HOW THE PAIN AND DYSFUNCTION OF THE WHIPLASH-INJURED NECK AFFECTS THE BRAIN
An article by Julie Beck in a 2016 issue of The Atlantic (Chronic Whiplash is a Medical Mystery) was quoting professor of medicine, Dr. Robert Ferrari as she said…
“That people can experience neck, head, and back pain after a car accident, or some other kind of neck energy transfer is not in doubt. What is unclear is whether such an energy transfer can cause chronic, long-lasting pain, and if so, how. And there is still no established physical reason why a whiplash injury would cause chronic pain. Given that, and given the involvement of insurance companies in car accidents, it would be easy to think a lot of these ongoing whiplash cases are scams fabricated to get a payout.
But Ferrari thinks only a very small percentage are malingering. The difference, Ferrari thinks, is whether the country in question has a whiplash culture. Whiplash cultures are those cultures in which there is the expectation that if you’ve been in a motor vehicle collision, you’ll probably have some significant problem as a result.”
So basically, this article from a huge national publication is saying that no, you’re not making it up. The pain is real (at least to you it’s real). But it’s all in your head. While I would never say that there is not at least some degree of psychosomatic issue with whiplash (“psychosomatic” are illnesses or pain brought on or aggravated by mental factors such as worry or stress), the truth is, there’s arguably some degree of psychosomatic with every disease or injury.
So today I want to take a look at how WHIPLASH INJURIES might by causing the far-reaching and seemingly unrelated symptoms that so often get suffering individuals labeled as scam artists, malingers, or money-grubbers by the other party’s insurance company (and quite frequently — at least in an unspoken fashion — by their own attorney).
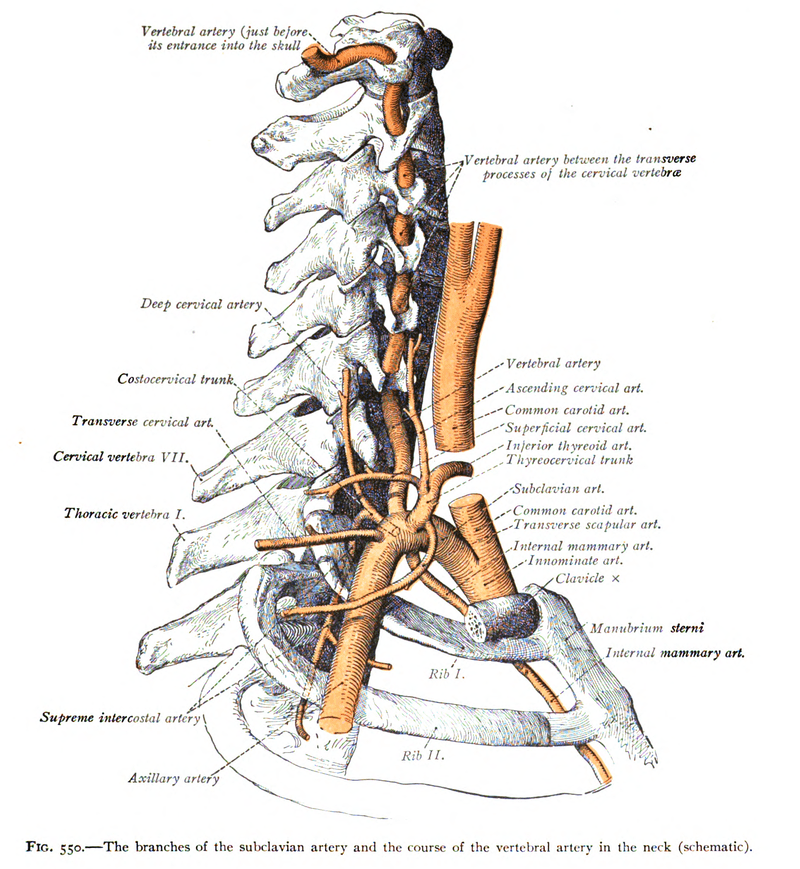
One of the things that you will almost always find with people who have been in WHIPLASH ACCIDENTS is that their cervical ranges of motion are diminished — often times very dramatically (but occasionally not at all — HERE). A study from earlier this summer (published in the Archives of Physical Medicine and Rehabilitation) asked a question via its title; To What Degree Does Active Cervical Range of Motion Differ Between Patients With Neck Pain, Patients With Whiplash, and Those Without Neck Pain?
