YOUR MICROBIOME IS THE NUMBER ONE FACTOR WHEN IT COMES TO YOUR HEALTH
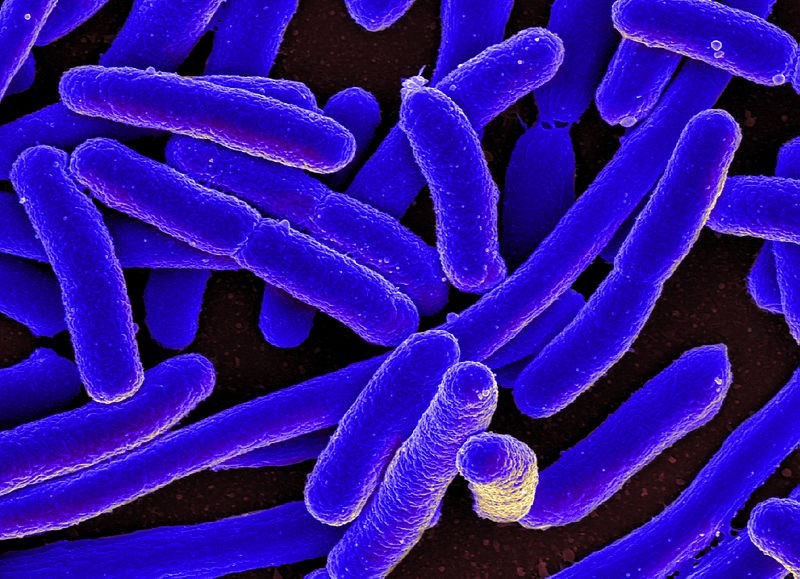
It is my strongly held belief that the single most important area of study in the field of medicine is the MICROBIOME (and intimately related to it, FMT). In fact, not a day goes by without dozens of scientific articles and peer-reviewed studies hitting the world wide web. Despite these huge advances on the academic side of medicine, LITTLE SEEMS TO BE CHANGING as far as the practice of medicine goes, as doctors continue to prescribe “Microbiome-Busting” drugs (ANTIBIOTICS, PPI’s, and ‘OTHERS‘) at record or near-record rates.
“We predict that Earth is home to upward of 1 trillion microbial species. Microbial biodiversity seems greater than ever anticipated yet predictable from the smallest to the largest microbiome.”From the abstract of Scaling Laws Predict Global Microbial Diversity from the March issue of the Proceedings of the National Academy of Sciences of the United States of America
Case in point, an article by Karen Weintraub from last week’s edition of Scientific American (Findings from the Gut—New Insights into the Human Microbiome). In this article she addresses many of the same things I have addressed under the category of GUT HEALTH. She talks about any number of diseases and their links to the Microbiome. She talks to DR. MARTIN BLASER — one of America’s foremost experts on the damage we are doing at a population level with antibiotics and author of Missing Microbes: How the Overuse of Antibiotics Is Fueling Our Modern Plagues — about the devastation being wreaked on our collective microbiomes via antibiotics. In essence she is sounding the alarm.
To give you an idea of how big this issue really is, I am going to show you some studies linking the health of your Microbiome to any number of health problems — some of them so seemingly unrelated that if you didn’t see it in black and white, you might not believe it. Most of these studies were published in the last several weeks, with none being older than March (one is February) of this year. As is always the case, results are cherry-picked due to restraints on time and space.
