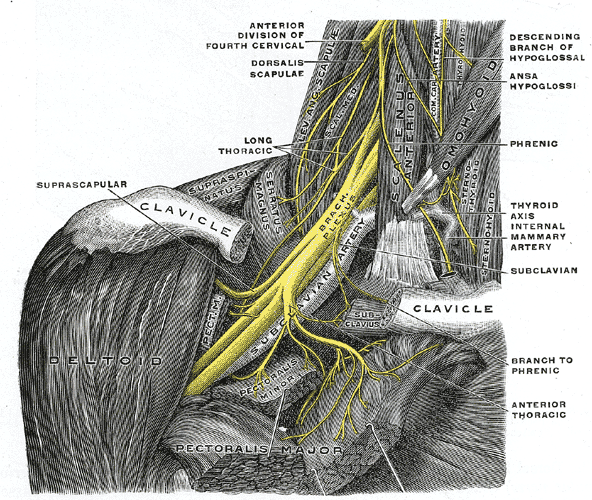
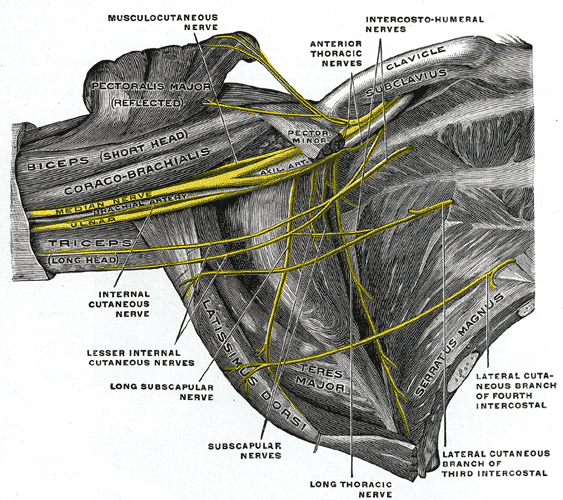
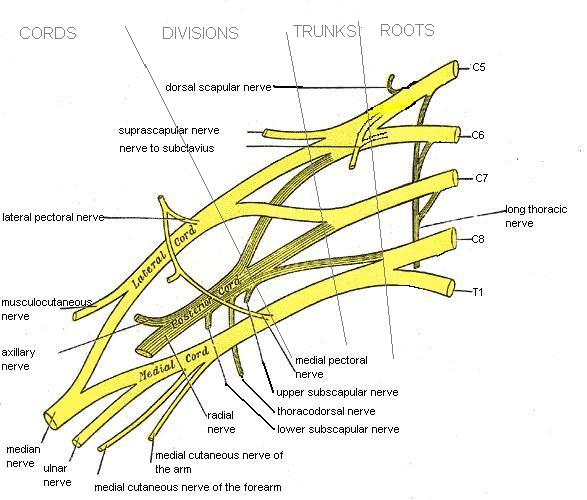
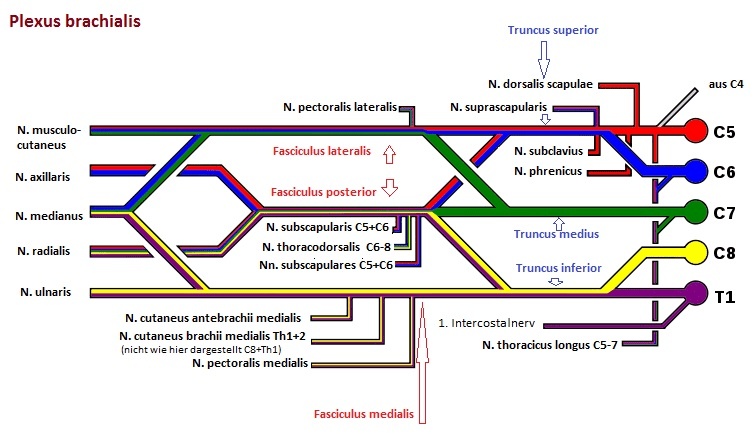
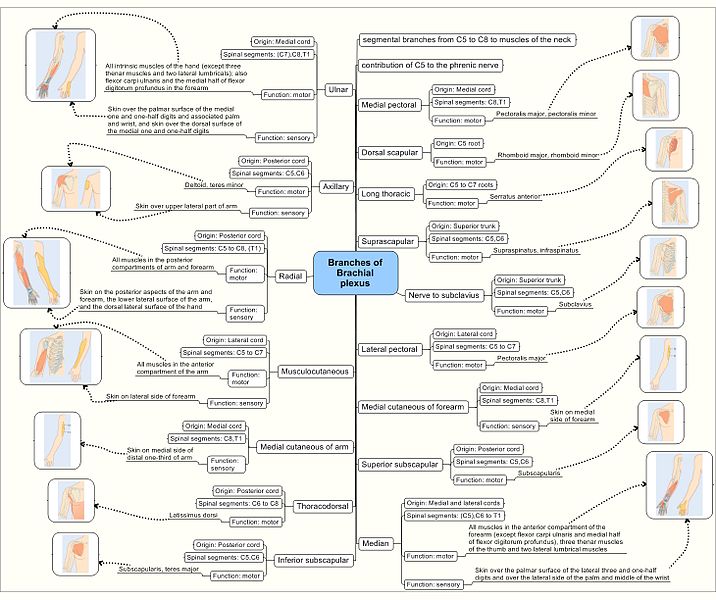
Some of the most common symptoms of Thoracic Outlet Syndrome include things like shoulder pain / weakness, arm or hand pain / weakness, pain and restriction of the neck, chest pain, and others. To those who are paying attention you’ll notice that TOS shares many of the same symptoms as Multiple Sclerosis, FIBROMYALGIA, RAYNAUD’S PHENOMENON, CERVICAL DISC PROBLEMS, ROTATOR CUFF PROBLEMS, CERVICAL (NECK) SUBLUXATIONS, SHOULDER TENDINOSIS, SHOULDER BURSITIS, CARPAL TUNNEL SYNDROME, and even certain types of Spinal Tumors. Now you can see why it is difficult to diagnose, but in order to show you what TOS really is, I want to show you a little bit of anatomy first. We’ll start with the nerves in the neck and armpit region — the Brachial Plexus.
THE BRACHIAL PLEXUS
WHICH TISSUE IS BEING COMPRESSED?
WHICH TISSUE IS DOING THE COMPRESSING?