The authors, six European researchers and physicians, looked at 27 studies that pertained to 2,700 subjects, concluding that “Patients with neck pain have a significantly decreased active cervical ROM compared with persons without neck pain, and patients with whiplash-associated disorders (WAD) have less active cervical ROM than those with nontraumatic neck pain.” While this is nice to see in black and white, any practicing chiro or bodyworker could have told you this.
Any time there are decreases in ranges of motion, there will be a corresponding loss of proprioception (HERE). While this might not seem like a big deal up front, it’s a huge deal because loss of proprioception is not only intimately associated with spinal degeneration (HERE), it’s directly linked to most chronic disease processes (HERE) as well as chronic pain. Speaking of chronic pain and whiplash; earlier this month a practicing anesthesiologist wrote a scientific paper for Anesthesia & Analgesia (Whiplash Injury: Perspectives on the Development of Chronic Pain) that concluded….
“Whiplash is largely a compression injury when the trunk is forced upwards into the cervical spine. Most frequently due to motor vehicle collision and often associated with considerable pain, suffering, disability, and cost, whiplash-associated injury is a debilitating and common form of neck pain with a range of clinical manifestations including neck, shoulder, and back pain, numbness, fatigue, nausea, cognitive deficits, and low self-reported physical and mental health.
The complex neurobiological interplay between intraarticular nociception [pain from various pathways] and the neuroimmune and neuroplastic effects of ongoing joint injury are illustrated with a pathway approach. Myriad motor and sensorimotor dysfunctions can manifest from WAD… WAD is used as a model for other pain syndromes in which imaging studies prove negative even though patients suffer profound disability.”
Although this sounds somewhat disjointed because I cherry-picked it due to time and space requirements as I do many quotes I use, notice some of their conclusions. Most of us tend to think of whiplash as a stretching / tearing sort of injury — this guy says it’s compressive (the facets in the rear of the spinal column are undoubtedly compressed as the body is driven out from under the head — the facets make up the IVF which is the small window the spinal nerves exit from).
Also note that there are numerous pathways to chronic pain. And finally, realize that the author mentions the whole imaging conundrum — soft tissues and connective tissues (fascia included) don’t show up will with standard advanced imaging (although that is SLOWLY IMPROVING at least with fascia, although I am not sure about CERVICAL FASCIA). But it doesn’t end here. Not by a long shot. As we got a small taste of in this study, chronic pain leads to some rather funky sensory and motor problems.
A study from earlier this summer was published in JOSPT (Dizziness, Unsteadiness, Visual Disturbances, and Sensorimotor Control in Traumatic Neck Pain) dealing with this very issue.
“There is considerable evidence to support the importance of cervical afferent dysfunction in the development of dizziness, unsteadiness, visual disturbances, altered balance, and altered eye and head movement control following neck trauma, especially in those with persistent symptoms….
The evaluation of potential impairments (altered cervical joint position and movement sense, static and dynamic balance, and ocular mobility and coordination) should become an essential part of the routine assessment of those with traumatic neck pain, including those with concomitant injuries such as concussion and vestibular or visual pathology or deficit.”
The study goes on to talk about these factors in relationship to proprioceptive loss, as well as the extensive manner they adversely affect motor function, coordination, and control.
“Joint position sense (JPS) is defined as the ability to relocate the natural head position without the assistance of vision. Greater errors have been shown in individuals with both idiopathic neck pain [not sure which tissue the pain is originating from or why it’s there] and persistent WAD, although errors are greater in those with neck trauma, especially in those with moderate to severe pain and disability.