- WHEN IT COMES TO HEALTHY MICROBIOME, DIET MATTERS: This is sort of a no-brainier — particularly considering we already know that sugar feeds infection; dysbiosis included (HERE). The March issue of Molecular Metabolism (A Healthy Gastrointestinal Microbiome is Dependent on Dietary Diversity) revealed that, “Like all healthy ecosystems, richness of microbiota species characterizes the GI microbiome in healthy individuals. Conversely, a loss in species diversity is a common finding in several disease states. The more diverse the diet, the more diverse the microbiome and the more adaptable it will be to perturbations. Unfortunately, dietary diversity has been lost during the past 50 years and dietary choices that exclude food products from animals or plants will narrow the GI microbiome further.” What does this mean for those kids who eat nothing but CHICKEN NUGGETS, toast, grilled cheese sandwiches, and hotdogs? This month’s issue of Trends in Endocrinology and Metabolism (The Fiber Gap and the Disappearing Gut Microbiome: Implications for Human Nutrition) answers this by concluding that, “Increasing evidence indicates that modern lifestyle, and specifically a Western diet, has led to a substantial depletion of the human gut microbiome. This loss is implicated in the rampant increase of chronic diseases, providing an incentive to fundamentally transform human nutrition towards being more holistic and microbiome-focused.” Stand up and pay attention folks — this conclusion came from a mainstream medical journal; not Mother Earth News. If you are not playing the part of the parent in your relationship with your younger children (educating them and making their food choices for them), you are most likely DESTROYING THEIR HEALTH in ways they well probably never completely recover from. Oh; and as for FIBER — it’s a big part of the food source (“prebiotic”) for your Microbiome.
- WHEN IT COMES TO A HEALTHY MICROBIOME, DIET MATTERS PART II: Numerous studies similar to the June 2016 issue of Current Opinion in Allergy and Clinical Immunology (Breastfeeding and Perinatal Exposure, and the Risk of Asthma and Allergies) have been introduced to the public in recent years. After talking about numerous things that either help or harm the developing infant’s Microbiome, this study states, “A diverse range of exposures were associated with allergic disease risk, highlighting the susceptibility of children during the perinatal period. Clinicians should reinforce public health messages concerning maternal obesity, smoking, and breastfeeding. The infant gut microbiome is emerging as an important hypothesis, which may mediate the relationship between many perinatal exposures and allergic disease.” These “EXPOSURES” are one of the reason that many experts believe that as a society, we are too clean — both on the inside and the outside (more to come on this topic of hygiene shortly). Another study — this one from last month’s issue of Genome Medicine (The Influence of a Short-Term Gluten-Free Diet on the Human Gut Microbiome) talked about the effects of GLUTEN on the Microbiome, stating that, “A gluten-free diet (GFD) is the most commonly adopted special diet worldwide. It is an effective treatment for coeliac disease and is also often followed by individuals to alleviate gastrointestinal complaints. It is known there is an important link between diet and the gut microbiome…. 21 predicted pathway activity scores showed significant association to the change in diet. We observed strong relations between the predicted activity of pathways and biomarker measurements. A GFD changes the gut microbiome.” This is not news to those who have been following my site for any length of time. Knowing this information makes it easier to understand why both Gluten and Autoimmune Diseases are so heavily linked to each other as well as to one’s Microbiome (HERE).
