“The fascia is a sheet of connective tissue, primarily collagen, that separates muscle tissue. Inflammation in the fascia can be an important part of the disease in patients with dermatomyositis.”From the Myositis Association’s article from earlier this summer, Dealing with the Constant Hum of Pain. The article is essentially the transcript of a Q & A with Dr. Wael Jarjour, associate professor and director of the division of rheumatology and immunology at Ohio State University. His research is focused on autoimmunity, and his clinical practice focuses specifically on systemic autoimmune disorders.
I wouldn’t even begin to guess on the number of AUTOIMMUNE DISEASES that we know about (HERE is a list of some of some of the more well-known of the lot). The thing that’s scary, however, is the virtually endless list of Autoimmune Diseases that don’t know about because they do not have names or ways to test for them. In other words, no one has figured out what the auto-antigen is (the tissue, cell, protein, enzyme, organ, gland, hormone, etc, that the body is attacking). A major problem with this scenario is that known or unknown, once you have one autoimmune disease you are likely to end up with several, as they tend to travel in packs like wolves. As I’ve told you before, this is not the result of faulty tissues or organs (THYROID for instance), but due to a faulty immune system — an immune system that “decides” to attack self.
What causes the body to start attacking itself? In other words, what drives autoimmunity? That’s easy; the same thing that drives most health-related problems — INFLAMMATION. The problem is that there are about a million things that can drive inflammation. And here’s the kicker. While said inflammation can certainly cause autoimmunity, it doesn’t end there. Inflammation always leads to SCAR TISSUE or FIBROSIS, and fibrosis always leads not only to degeneration (HERE), but is the very thing that kills the majority of Americans (HERE and HERE).
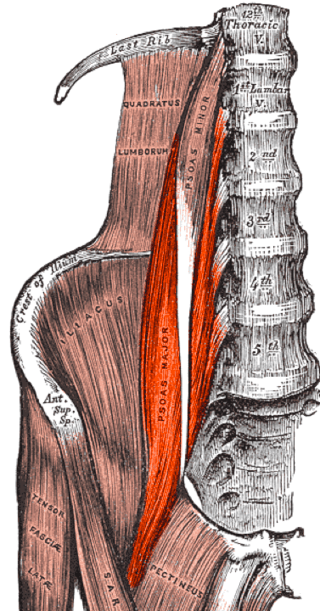
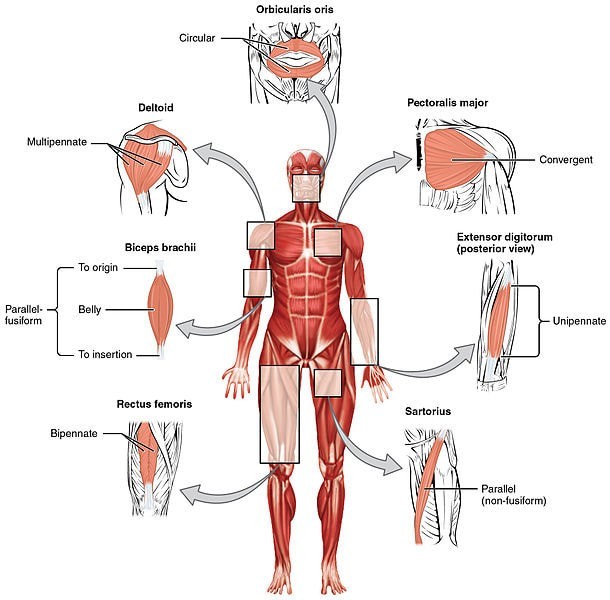
Although there are almost an unlimited number of these unnamed autoimmune, there are some named autoimmune diseases that are intimately associated with FASCIA. The one that comes immediately to mind is one that my sister had called Scleroderma that SHE TOOK CARE OF IT NATURALLY. Sclero = scar tissue, and Derma = skin. Some of the biggest names in fascia research (Schleip, Findley, Chaitow, and Huijing) discussed the relationship between fascia and autoimmunity as related to scleroderma in 2012’s 550 page behemoth, Fascia, The Tensional Network of the Human Body.