Further, persistent WAD and symptoms of dizziness had greater errors than those not complaining of dizziness, suggesting that these symptoms may be due to greater abnormal cervical afferent [sensory] input.”
What do these people do with the pain and what is the single biggest factor in determining outcomes? Can anyone say “Pain Avoidance”? According to April’s issue of Acta Anesthesiologica Scandinavica (Pain Avoidance Predicts Disability and Depressive Symptoms Three Years Later in Individuals with Whiplash Complaints).
“Longstanding symptoms due to whiplash are commonly associated with decreased levels of emotional and physical functioning. Psychological inflexibility, and more specifically avoidance, was a unique predictor of pain disability and depressive symptoms, also when controlling for background variables, pain related variables and psychological distress. Level of education was also found to predict both pain disability and symptoms of depression.
Lastly, pain variability predicted pain disability, and anxiety predicted depressive symptoms. Pain avoidance significantly predicted pain disability and depressive symptoms 3 years later. Although tentative, results warrant more studies to further explore the importance of pain avoidance for future health.”
What exactly are “pain avoidance” and “psychological inflexibility”?
Pain avoidance is just what it sounds like — trying to avoid pain. People in chronic pain, however, are forced to make daily decisions like this; I really should be a good dad and go play basketball with my son, but I know that it will fire up my chronic foot issue and I will suffer for three days.
Psychological inflexibility is loosely defined as being so rigid in our thoughts, feelings, and emotions that we cannot change them for the longer term good. Psychological inflexiblity goes along with pain avoidance and is heavily associated with things like ANXIETY, DEPRESSION, SICKNESS & DISEASE, learning disabilities, poor work performance, WORRY & STRESS, SUBSTANCE ABUSE, as well as a lower quality of life. All of these things and others can potentially lead people into something known as Central Sensitization.
Central Sensitization: Where Chronic Pain’s “Rubber” Meets the Road in Whiplash Injured Patients

If you want to read more about CENTRAL SENSITIZATION, follow the link as I have several posts on the subject. The Institute for Chronic Pain (What is Central Sensitization?) says of Central Sensitization (cherry-picked as are many of my quotes)…..
“Central sensitization is a condition of the nervous system that is associated with the development and maintenance of chronic pain. When central sensitization occurs, the nervous system… gets regulated in a persistent state of high reactivity. This persistent, or regulated, state of reactivity lowers the threshold for what causes pain and subsequently comes to maintain pain even after the initial injury might have healed.
Central sensitization has two main characteristics. They are called allodynia and hyperalgesia. Allodynia occurs when a person experiences pain with things that are normally not painful. Hyperalgesia occurs when a stimulus that is typically painful is perceived as more painful than it should. Chronic pain patients can sometimes report sensitivities to light, sounds and odors.
Central sensitization is also associated with cognitive deficits, such as poor concentration and poor short-term memory. Central sensitization also corresponds with increased levels of emotional distress, particularly anxiety. Lastly, central sensitization is also associated with sick role behaviors, such as resting and malaise, and pain behavior.
Central sensitization can occur with chronic low back pain, chronic neck pain, whiplash injuries, chronic tension headaches, migraine headaches, rheumatoid arthritis, osteoarthritis of the knee, endometriosis, injuries sustained in a motor vehicle accident, and after surgeries. Fibromyalgia, irritable bowel syndrome, and chronic fatigue syndrome, all seem to have the common denominator of central sensitization as well.”
In other words, pain and neurological reactivity can get locked into the brain so that even though the original insult / injury is long gone, a “recording” of the pain continues to play on a loop. Thus, even though this pain is technically in people’s head, it is very real. The pain of Central Sensitization is not psychosomatic. Despite lots of theories as to why this occurs, no one really knows for sure, although the commonest of the common denominators seems to be INFLAMMATION — yet another reason to live an anti-inflammatory lifestyle (more to come on this shortly).
Some of you might remember that I spent some time discussing the fact that current research is showing that as many as half of all people (especially women) who are injured in a whiplash accident progress to chronic. This is borne out by a study from the January 2016 issue of BMC Public Health (Five Years After the Accident, Whiplash Casualties Still Have Poorer Quality of Life in the Physical Domain than Other Mildly Injured Casualties).