- MICROBIOME AND KIDNEY STONES / KIDNEY DISEASE: This study from last week’s issue of Urolithiasis — a journal especially devoted to doctors who specialize in kidney stones (Evidence for a Distinct Gut Microbiome in Kidney Stone Formers Compared to Non-Stone Formers) revealed that urinary Dysbiosis was linked to forming kidney stones. “These preliminary studies for the first time associate differences in the gut microbiome with kidney stone formation.” For the record, there are any number of studies on various forms of Kidney Disease as they relate to one’s Microbiome. Case in point, a study from last week’s issue of Pediatric Nephrology (Gut Microbiome and Kidney Disease: A Bidirectional Relationship). “Here, we review changes in the host-microbiome symbiotic relationship in an attempt to explore the bidirectional relationship in which alterations in the microbiome affect kidney disease progression and how kidney disease may disrupt a balanced microbiome.“
- MICROBIOME AND ALLERGIC DISEASE / ASTHMA: Last week’s issue of the European Journal of Otorhinolaryngology (The Possible Mechanisms of the Human Microbiome in Allergic Diseases) specifically looked at the relationship between, “microbiome, dysbiosis, allergy, allergic rhinitis, and allergic disease.” Their conclusions provided a great overview of this topic. “The microbiome is the genetic material of all microbes (bacteria, fungi, protozoa, and viruses) that live on or in the human body. Microbes outnumber human cells in a 10:1 ratio. Most microbes live in the gut, particularly the large intestine. Changes in the immune function of the respiratory tract are (at least in theory) linked to the immunomodulatory activity of the gut microbiota. The gut microbiota shapes systemic immunity, thus affecting the lung mucosa. Alternatively, changes in the gut microbiota may reflect alterations in the oropharyngeal microbiota, which may in turn directly affect the lung microbiota and host immune responses via microaspiration. Dysbiosis is defined as qualitative and quantitative changes in the intestinal flora; and modern diet and lifestyle, antibiotics, psychological and physical stress result in alterations in bacterial metabolism, as well as the overgrowth of potentially pathogenic microorganisms. All immune system components are directly or indirectly regulated by the microbiota. The nature of microbial exposure early in life appears to be important for the development of robust immune regulation; disruption of either the microbiota or the host response can trigger chronic inflammation. Dysbiosis is also an important clinical entity. Antibiotics, psychological and physical stress, and dietary factors contribute to intestinal dysbiosis.” This, folks, is why ASTHMA is so heavily linked to antibiotics taken in infancy / childhood. The March issue of the Annals of the American Thoracic Society (Gut Microbiota and Allergic Disease. New Insights) came to almost identical conclusions. “The rapid rise in childhood allergies (atopy) in Westernized nations has implicated associated environmental exposures and lifestyles as primary drivers of disease development. Culture-based microbiological studies indicate that atopy has demonstrable ties to altered gut microbial colonization in very early life. Infants who exhibit more severe multisensitization to food- or aero-allergens have a significantly higher risk of subsequently developing asthma in childhood. Hence an emerging hypothesis posits that environment- or lifestyle-driven aberrancies in the early-life gut microbiome composition and function represent a key mediator of childhood allergic asthma.“
- MICROBIOME AND BRAIN / NEUROLOGICAL FUNCTION: Almost nowhere are there more studies on the microbiome than the area of NEUROLOGICAL & BRAIN HEALTH. This month’s issue of Clinical Psychopharmacology and Neuroscience (The Microbiome and Mental Health: Looking Back, Moving Forward with Lessons from Allergic Diseases) takes up where the last bullet point left off. “Relationships between gastrointestinal viscera and human emotions have been documented by virtually all medical traditions known to date. In particular, we pay specific attention to how the hygiene hypothesis and emerging research on traditional dietary patterns has helped re-ignite interest in the use of microbes to support mental health. At present, the application of microbes and their structural parts as a means to positively influence mental health is an area filled with promise. Impediments that could block translation of encouraging experimental studies include environmental forces that work toward dysbiosis, perhaps none more important than westernized dietary patterns. The microbiome is intimately connected to diet, nutrition, and other lifestyle variables; microbial-based psychopharmacology will need to consider this contextual application, otherwise the ceiling of clinical expectations will likely need to be lowered.” Re-read that last sentence and grasp the magnitude of what’s being said. No matter what sort of drugs Big Pharma comes up with (HERE), they will not ultimately be able to surmount a CRAPPY DIET.