Because slceroderma is characterized by a thickening of the skin, it affects fascia (see how the fascia is related to the skin HERE). As you can imagine, this not only causes a host of problems, but in some cases can actually attack and thicken organs as well. In scleroderma, inflammation causes the skin to become “LEAKY,” which leads to more inflammation, eventually causing significant dysregulation of FIBROBLASTS. Scleroderma is also related to MCTD (Mixed Connective Tissue Disease), which has characteristics of it, as well as of lupus, MYOSITIS, and RHEUMATOID ARTHRITIS (and sometimes Sjögren Syndrome, which causes dry eyes, dry mouth, CHRONIC FATIGUE and joint pain, as well as problems with organs, blood vessels, and the central nervous system). Speaking of RA…
The brilliant HELENE LANGEVIN wrote an article for The Rheumatologist (What Role Does Fascia Play in Rheumatic Diseases?) in which she essentially asked why fascia is being ignored in rheumatic diseases even though it, “should fall squarely within the purview of rheumatology.” Instead, she said that the tissue is, “barely mentioned“. She went on to say (I’m cherry-picking)……
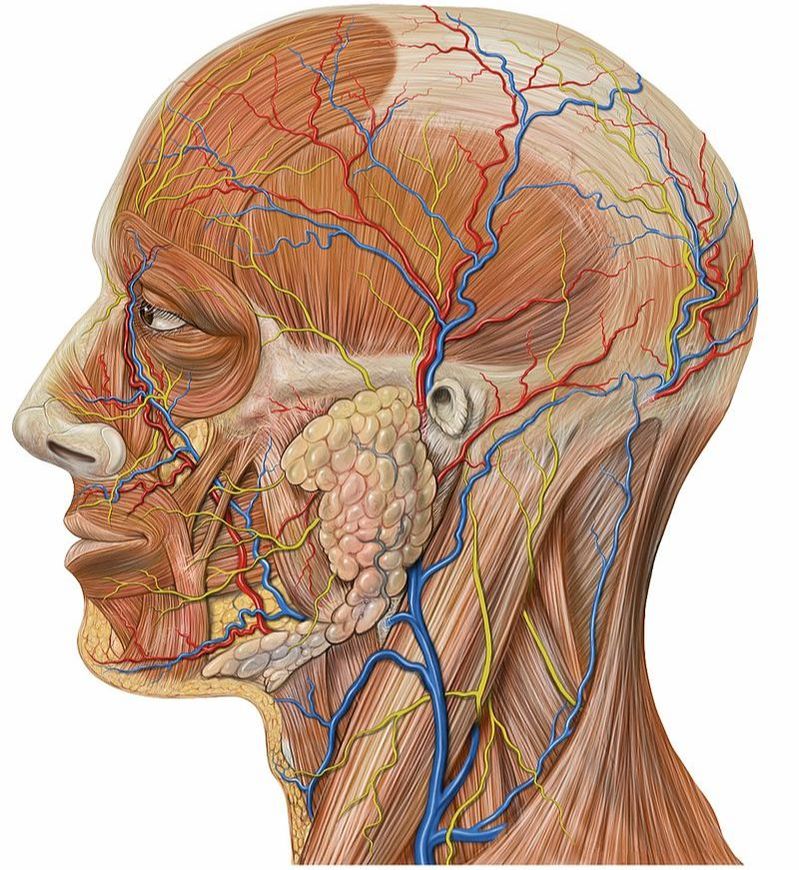
“Can pain come from fascia? fasciae are substantially innervated, and there are sensory receptors within fascia that respond to mechanical and chemical stimuli. Furthermore, the receptive fields of these sensory neurons enlarge in the presence of inflammation, supporting the potential role of fascia as a ‘pain generator.'”
Dr. Langevin went on to discuss the pathological “thickening” of fascia that’s most commonly seen in the THORACOLUMBAR FASCIA of in people with chronic low back pain. She then asked whether or not it would be possible that, “inflammation may also be present in fasciae? Could fascia involvement in rheumatoid arthritis contribute to pain and the diffuse ‘morning stiffness,’ even before overt joint pathology has occurred?” She cites two studies as proof that this is likely then talks about the importance of STRETCHING (a standard component of MECHANORECEPTIVE REHABILITATION). And finally, after talking about fascia’s relationship to the immune system, she says, “If this is true, body movements (change in position, exercise, stretching) could play an important role in immune surveillance mechanisms and possibly in autoimmunity.” Speaking of autoimmunity as related to fascia, listen to what professor, author, researcher, and physician, Rula A. Hajj-ali of the Cleveland Clinic said in the Merck Manual — the world’s oldest and best-selling medical textbook since 1899.
After talking about connective tissues in terms of LIGAMENTS, TENDONS, and others (not shockingly he left out fascia), he stated, “In autoimmune disorders, inflammation and the immune response may result in connective tissue damage, not only in and around joints but also in other tissues, including vital organs.” Why would this be? Why would this doctor mention things like heart problems, kidney problems, or lung problems as associated with autoimmune connective tissue issues and joint pain? Only because virtually all of your body’s tissues and organs (not to mention joints) are wrapped in fascia! This fascia goes by dozens of different names (usually according to where its found), but are all composed of essentially the same ‘stuff’.