After factoring out all sorts of confounders such as PTSD, socioeconomic status, and psychological factors, these authors determined that, “deteriorated quality of life in the physical domain remained 5 years after the accident, specifically in the grade-2 whiplash group, pain playing a predominant intermediate role, which may be in line with the hypothesis of neuropathic pain.” Neuropathic pain? Can anyone say Central Sensitization?
March’s issue of Physical Therapy went on to talk about the differences in pain and recovery between the sexes (I’ve shown you before but will show you again just how big the difference really is). In a study called Differences Between Women With Traumatic and Idiopathic Chronic Neck Pain and Women Without Neck Pain: Interrelationships Among Disability, Cognitive Deficits, and Central Sensitization, the authors concluded…..
“Pain-related disability, reduced health-related quality of life, and cognitive deficits were present in participants with CWAD (chronic whiplash-associated disorders) and, to a significantly lesser extent, in participants with CINP (chronic idiopathic neck pain). Local hyperalgesia was demonstrated in participants with CWAD and CINP but not in women who were healthy.
However, distant hyperalgesia and decreased conditioned pain modulation efficacy were shown only in participants with CWAD; this result is indicative of the presence of central sensitization. Moderate to strong correlations among disability, cognitive deficits, and hyperalgesia (local and distant) were observed in participants with CWAD.”
One of the things I noticed as I read studies on the subject is that TRIGGER POINTS (especially Trigger Points in the UPPER TRAPS & LEVATOR) were frequently associated with Central Sensitivity, which was seen in a recent study from Frontiers in Neurology (An Attempt of Early Detection of Poor Outcome after Whiplash). The 12 French authors of this study were attempting to figure out what characterized the people who didn’t really recover — the people who ended up chronic. Beyond chronic TP’s,
“All chronic patients exhibited high level of catastrophizing at the acute stage and/or PTSD. Their head and trunk motor control values, and in some cases vestibular tests, are far from the healthy group. Practically speaking, the results of this study are in line with previous results and suggest that low-grade whiplash patients should be submitted as early as possible after the trauma to neuropsychological and motor control tests in a dedicated consultation.
In addition, they should be sent to a neuro-otologist for a detailed examination of vestibular functions, which should include cVEMP (cervical vestibular evoked myogenic potentials). Then, if diagnosed at risk of WAD, these patients should be submitted to an intensive preventive rehabilitation program, including vestibular rehabilitation if required.”
Although there are undoubtedly medical neurologists doing this sort of work for patients suffering from WAD, I have yet to see it.
When people are injured, if they even go to the doctor, they will be told something like, “Thank God Mrs Smith, everything looks fine. You’ll be sore for a few days, but you’ll be OK.” Since there were no blood, guts, or broken bones, you assume they have a clue what they are talking about. You are given some drugs from the “BIG FIVE” category, sent home, and told to call your family physician if you have any problems.
The problem is that simple math tells us that half of these people are walking out of the ER and into a world where pain will become their overriding thought process — the thing they think about all the time — the thing they cannot get away from (HERE is an example).
A similar study was published just last month in the journal, Pain Physician (What Are the Predictors of Altered Central Pain Modulation in Chronic Musculoskeletal Pain Populations? A Systematic Review), the reviewers said that…
“Existing studies have investigated predictors of poor outcomes associated with musculoskeletal pain, including disability and failure to return to work. However, there remains little consensus. Common to a significant proportion of chronic musculoskeletal pain populations is the phenomenon of sensitization of the central nervous system pain pathways. A strong clinical predictor of altered central pain modulation is disproportionate, non-mechanical, unpredictable pattern of pain provocation in response to multiple/non-specific aggravating/easing factors.
Altered central pain modulation is associated with many non-specific chronic musculoskeletal pain conditions and the etiology is poorly understood. It is considered by some that altered central pain modulation is a disease in itself rather than a disease of the particular presenting musculoskeletal condition. Premorbid and acute stage high sensory sensitivity and/or somatization are the strongest predictors of altered central pain modulation in chronic musculoskeletal pain to date.”