- MICROBIOME AND BRAIN / NEUROLOGICAL FUNCTION PART II: In a study from last month’s issue of Molecular Psychiatry (From Gut Dysbiosis to Altered Brain Function and Mental Illness: Mechanisms and Pathways) we see more of the same. “The human body hosts an enormous abundance and diversity of microbes, which perform a range of essential and beneficial functions. We know, for example, that animals raised in a germ-free environment exhibit substantially altered immune and metabolic function, while the disruption of commensal microbiota in humans is associated with the development of a growing number of diseases. Evidence is now emerging that, through interactions with the gut-brain axis, the bidirectional communication system between the central nervous system and the gastrointestinal tract, the gut microbiome can also influence neural development, cognition and behavior, with recent evidence that changes in behavior alter gut microbiota composition, while modifications of the microbiome can induce depressive-like behaviors. Although an association between enteropathy and certain psychiatric conditions has long been recognized, it now appears that gut microbes represent direct mediators of psychopathology.” Not surprisingly, the March issue of the journal Frontiers in Microbiology published a similar study called Gut Microbiota: The Brain Peacekeeper. They concluded that, “Gut microbiota regulates intestinal and extraintestinal homeostasis. Accumulating evidence suggests that the gut microbiota may also regulate brain function and behavior. Results from animal models indicate that disturbances in the composition and functionality of some microbiota members are associated with neurophysiological disorders, strengthening the idea of a microbiota-gut-brain axis and the role of microbiota as a “peacekeeper” in the brain health.“
- MICROBIOME, INFLAMMATION & BRAIN FUNCTION PART III: Last July’s issue of Nature Medicine (Inflammasomes: Mechanism of Action, Role in Disease, and Therapeutics) described the “Inflammasome” thusly: “The inflammasomes are innate immune system receptors and sensors that regulate the activation of and induce inflammation in response to infectious microbes and molecules derived from host proteins. They have been implicated in a host of inflammatory disorders. Additionally, increasing evidence in mouse models, supported by human data, strongly implicates an involvement of the inflammasome in the initiation or progression of diseases such as metabolic disorders and neurodegenerative diseases.” In other words, the Inflammasome might best be thought of as ‘pre-inflammation’. A study from last month’s Molecular Psychiatry (Inflammasome Signaling Affects Anxiety and Depressive-Like Behavior and Gut Microbiome Composition) revealed that, “The inflammasome is hypothesized to be a key mediator of the response to physiological and psychological stressors, and its dysregulation may be implicated in major depressive disorder. Inflammasome activation causes the maturation of proinflammatory cytokines involved in neuroimmunomodulation, neuroinflammation and neurodegeneration…. Our results suggest that the protective effect of caspase-1 inhibition involves the modulation of the relationship between stress and gut microbiota composition, and establishes the basis for a gut microbiota-inflammasome-brain axis, whereby the gut microbiota via inflammasome signaling modulate pathways that will alter brain function, and affect depressive- and anxiety-like behaviors.” What is Capsase-1 ? According to the venerable Wikipedia it’s, “an enzyme that proteolytically cleaves other proteins, such as the precursor forms of the inflammatory cytokines…. It plays a central role in cell immunity as an inflammatory response initiator. Once activated by an inflammasome complex, it initiates a two-fold inflammation response through the initiation of pyroptosis, a programmed cell death pathway.”
- MICROBIOME AND BRAIN PART IV — PARKINSON’S DISEASE: Because it hits so close to home (HERE), I am going to at least mention Parkinson’s Disease here. Last month’s issue of Future Medicine published a study called Can Microbiota Research Change Our Understanding of Neurodegenerative Disorders?. After mentioning things like ALZHEIMER’S, Parkinson’s, and Lou Gherig’s Disease (ALS) by name, the author stated of them that, “no effective disease-modifying treatments are available.” In other words, there are no drugs that effectively treat these diseases. But here is hope if you are willing to step outside the box. A study from Parkinsonism Related Disorders (Microbiota-Gut-Brain Signalling in Parkinson’s Disease: Implications for Non-Motor Symptoms) has some interesting things to say about this common and devastating disease as it relates to one’s Microbiome. “Parkinson’s disease is the second most common neurodegenerative