Not to sound cold or calloused, but I am not extremely interested in exactly what structure is being compressed (blood vessel or nerve). What I am really interested in is which tissue is doing the compressing. This is because in many (maybe the majority) of Thoracic Outlet cases, it is muscles that are guilty of compressing the arteries and nerves. In other words, there is a great chance that this problem can be managed with TISSUE REMODELING.
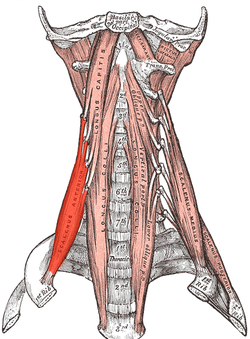
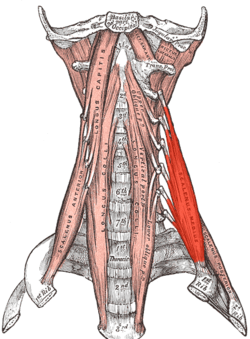
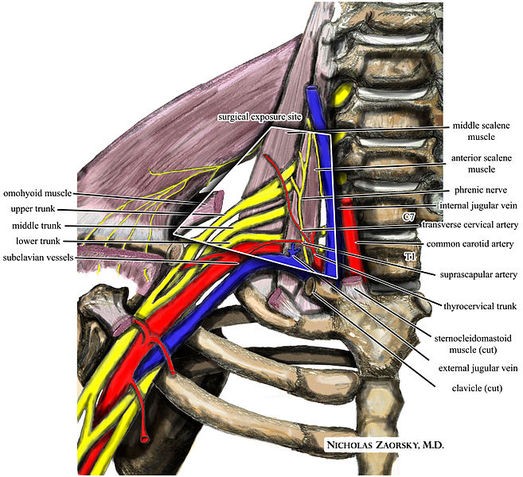
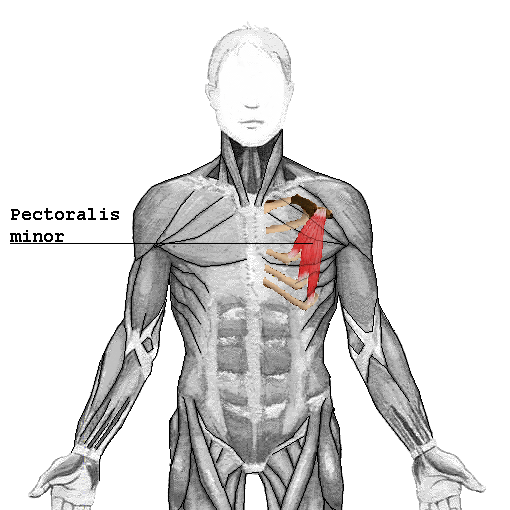
Which muscles are the most frequent culprits as far as compressing blood vessels or nerves is concerned? Let’s look first at the Anterior and Medial Scalene Muscles. When the Scalene Muscles are under constant tension, they actually hypertrophy (get bigger), making compression of the Brachial Plexus that much easier. In the picture underneath these two, you will notice one of the most common place for TOS compression to occur. The question now becomes, what puts so much tension on the Scalene Muscles? We’ll answer that, but first I want to talk about the three types of Thoracic Outlet Syndrome.