What is somatization? It’s essentially recurrent and often multiple medical symptoms that have no detectable cause. Somatization is what caused the most renowned whiplash research team on the planet (Gargan & Bannister) well over two decades ago, to say that (I am loosely quoting from memory here) “whiplash injuries often lead to bizarre and seemingly unrelated symptoms“.
And here’s just one of the many problem with all of this. If you are coming to see me for chronic hardcore WAD symptoms from one or two hours away, it’s not really a big deal. I treat you and you either get better or you don’t. If you don’t, there are any number of reasons, including Central Sensitization, that might explain why (HERE).
However, if you are flying HALFWAY ACROSS THE COUNTRY — or EVEN THE WORLD — for treatment, I do an email history in order to see if I think I can even help you, and to make your visit as productive as possible (HERE). As you have seen so far, the “consensus” is that there is not really a great way to diagnose Central Sensitization — to know for sure whether your pain is locked into your brain like an old cassette tape playing on auto-reverse. The situation, however, might be getting better.
Just five short weeks ago, a group of researchers and physicians from the orthopedics department at Duke University published a paper in Pain Practice (Measurement Properties of the Central Sensitization Inventory: A Systematic Review) where they looked at something called the CSI (Central Senstitization Inventory — a system created to determine whether or not a person has CS).
In this study, they looked at CS as related to “several medical diagnoses, including post-cancer pain, low back pain, osteoarthritis, whiplash, and fibromyalgia, comparing the results of 14 different studies to what they determined the CSI should be, trying to figure out its predictive ability to determine whether or not a person might be centralizing. Their results suggest the tool generates reliable and valid data that quantifies the severity of several symptoms of CS. Only time will tell if this is true of not, or if the tool proves to be the real McCoy.
This discussion about the brain being the source of pain is highly intriguing in light of an editorial that was published in August’s issue of a Greek journal called the Hellenic Journal of Nuclear Medicine (Whiplash Syndrome: A Disorder of the Brain?). In this paper, the authors — German engineers / MD’s — dealt with the fact that despite mountains of research from the past two decades, we still have more questions than answers. They then discussed the three main theories concerning whiplash.
- IT DOESN’T REALLY EXIST: This comes from studies published in other countries — mostly third-world countries — that claim that people who are injured in societies where no one really knows much about car crashes and are not expecting some sort of financial settlement, don’t really have chronic neck pain or WAD after motor vehicle accidents (this was roughly the assertion seen in the very beginning of today’s post). This group really does believe that the pain is all in one’s head (somatization), with zero physiological reason.
- THE NOCICEPTIVE-VASCULAR HYPOTHESIS: Remember that inflammation is always the result of some sort of tissue damage, whether caused by injury, diet, exposure to reactive foods, parasites, black mold, EMF’s, etc, et, etc. Research has shown that when soft tissues tear, INFLAMMATORY MEDIATORS are released not just locally, but into the general circulation, hypersensitizing sensory nerves, and leading to Chronic Pain (HERE).
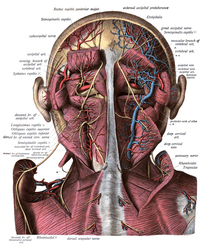
- THE MIDBRAIN HYPOTHESIS: This theory says that there is a “mismatch between aberrant information from the cervical spinal cord and the input from the vestibular [balance / inner ear] and visual systems,” that are then integrated into different parts of the midbrain. The authors go on to expound that functional MRI imaging techniques of the central nervous system consistently light up specific areas of the brain as seen with new 3-D technology (this phenomenon could be partially explained by the second bullet point in relation to something called LEAKY BRAIN SYNDROME).
“The most frequent symptoms in patients with whiplash syndrome are neck pain and headache, followed by visual and vestibular problems, cognitive limitations, and emotional disturbances. These symptoms were mostly caused by rear-end vehicle collisions while only 50% of the injured recover from initial symptoms within one year after the accident.