disorder, affecting 1-2% of the population over 65 years of age. The primary neuropathology is the loss of midbrain dopaminergic neurons, resulting in characteristic motor deficits, upon which the clinical diagnosis is based. However, a number of significant non-motor symptoms (NMS) are also evident that appear to have a greater impact on the quality of life of these patients. In recent years, it has become increasingly apparent that neurobiological processes can be modified by the bi-directional communication that occurs along the brain-gut axis. The microbiota plays a key role in this communication throughout different routes in both physiological and pathological conditions. Thus, there has been an increasing interest in investigating how microbiota changes within the gastrointestinal tract may be implicated in health and disease including PD.“
- MICROBIOME AND HIGH BLOOD PRESSURE: One of the many things we’ve learned about Gut Health from DR. ART AYERS is that one’s Microbiome makes all sorts of nutrients and chemicals needed by your body, including Vitamins (see link). In cases of Dysbiosis, the Microbiome makes bad things. These metabolic products of your bacteria, whether good or bad, make up what is known as your “metablome”. A study from the March issue of BioMed Research International (A Nested Case-Control Study of Association between Metabolome and Hypertension Risk) sheds light on how critical this phenomenon is by revealing that, “Among the 241 metabolites identified in this study, baseline levels of 26 metabolites were significantly different between hypertension and control groups. After adjusting for body mass index, smoking, and drinking, 16 out of the 26 metabolites were still associated with hypertension risk…. Higher level of a fermentation product of gut microbes was associated with higher risk of hypertension. Our study identified multiple metabolites that associated with hypertension risk. These findings implied that… gut microbiome might play an important role in the pathogenesis of hypertension.“
- MICROBIOME AND BREAST CANCER: In case you weren’t aware, I have written an awful lot of posts on BREAST CANCER. A study from last month’s issue of the Journal of the National Cancer Institute (The Intestinal Microbiome and Estrogen Receptor-Positive Female Breast Cancer) came to some interesting conclusions in this arena. “The huge communities of residential microbes, including bacteria, viruses, Archaea, and Eukaryotes, that colonize humans are increasingly recognized as playing important roles in health and disease. In health, the function of the microbiome might be considered to be in dynamic equilibrium with the host, exerting both local and distant effects. However, ‘disequilibrium’ [dysbiosis] may contribute to the emergence of disease, including malignancy. In this review, we discuss how the intestinal bacterial microbiome and in particular how an ‘estrobolome,’ the aggregate of enteric bacterial genes capable of metabolizing estrogens, might affect women’s risk of developing postmenopausal estrogen receptor-positive breast cancer. Estrobolome composition is impacted by factors that modulate its functional activity.” Did you catch that? My best guess is that someone like Art Ayers would tell us that certain foods (broccoli for instance) that feed the P-450 CYTOCHROME SYSTEM are not themselves cleaning out estrogen (not to mention XENOESTROGENS), but are actually feeding the bacteria that do it.
- THE MICROBIOME AND CANCER IN GENERAL: Considering that 80% of your Immune System is found in your Gut (HERE), it should come as no surprise that Dysbiosis is related to all forms of CANCER. Last month’s issue of the World Journal of Clinical Oncology (Role of the Microbiome in Non-Gastrointestinal Cancers) had something to say about this. “Disruption in the microbiome composition, termed dysbiosis, is mirrored by the development of pathologies in the host. Among the most serious consequences of dysbiosis, is the development of cancer. As many as 20% of total cancers worldwide are caused by a microbial agent. To date, a vast majority of microbiome-cancer studies focus solely on the microbiome of the large intestine and the development of gastrointestinal cancers. Here, we will review the available evidence implicating microbiome involvement in the development and progression of non-gastrointestinal cancers, while distinguishing between viral and bacterial drivers of cancer, as well as “local” and “systemic”, “cancer-stimulating” and “cancer-suppressing” effects of the microbiome.” I showed you earlier in this post that sugar feeds infection / dysbiosis. Should we not be surprised then that SUGAR FEEDS CANCER as well? It’s not like this is new information. Germany’s Dr. Otto Warburg won the Nobel Peace Prize for figuring this out ten years prior to our entry into WWII (1931).