SCALENE MUSCLES SEEN ON THE LEFT SIDE, BUT LABELED ON THE TOP RIGHT
NOTICE THE BRACHIAL PLEXUS AND SUBCLAVIAN VESSELS DIRECTLY UNDER THE (REMOVED) COLLAR BONE
THE THREE KINDS OF THORACIC OUTLET SYNDROME
- NEUROGENIC TOS: As the name implies, this is the form of Thoracic Outlet Syndrome that is due to compression of the nerves that make up the Brachial Plexus. 19 out of 20 people suffering from TOS have the Neurogenic form of the problem. Neurogenic TOS will sometimes be severe enough to have caused atrophy in the meaty muscle at the bottom (palm) of the thumb. However, before atrophy sets in, most people with Neurogenic TOS will complain of numbness and tingling, or pins and needles in the fingers and hand. Weakness will frequently be seen as well. Sometimes the hand will be prone to blanching or be cold for no reason. This will often times be associated with dull achy pain in the neck, shoulder, or arm region — often on the underside in the armpit area. The person may complain of forearm muscle cramping and difficulty with fine motor skills. This is the most likely type of TOS to be caused by FASCIAL ADHESIONS.
- ARTERIAL TOS: Arterial Thoracic Outlet Syndrome is, as you might guess from the name, due to a compression of an artery. In this case, the artery happens to be the Subclavian Artery (sub – under, clavian – clavicle); the artery that runs under the collar bone. People with the Arterial type of Thoracic Outlet Syndrome tend to complain of changes in the color of the hand, hands that are hypersensitive to cold, as well as swelling of the hands. In essence, they get almost the same set of symptoms that someone with Neurogenic TOS would get. The biggest difference to look for is the swelling in the forearm and hand. In some of the more radical cases of Arterial TOS (remember, Arterial TOS is less than 5% of all TOS), we can see double vision and other visual disturbances, vertigo, fainting, hearing loss, etc. This is what can happen when blood flow is significantly decreased.
- VENOUS TOS: Venous Thoracic Outlet Syndrome is caused by compression of the Subclavian Vein — the vein that runs underneath the clavicle (collar bone). Guess what? Venous TOS also has the same general set of symptoms as the other two forms of the problem. However, these folk’s TOS tends to be characterized by a weaker pulse than the opposite side (unless they happen to have it bilaterally). The vessel-related forms of TOS (Arterial & Venous) are less likely to respond to what I do, although we have helped a lot of patients with this type of TOS over the years. Although it matters a great deal to a surgeon, it does not so much matter to me if the compression is occurring at the Brachial Plexus or at one of the Subclavian (below the Collar Bone) Blood Vessels. My conservative treatment will be the same either way.
CAUSES OF THORACIC OUTLET SYNDROME
|
The predisposing factors responsive for the development of thoracic outlet syndrome are fibromuscular bands, bony protuberances and long or larger transverse processes, this together with the tendinous or cartilaginous muscular insertions are responsible for the compression of the neurovascular structures at the thoracic outlet. –Dr. Carlos Selmonosky, one of America’s premier TOS surgeons (retired).
|
It has also been shown that if you get symptoms while carrying a backpack or wearing a heavy jacket, this might be a tip off that you have TOS. Any sort of heavy burden on the shoulder girdles can cause neurovascular compression in the “Thoracic Outlet” (Thoracic Outlet Syndrome). Bottom line; there is lots of potential for people to develop Thoracic Outlet Syndrome. But every cloud has a silver lining.