Interestingly, the most frequent clinical symptoms of whiplash (i.e. visual problems such as impaired spatial ability or blurred vision, or cognitive limitations such as the difficulty forming thoughts and difficulties not in attending but in disengaging once the subject has focused on an object of attention) fit with hypoperfusion of the posterior parietal occipital region.”
What is this saying? For starters, it’s reiterating what I have shown you repeatedly from peer review; that if you are injured in a whiplash-type accident, whether you fully recover or slip into chronic is essentially a coin toss — a 50/50 proposition. It also talks about the posterior occipital region of the brain (this region is in the far back area of the brain, as well as slightly in front of it). Gordon Johnson of Brain Injury Help simplifies things nicely in an article called Parietal Lobes and Occipital Lobes.
“The parietal lobes are areas for the reception and organization of language functions. The parietal lobes integrate sensory data from other parts of the body. They also play a big role in understanding numbers and their relations. Further, they have an important role in the manipulation of objects and in the processing of information relating to the sense of touch. The parietal lobes have both the left and right hemispheres.
The left side is concerned in symbolic functions in language and mathematics. The right hemisphere is more focused on images and spatial relationships. The Occipital Lobes are divided into different functional visual areas. Each area contains a map of the visual world. The Occipital Lobes are the area where specialized neurons which receive and process visual information reside. The visual pathways run from the retina to the primary visual cortex, contained within the Occipital Lobes.”
While this is certainly a bit oversimplified, it does a good job of showing why a BRAIN ISSUE in this area could affect both balance and vision (vision is critical for balance). With numerous recent medical studies calling for multidisciplinary and interdisciplinary treatment of WAD (HERE is one of many), we should be seeing more of the testing that was discussed in this study as well as earlier.
However, the only group of physicians I am aware of are doing this sort of work on a consistent basis are CARRICK-TRAINED FUNCTIONAL NEUROLOGISTS. Which brings me around to one final point; what about the settlement money at stake?
With attorneys advertising for crash victims by way of the internet, billboards, printed ads, radio, television, and any number of others (including the proverbial “ambulance chasing”), it’s clear that there is a lot of money at stake.
July’s JOSPT (The Nature of Whiplash in a Compensable Environment: Injury, Disability, Rehabilitation, and Compensation Systems) revealed that, “compensation schemes have, however, been subject to a common set of interrelated concerns, chiefly concerning the incentives, behaviors, and outcomes that may arise when financial compensation for injuries is available to injured party.” I would assume the same thing.
What’s interesting, however, is that studies on whether or not settlement dollars “affect” the severity of a person’s injury are all over the place, with the insurance industry naturally claiming that it makes a big difference, while numerous other sources consistently show that it doesn’t. “Information asymmetries between insurers and claimants, claimants and clinicians, clinicians of different types, and other dyadic interactions complicate the insurance arrangements that apply in injury compensation schemes.”
My experience after a quarter century of practice is that patient’s problems frequently continue long after the claim has been settled, regardless of the outcome of litigation. In other words, people don’t all of a sudden get well because their attorney won them a settlement (which btw, is usually far less than people are led to believe it will be).
