SCAR TISSUE OR FIBROSIS?
DOES IT REALLY MATTER WHAT WE CALL IT?
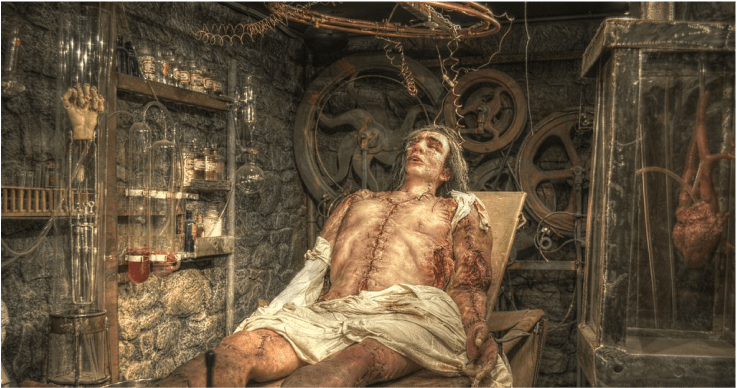
In my clinic, I talk about Scar Tissue —- a lot (HERE). When most of us think of Scar Tissue we picture it as seen above. The wax replica of Frankenstein’s Monster is a mass of scars; on his head, torso, trunk, and limbs. Although I do treat lots of people with POST-SURGICAL SCAR TISSUE, most of what I treat are the invisible FASCIAL ADHESIONS that, by their very nature, continue to befuddle most of the medical community (HERE). We’ll talk about why throughout the post.
Although it’s never patients that are guilty, people sometimes take me to task for talking or writing about “Scar Tissue”. Need an example? Here is a recent email I got from an Orthopedic Surgeon somewhere on the East Coast (name will remain anonymous). “Dr. Schierling, Having read some of your material on scar tissue I feel I must set the record straight by telling you how wrong you are to confuse it with fibrosis or what you refer to as “Fascial Adhesions”.
He went into more detail, talking about things like Keloids, and telling me that I was setting the practice of medicine back by oversimplifying and mixing some of these terms. Although he could potentially be correct, I doubt it. And to prove my point, I’ll use that pinnacle of academia — Wikipedia. Although many people decry Wikipedia (I completely understand why), I’m an unabashed fan — especially when an entry is well-referenced so that I can look at sources. Today we are going to discuss its entries for both Scar Tissue and Fibrosis, and see if we can learn anything about this debate. Please note that I cherry-pick everything so as to keep the post from getting too long. This is taken from their entry on Scar Tissue (Scars).
“Scars are areas of fibrous tissue (fibrosis) that replace normal skin (and other tissues) after injury of the body. Thus, scarring is a natural part of the healing process. With the exception of very minor lesions, every wound (e.g., after accident, disease, or surgery) results in some degree of scarring.”
Sometimes in the practice of medicine, a tissue that is exposed to injury, surgery, or disease processes, is referred to in a strange-sounding manner. Said tissue is said to have experienced an “insult” or been “embarrassed“. Often times these sorts of things have to do with the sort of tissue damage that causes INFLAMMATION. It is critical for understanding this post that you understand Inflammation. Mostly because Inflammation always leads to Fibrosis (HERE). Doctors realize this and attempt to squelch this most common of Immune System responses by prescribing drugs to block it (usually NSAIDS and / or CORTICOSTEROIDS). As we move forward we see that….
“Scar tissue is composed of the same protein (collagen) as the tissue that it replaces, but the fiber composition of the protein is different. This collagen scar tissue alignment is usually of inferior functional quality to the normal collagen alignment.”
If you want to see pictures of Connective Tissues (LIGAMENTS, TENDONS, FASCIA, and MUSCLES — yes, I know that muscles are not really a ‘Connective Tissue’), click the links. It is the “inferior functional quality” that leads to repetitive re-injury of the affected area (which subsequently leads to DEGENERATION). If you are interested in reading about COLLAGEN and the healing processes it must go through after insult, injury, embarrassment, or whatever you want to call it, follow the link. Let’s continue.
“An injury does not become a scar until the wound has completely healed; this can take many months, or years in the worst pathological cases…. To begin to patch the damage, a clot is created; the clot is the beginning process that results in a provisional matrix. Over time, the wounded body tissue then overexpresses collagen inside the provisional matrix to create a collagen matrix. This collagen overexpression continues and crosslinks the fiber arrangement inside the collagen matrix, making the collagen dense. This densely packed collagen, morphing into an inelastic whitish collagen scar wall, blocks off cell communication and regeneration; as a result, the new tissue generated will have a different texture and quality than the surrounding unwounded tissue.”
The way I like to think of it is that when you are injured, the area bleeds (microscopically and maybe very minimally) into the surrounding tissues, which in turn causes tissue to be laid down for repair. Via use and normal mechanical stresses, this tissue aligns itself in as an elastic manner as it can, going through a process known as the “Remodeling Phase”. This is the fourth and final stage of the soft tissue repair process, and not surprisingly, is not only the least talked about but the longest lasting (see previous link).