Although this next study pertains to DUPUYTREN’S CONTRACTURE of the palmar surface of the hand, the sequence of metabolic pathology leading to the thickening and contracture will be similar in all autoimmune issues (numerous studies have characterized DC as an autoimmune disease). Last July’s issue of Current Molecular Biology Reports (Connective Tissue Degeneration: Mechanisms of Palmar Fascia Degeneration) revealed that,
“The early phases of the wound healing response are dependent on inflammation and fibrogenesis, recruitment of platelets, immune cell and fibroblast invasion, pro-inflammatory cytokine secretion, differentiation of fibroblasts to myofibroblasts and fibrin clot formation. If the damaging stimuli are repetitive, this will lead to persistent inflammation; higher levels of interleukins, tumor necrosis factor alpha (TNFα) and pro-fibrogenic transforming growth factor beta (TGFβ) [all in the family of inflammation] and therefore scarring. Although acute tissue injury is resolved completely, repetitive chronic injury, the addition of other factors such as age or diabetes or chronic inflammation have the potential to interfere with the correct remodeling of tissue and are contributing factors to persistent scarring. Mast cells [they release histamine, another inflammatory mediator] could also be involved in the inflammatory response leading to the development of fibrosis.”
Bottom line, while ACTIVATION OF FIBROBLASTIC ACTIVITY is typically a good thing, when these processes turn pathological, too much of a good thing becomes a bad thing — potentially a very bad thing.
Here’s one that will knock your socks off. Dr Langevin (an endocrinologist and neurologist) just showed us that fascia is essentially an immune system organ (something I’ve talked a bit about HERE). As far as the immune system goes, we already know that something like 70 or 80 percent of it is found in the Gut (HERE). An article called The IBS/SIBO-Psoas Connection and Why It’s Important for Highly Sensitive People calls this relationship into play. As you read this, you need to be aware that the vast majority — some studies say 85% — of THOSE WITH SIBO HAVE IBS (the former is believed by many to be autoimmune, while the later is known to be autoimmune), and both are intimately related to a host of other autoimmune diseases. The author simply connected the dots (quotes below are cherry-picked). Side Note: You will see how important this relationship really is when you see my next post on the relationship between inflammation and SYMPATHETIC DOMINANCE.
“The psoas bridges the belly’s enteric brain, central, and autonomic nervous systems. The large nerve ganglion located within the belly core going to the digestive and reproductive organs passes over, embeds into, and through the psoas. When looking at issues in the gut, including IBS/SIBO, I think the psoas may be a big contributor. When fascia is unhealthy, largely due to inflammation or injury, it becomes sticky and can form adhesions. Many sources cause the inflammation that leads to adhesions, the most obvious being direct injury or trauma. Other factors include infection, repetitive movement, poor diet, toxins, poor posture and emotional stress. Because fascia provides the atmosphere through which nerve interactions happen, it responds to stress and tension. Additionally, during an injury, it’s common for fascia to constrict around the injury in order to provide structured protection, tightening the whole fascial system and potentially causing pain and discomfort in an area of the body not associated with the injury. The enteric nervous system functions without us thinking about it, but requires communication between this system and the CNS through sympathetic and parasympathetic fibers connecting the two. Through these links, the two systems can speak to each other. Generally, sympathetic stimulation (usually a stress response, indicating activity) inhibits gastrointestinal secretions and causes the digestive tract to constrict or close down. Parasympathetic stimuli (our “rest and digest” system) stimulates digestive activities.”
The bottom line is that yes, I believe that fascia can be affected by autoimmunity. In fact, I believe that it’s not terribly uncommon to see it attacked, whether via some of the known entities we discussed at the beginning of the post, or by inflammation induced by the unknown entities I touched on as well. I get slews of emails from people wondering if I can help them with _________ (insert problem here), many of which are various sorts of PAIN SYNDROMES. The things I am more likely to be able to help tend to be rather straightforward. For example, Mary gets in a car wreck, develops restriction, CHRONIC NECK PAIN (and probably HEADACHES), and contacts me to see if I think I can help. Probably so, and the cool thing is that she’ll know in a single visit (HERE or HERE).
However, when people contact me with scenarios that look like THIS ONE — pain all over the place, and a wide array of problems (like some of THESE) — the odds that I can solve your problem without dramatic FM INTERVENTION shrink dramatically. The beautiful thing is that you can help yourself (I have provided a generic protocol HERE).
My rule of thumb (which is not always hard and fast) is that when people have known autoimmune diseases and/or pain that is both above and below the waist and on both sides of the body, I start thinking systemic issues such as autoimmunity (SYSTEMIC FASCIAL ADHESIONS among others). If this is the case, underlying drivers of inflammation must be addressed before TISSUE REMODELING is really going to help. Once you realize that there are those who believe that problems with fascia are the root of all sickness, disease, and pain, this post starts to make even more sense (HERE). If you know anyone who needs to see this material, be sure and get it in front of them by emailing them a link of showing us some love on FACEBOOK.

2 Responses
Fabulous. After much research, mainly on myself (autoimmune issues like crohns) I’ve found such a huge link between psyche and the inflammatory nature of my suggested condition. Do you have more articles or studies I might read around this as I’m fascinated. Thanks!
Thanks Christine, be sure and follow some of those links under autoimmunity or simply use the search feature to find what you are after. Tons of stuff right up your alley!