A QUICK ANECDOTE ABOUT DIET SODA OR MSG
AND WHIPLASH-INDUCED CHRONIC NECK PAIN
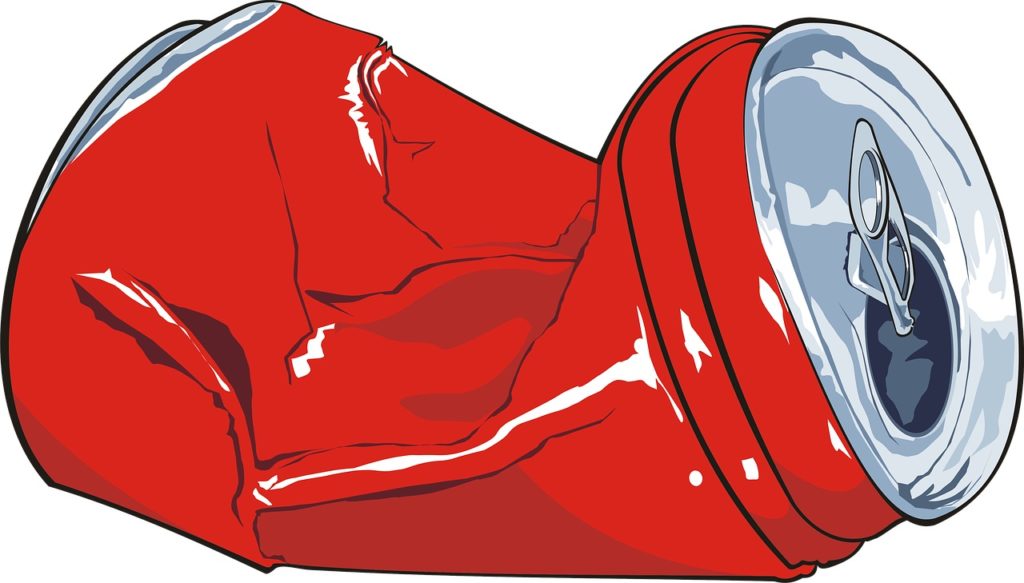
It wasn’t that long ago that I saw a patient who was truly struggling with neurological signs and symptoms of whiplash, including CHRONIC PAIN. In quizzing this person, I quickly realized that they used to be a CARB AND SODA JUNKY, but had recently gone on a DIET SODA KICK in order to try and lose weight (emphasis on the word try).
Firstly, if you have followed my site to any degree you already know that science has actually shown that people gain more weight on diet soda than regular soda (HERE). Secondly, you are probably also aware of the way that excitotoxins such as aspartame and MSG stimulate (excite) the nervous system, pain pathways included.
The internet is littered with websites and books outlining the harms of consuming MSG and NutraSweet (aspartame), particularly as related to chronic pain — my favorite is neurosurgeon Russell Blaylock’s 1994 offering, Excitotoxins: The Taste That Kills. Although studies abound, as I was looking on PubMed, a couple caught my eye.
The first, on aspartame, was published in the summer of 2014 by the University of North Dakota (Neurobehavioral Effects of Aspartame Consumption). This freaky study showed that elderly people who consumed more ASPARTAME (but were still well below the limits of what the government considers high) showed, “more irritable mood, exhibited more depression, and performed worse on spatial orientation tests.”
As for MSG, the December 2012 issue of Clinical & Experimental Rheumatology (The Effect of Dietary Glutamate on Fibromyalgia and Irritable Bowel Symptoms) linked MSG to two different AUTOIMMUNE DISEASES —- FIBROMYALGIA and IBS.
For this study 57 people with both Fibromyalgia and IBS went on an excitotoxin-free diet for a month (no MSG, aspartame, hydrolyzed protein, etc, etc, etc). The 37 people who actually made it through all four weeks were then assessed via questionnaires and pain scales. In only four weeks, one third of their symptoms resolved (that’s resolved as in bye-bye). This group was then divided into two different groups that were double-blindedly either given excitotoxins in their food three times a week for two weeks, or not.
“The MSG challenge, as compared to placebo, resulted in a significant return of symptoms; a worsening of fibromyalgia severity; decreased quality of life in regards to IBS symptoms… These findings suggest that dietary glutamate may be contributing to FM symptoms in some patients. Future research on the role of dietary excitotoxins in FM is warranted.“
I bring this issue up because I recently had a patient who had largely gone PALEO, but had not given up either NutraSweet (aspartame) or flavoring their food with an MSG-based “spice” powder. Once I convinced them to make a clean break, the results were remarkable and rapid.
Within a matter of days this individual had relieved almost all the chronic pain they were having — pain that while diagnosed as Fibro, had started shortly after a rather serious MVA. Over the years I have seen many similar cases. If you are looking for other tricks to help relieve (or better yet, reverse) inflammation and restore mechanical and neurological function to the body, HERE is the post to look at.