- MICROBIOME AND CHEMOTHERAPY: In this interesting study (Pretreatment Gut Microbiome Predicts Chemotherapy-Related Bloodstream Infection) that was published in last week’s edition of Genome Medicine, we see that, “Bacteremia, or bloodstream infection (BSI), is a leading cause of death among patients with certain types of cancer. A previous study reported that intestinal domination, defined as occupation of at least 30 % of the microbiota by a single bacterial taxon, is associated with BSI in patients undergoing allo-HSCT (stem cell transplantation). We found that patients who developed subsequent BSI exhibited decreased overall diversity and decreased abundance of taxa… These results suggest that the gut microbiota can identify high-risk patients before HSCT and that manipulation of the gut microbiota for prevention of BSI in high-risk patients may be a useful direction for future research.“
- MICROBIOME AND SYSTEMIC ARTHRITIS (RHEUMATOID): A study from last month’s issue of Genome Medicine (An Expansion of Rare Lineage Intestinal Microbes Characterizes Rheumatoid Arthritis) provided some details on something we knew years ago — that RHEUMATOID ARTHRITIS is associated with gut bacteria. “The adaptive immune response in rheumatoid arthritis (RA) is influenced by an interaction between host genetics and environment, particularly the host microbiome. Association of the gut microbiota with various diseases has been reported, though the specific components of the microbiota that affect the host response leading to disease remain unknown. Patients with RA exhibited decreased gut microbial diversity compared with controls, which correlated with disease duration and autoantibody levels. A taxon-level analysis suggested an expansion of rare taxa, with a decrease in abundant taxa in patients with RA compared with controls.” One of these ‘rare‘ taxa (Collinsella), “correlated strongly with production of the proinflammatory cytokine IL-17A. A role for Collinsella in altering gut permeability and disease severity was confirmed in experimental arthritis.” Did you catch that? Not only do these dysbiotic bacteria create INFLAMMATION, they lead to CHANGES IN INTESTINAL PERMEABILITY (aka a “Leaky Gut”). “These observations suggest dysbiosis in RA patients resulting from the abundance of certain rare bacterial lineages.”
- MICROBIOME AND CHRONIC PAIN: At February’s 32nd annual meeting of the American Academy of Pain Medicine, Dr. Gerald Mullin gave a talk to pharmacists called The Gut Balance Revolution. Among other things the transcript of his lecture says that, “Agents and diets that perturb the gut microbiome can incur a heavy price, leading to diabetes, obesity, nonalcoholic fatty liver disease, dementia, and cardiovascular disease. Noting the general principle that increased species diversity increases an ecosystem’s efficiency and productivity while making it less functionally susceptible to external stressors, he pointed out that gut microbiome diversity helps with barrier integrity and with training the immune system, and overall has a great impact on health and well-being. Factors contributing to dysbiosis of the gut microbiota include host genetics, lifestyle (e.g., diet, stress), reduced early colonization (e.g., hospital birth, altered microbe exposure), and medical practices (e.g., vaccination, antibiotics, excessive hygiene).” This, folks, is a true mind bender. We have a mainstream MD, lecturing pharmacists about the HYGIENE HYPOTHESIS and the fact that VACCINES HAVE THE ABILITY TO DESTROY GUT HEALTH (or HERE). He then went on to talk about the way that PPI DRUGS are causing dysbiotic problems like C. DIFF and SIBO. He goes on to say about people’s ability to get back to normal after taking a round of antibiotics, “Recovery of gut biodiversity after a week’s course of clindamycin, a regimen commonly prescribed for dental procedures, may take up to two years. Furthermore, it has been proposed that subtherapeutic levels of antibiotics lead to increased adiposity [obesity]. One study showed that repeated exposure to broad-spectrum antibiotics at ages zero to 23 months is associated with early childhood obesity.” I actually have several studies on my site that show this last sentence to be true. Oh, he did eventually get around to mentioning CHRONIC PAIN in his talk as well.