Although Inflammation abounds (see previous link on inflammation as the chemicals whose purpose is to provide communication between cells and tissues in order to get the body to start its tissue healing process), the resultant Scar Tissue prevents said communication. Furthermore, not only does Inflammation hypersensitize nerve endings to pain (HERE), it always leaves the resultant tissue of a “different” (poor, weak, inelastic) quality; the reason that things are never quite the same after an injury (HERE). The entry also spent a great deal of time discussing FIBROBLASTIC PROLIFERATION — something needed, at least initially, for healing to take place. It’s also why hardcore soft tissue problems must sometimes be addressed with the same mindset as playing a carnival game (HERE).
As a side note to this, the Scar Tissue entry also mentioned STRETCH MARKS. “Stretch marks (technically called striae) are also a form of scarring. These are caused when the skin is stretched rapidly (for instance during pregnancy, significant weight gain, or adolescent growth spurts), or when skin is put under tension during the healing process, (usually near joints).”
Although it does not happen on a daily basis, I have seen any number of patients who not only have this issue, but it actually causes significant pain and restriction (pictures in link above) — usually in the THORACOLUMBAR FASCIA (HERE is a recent example). Now we are going to discuss Wiki’s entry for Fibrosis. “Fibrosis is the formation of excess fibrous connective tissue in an organ or tissue” Although FIBROSIS can be caused by things other than injury, when injury is the cause, “it is called scarring. Physiologically, fibrosis acts to deposit connective tissue, which can obliterate the architecture and function of the underlying organ or tissue. Fibrosis can be used to describe the pathological state of excess deposition of fibrous tissue, as well as the process of connective tissue deposition in healing.” What is the chief difference between Scar Tissue and Fibrosis? Again, from Wikipedia’s entry on Fibrosis….
“Fibrosis is similar to the process of scarring, in that both involve stimulated fibroblasts laying down connective tissue, including collagen. The process is initiated when immune cells such as macrophages [a type of white blood cell] release soluble factors that stimulate fibroblasts. The most well characterized pro-fibrotic mediator is TGF beta [Cytokine — inflammation], which is released by macrophages as well as any damaged tissue between surfaces called interstitium. Other soluble mediators of fibrosis include CTGF, platelet-derived growth factor (PDGF), and Interleukin 4 (IL-4) [Inflammation]. These ultimately lead to the proliferation and activation of fibroblasts, which deposit extracellular matrix into the surrounding connective tissue.”
What did you see here? You saw that whether it came from an injury or some sort of disease process, Fibrosis was always (or at least almost always) preceded by one of the numerous chemicals responsible for intercellular communication that we collectively refer to as INFLAMMATION. Are you starting to see why I am such a stickler for number one, EATING AN ANTI-INFLAMMATORY DIET, and number two, figuring out what things other than your injury might be driving inflammatory processes in your body (HERE)?
The difference between Scar Tissue and Fibrosis? I’m not totally sure myself. Although it is mostly a matter of semantics, I would assume that people who specialize in this field would say that “scarring” is a normal physiological process, while “fibrosis” is much more likely to be pathological (caused by some sort of disease process or genetic abnormality). As for ‘Fascial Adhesions’, it’s a term that I made up to describe the phenomenon I regularly see in MY PATIENTS over the course of the last couple decades or so (truthfully, I’m not sure I’ve ever had an original thought in my life — someone was surely using it before I was). The chief problem with having this “Fibrosis” / “Scar Tissue” in the Fascia is that many experts argue that it is already one of the most potentially-painful tissues in the body to begin with.
Couple this with the fact that excepting the THORACOLUMBAR FASCIA and PLANTAR FASCIA, you can’t see it on MRI (HERE). And on top of everything else, Scar Tissue itself is known to potentially be as much as 1,000 times more pain sensitive than normal tissue. As you contemplate these facts, it’s not difficult to see a “PERFECT STORM” of Chronic Pain (not to mention the accusations of being a malingerer or drug seeker) looming on the horizon of many people’s lives. for those of you already living this nightmare, I have an article called TWENTY REASONS WHY FASCIA that might be very helpful.
Truthfully, I don’t really care what you want to call it. Call it ‘Banana Boat’ for all I care. It’s essentially the same stuff. Although the medical community would probably prefer the word “Fibrosis,” I usually use the term “Scar Tissue” when talking to patients, as it is something they can understand and easily relate to since everyone has scars. Regardless of terminology, I use pictures to describe what I am talking about. Truthfully, it can be virtually impossible to tell them all apart and doesn’t really matter at all as far as treating the patient is concerned (HERE). Speaking of treating……
It is almost impossible to get rid of Scar Tissue (HERE), but it can be “remodeled” if it can be accessed (HERE or HERE). When dealing with simple injuries, sometimes STRETCHING can be enough to solve them (and as the link reveals, sometimes not). Getting rid of hardcore Fascial Adhesions / Scar Tissue / Fibrosis is going to require some degree of “controlled trauma” in order to break the unorganized tissue matrix and ‘re-start’ the healing process (TISSUE DEFORMATION). Depending on the amount of Scar Tissue present, this process must sometimes be, at least to some degree, harsh (HERE). The awesome thing is, even if you’ve had your problem for decades, you’ll know after one treatment whether or not this approach will prove helpful for you (HERE).