Re-read the quote at the beginning of this section. Look what it says. It talks about “fibromuscular bands” (fibrous = Scar Tissue). If you want to read about Scar Tissue in muscles, HERE is the single best place on the web to do it. The quote also mentions “tendinous tnsertions“. Guess what? The single best information on Tendinosis on the internet can be found HERE. For those who do not grasp how big a deal this is, it is like being handed the blueprint for tackling this problem. It reminds me of Arnold’s famous line from 1987’s classic offering, Predator. Just after Dutch and his band of elite mercenaries wildly open up on their unseen alien stalker, he utters the famous line; “If it bleeds, we can kill it“. If your TOS symptoms are coming from compression due to FASCIAL ADHESIONS or some sort of TENDINOSIS, there is a fighting chance that your problem can be solved conservatively (non-surgically).
DIAGNOSING THORACIC OUTLET SYNDROME
|
Diagnosis of TOS is mainly done on clinical basis. Dr. Raul Poblete Silva F.A.C.S. Emeritus Assistant Professor, Department of Surgery, University of Chile, former Head Department of Vascular Surgery, Military Hospital of Santiago, Chile
|
- POINT TENDERNESS IN THE AREA JUST BEHIND THE COLLAR BONE: This is tenderness in the general area where compression occurs in Thoracic Outlet Syndrome. It is where all the structures lie (the arteries and nerves) that can be compressed, as well as the muscles, ligaments, tendons, or bones (i.e. the first rib or cervical rib) that can do the compressing.
- HAND(S) BLANCHING WHEN ELEVATED TO OVERHEAD POSITION: When the hands are raised overhead for anywhere from 2-5 minutes, the affected hand(s) will blanch white (pale). When the patient holds their hands over their head while trying to reproduce TOS symptoms, they need to hold their elbows at a 90 angle and push them backwards (the chest will jut out slightly when this is done properly).
- PINS AND NEEDLES / NUMBNESS AND TINGLING IN HAND(S) WHEN ELEVATED TO OVERHEAD POSITION: Hold your hands over your head; in the same position the bullet point above talked about, for about 2-5 minutes. The affected hand(s) will develop numbness and tingling or pins and needles. Doctors refer to these sensations as ‘paresthesias’.
- FINGER WEAKNESS: Have the person stand in front of you with their hands out, palms down, and fingers together. Now put your hand around their finger and gently resist while they try to push their fingers apart. Now do the opposite. Same thing, but with their fingers spread wide apart, see how much force it takes to squeeze them together. Weakness; particularly in the ring and pinky fingers could indicate TOS.
- SCALENE TEST: Have the person sit down. Get a pulse at the wrist of the affected side. Now have them turn their head toward the affected side and tip their head backward, while you move their extended arm backwards as far as you can do so comfortably. The lessening or obliteration of a pulse indicates a positive test. Be aware that this test, also called Adson’s Maneuver is no longer considered diagnostic because of the incredible numbers of false positives.
- COSTOCLAVICULAR MANEUVER: Be warned that there are about a million and one variations on this test. The easiest is to simply have the patient stand at attention, chest up and out, with their shoulders drawn back. Just like the test above, pull their extended arm backwards to their tolerance and see if the pulse goes away.
- CAN YOU MAKE YOUR SYMPTOMS GO AWAY? If you have a patient with symptoms you think might be TOS, have them stand with their arms crossed (mummy-like) over the chest. Now step around behind them, grab the elbows and ‘lift’ up on both shoulder girdles. Hold the position for at least one minute. Did the patient get relief? Could be that you are ‘decompressing’ a Thoracic Outlet Syndrome by raising the collar bones off the affected structures.
As you can see, the diagnosis is tricky. Not only does Thoracic Outlet syndrome look like several other problems, the symptoms of all three types of TOS are almost identical to each other. This is why I said earlier that we are much more interested in the tissue that is compressing, rather than the tissue being compressed. For our purposes, it does not really matter what is being compressed. If it is possible to relieve the compression, the tissue being compressed is irrelevant.
TREATING PATIENTS WITH TOS
|
“Left untreated a severe progressive denervation [loss of nerve supply] of the upper limb occurs affecting mostly the C8-T1 nerve areas [supplies the ring and pinky fingers]. The muscle atrophy can lead to advanced muscle wasting of hand and arms results in ankylosis [ARTHRITIS] of the shoulder that may lead to a frozen shoulder.” World’s foremost expert on TOS, Dr. Raul Silva, from a 2011 internet article on the subject.