- MOM’S USE OF ANTIBIOTICS WHILE PREGNANT OR NURSING ADVERSELY AFFECTS HER BABY: A study from last month’s Journal of Immunology (Maternal Antibiotic Treatment Impacts Development of the Neonatal Intestinal Microbiome and Antiviral Immunity) was a smack in the face to doctors who OVER-PRESCRIBE ANTIBIOTICS to pregnant or lactating mothers. “Microbial colonization of the infant gastrointestinal tract (GIT) begins at birth, is shaped by the maternal microbiota, and is profoundly altered by antibiotic treatment. Antibiotic treatment of mothers during pregnancy influences colonization of the GIT microbiota of their infants. Maternal antibiotic treatment/treated (MAT) during pregnancy and lactation resulted in profound alterations in the composition of the GIT microbiota in mothers and infants. Streptococcus dominated the GIT microbiota of MAT mothers, whereas Enterococcus faecalis predominated within the MAT infant GIT. MAT infant mice subsequently exhibited increased and accelerated mortality following vaccinia virus infection. We additionally determined that control infant mice became more susceptible to infection if they were born in an animal facility using stricter standards of hygiene. These data indicate that undisturbed colonization and progression of the GIT microbiota during infancy are necessary to promote robust adaptive antiviral immune responses.” Are you catching some of this folks? Can anyone say TOO CLEAN?
- ARTIFICIAL SWEETENERS DESTROY YOUR MICROBIOME: The March issue of Physiology & Behavior published a study called Low Calorie Sweeteners and Gut Microbiota. “Studies dating back to 1980s, using bacterial cultures, have reported associations between low calorie sweeteners (LCS) and alterations in bacterial composition, raising the potential that LCS might exert effects on the host via interactions with gut microbiota.” This is the very reason that even though they have zero calories, DIET SODA’S cause double the weight gain (mostly in the form of BELLY FAT) that regular sodas do (HERE).
- MICROBIOME AND IRRITABLE BOWEL SYNDROME / FODMAPS: We’ve known for quite sometime that FODMAPS are intimately related to IBS. A study in the March issue of Gut (FODMAPs Alter Symptoms and the Metabolome of Patients with IBS: A Randomized Controlled Trial) helped us better understand why. “To gain mechanistic insights, we compared effects of low fermentable oligosaccharides, disaccharides and monosaccharides and polyols (FODMAP) and high FODMAP diets on symptoms, the metabolome and the microbiome of patients with IBS. IBS symptoms are linked to FODMAP content and associated with alterations in the metabolome. In subsets of patients, FODMAPs modulate histamine levels (reduced eightfold in the low FODMAP group) and the microbiota, both of which could alter symptoms.“
- MICROBIOME AND GUT FAILURE CAN LEAD TO DEATH: Last month’s issue of Critical Care Clinics (The Gut as the Motor of Multiple Organ Dysfunction in Critical Illness) talked a bit about what happens in an ICU setting. “All elements of the gut – the epithelium, the immune system, and the microbiome – are impacted by critical illness and can, in turn, propagate a pathologic host response leading to multiple organ dysfunction syndrome. Studies have demonstrated that this can occur by release of toxic gut-derived substances into the mesenteric lymph where they can cause distant damage. Further, intestinal integrity is compromised in critical illness with increases in apoptosis [inflammatory mediators that cause programmed cell death] and permeability [Leaky Gut — something we have been aware of for at least two decades — HERE]. There is also increasing recognition that microbes alter their behavior and can become virulent based upon host environmental cues [H. PYLORI is probably the best example of this phenomenon]. Gut failure is common in critically ill patients…“
Truthfully, this post is just barely scratching the surface of how big this whole Microbiome thing really is. The real question, however, is not where you can find more research. The real question is what can a person do who knows they have one or both sides of the coin that is fouled up Gut Health (Dysbiosis and / or Increased Intestinal Permeability)? I’m glad you asked. About six months ago I created a post called HOW TO HEAL YOUR DAMAGED GUT — and it’s totally free.