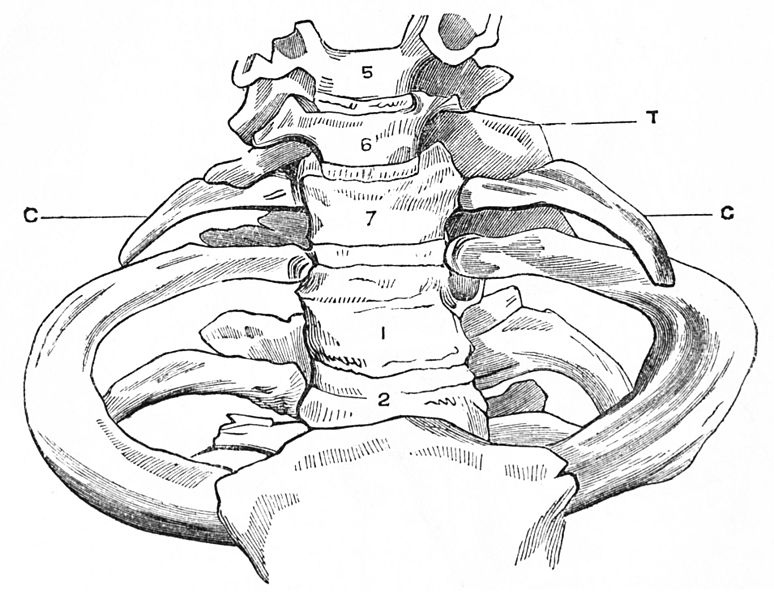
CERVICAL RIB: Notice the Cervical Rib (‘C’) at the C7 Vertebral Level
|
If, after examining the patient, I suspect TOS, the first thing I will do is determine which particular muscles, tendons, fascias, etc, might be constricted with Microscopic Scar Tissue. Like I have said before, whether the problem is vascular or neurogenic does not matter too much to me at this point. I am going to treat this patient 1 – 4 times (depending on what I do) and look for improvement. If we get improvement, we continue. If not, I will refer the patient out for further evaluation. With our Tissue Remodeling, we will know in one or two treatments whether or not Microscopic Scar Tissue is the major culprit (VIDEO TESTIMONIALS).
Why is properly Diagnosing and Treating Thoracic Outlet Syndrome so important? Because if patients do not get better with conservative care, they need to be re-evaluated. Let me share a story with you. Earlier this year, a good friend of mine and I were eating lunch and jawing about sports. We were sitting out on the deck, eating my wife’s famous white chili, and talking about the old Houston Astros (can anyone say Nolan Ryan?). My friend is quite the expert on the subject as he is about 20 years older than I, as well as being from Texas. I asked him whatever happened to JR Richard. We both vaguely recalled something about him having a stroke, but did not know anything about it. My first thought was that it was a Darryl Strawberry sort of thing (i.e. drugs). Imagine how surprised I was while researching this topic to find out that Richards’ stroke was caused by a vascular TOS. Wow; TOS can cause a stroke!
But the real kick in the teeth concerning untreated vascular TOS was something that one of the world’s foremost experts on TOS, Cardiothoracic Surgeon, Dr Raul Silva, said at the end of an article he had written the subject. Although the mechanism is unknown at this point, Dr Silva stated that, “Thoracic Outlet Syndrome is a highly prominent and important factor in the genesis, and progression of Multiple Sclerosis” — and he had some hard evidence to back up his assertion. As you may have guessed, MS is an AUTOIMMUNE DISEASE that can destroy one’s life. What the connection is, I have no idea. It is interesting to note, however, that another Autoimmune Disease, Raynaud’s Phenomenon (chronically cold hands that blanch white) has the appearance of Thoracic Outlet Syndrome as well.
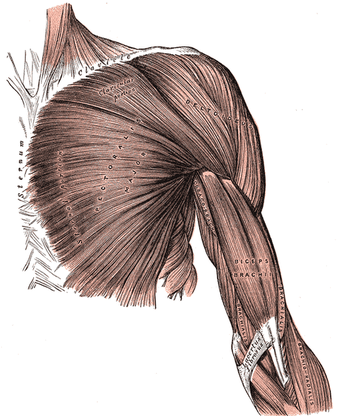
THE PECTORAL / DELTOID / BICEP JUNCTION
WHERE THE SHOULDER, BICEP, AND CHEST ALL COME TOGETHER
|
As you can see, this is a miserable and potentially serious problem. Help us spread the word by liking us on FACEBOOK.
|