WHY HEAD INJURIES LEAD TO AUTOIMMUNITY AND POOR HEALTH
- Traumatic Brain Injuries are a leading cause of death and disability in both children and adults.
- Traumatic Brain Injuries are frequently related to MOTOR VEHICLE ACCIDENTS and SPORTS, however, falls and physical ABUSE are common causes as well.
- In excess of 5 million Americans are currently disabled as the result of Traumatic Brain Injury.
- Traumatic Brain Injuries have a direct cost of over 100 billion dollars annually, with an indirect cost that could be many times higher.
- Traumatic Brain Injuries dramatically increase one’s chances of Alzheimer’s and Dementia.
- Traumatic Brain Injuries are common among veterans — particularly those who served in Iraq, where IED’s were so common.
One of the biggest problems with diagnosing head injuries are the primary tools we use (CT & MRI). The problem is that not only are CT’s particularly dangerous (read the link), but rarely are they to provide ER doctors with what I refer to as “ah ha” moments (“Ah ha, Mrs. Smith; I see your problem!”). This is because the tests are looking for VISIBLE PATHOLOGY — chiefly bleeding / swelling. However, with each passing day, the research reinforces that fact that most TBI damage occurs at the cellular level. Thus, people are told they are fine when they might be anything but. The real problem is that the majority of practicing physicians are not aware of how easily head Injuries and TBI’s can open the gate leading to AUTOIMMUNITY (HERE is a list of a few Autoimmune Diseases, although there are thousands of them) and overall ill health.
If you’ve followed my blog, none of this is new (HERE, HERE, HERE, and even HERE — Pam Arnold’s hellish journey after hitting her head on a gravestone). There is, however, a veritable avalanche of new information on the topic. The study I want to talk about today is not brand new —- it came out in last March’s issue of the French medical journal PLoS One (Human Traumatic Brain Injury Induces Autoantibody Response against Glial Fibrillary Acidic Protein and Its Breakdown Products). It’s been sitting in my blog que for months, and today we are going to pick it apart.
Traumatic brain injury (TBI) is a leading cause of death and disability worldwide. The pathogenesis of TBI involves two components: the initial mechanical injury, and subsequent secondary cell death that expands the core lesion. During acute neuronal necrosis [abnormal and early nerve death], calpains [specific proteolytic enzymes] are hyper-activated, while caspases [a different proteolytic ennzyme] are activated in apoptosis [normal or “programmed” cellular death].
When tissue is injured or compromised, the cells that take the brunt of the injury are killed (necrosis). Dead cells rupture their contents, causing a massive ACUTE INFLAMMATORY RESPONSE. Among other things, this response will attract fluid to the area in the form of swelling (edema). Because we know the approximate rate of Cellular Apoptosis — normal cellular death at the end of a normal life cycle (approximately 60 billion cells per day in a normal adult) —- there should be a fairly consistent ratio of Caplains to Caspases in the blood. That is, until massive amounts of very specific Caplains are released into the bloodstream following a TBI.
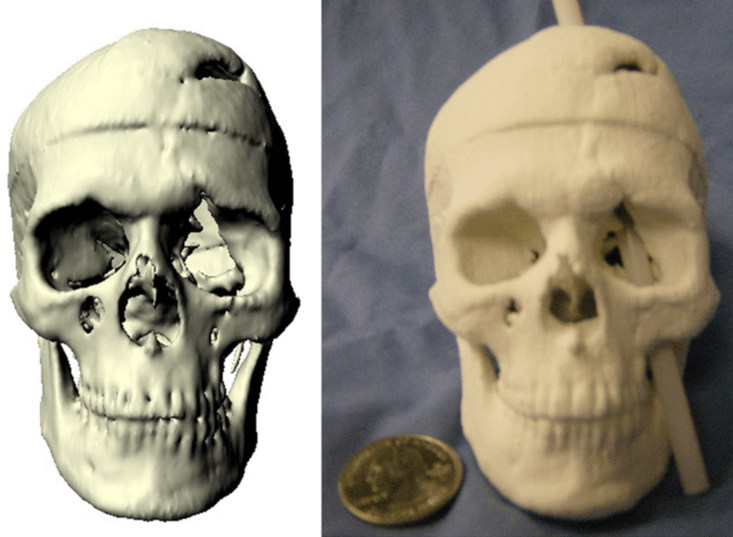
Animal model studies and clinical data both indicate that blood-brain barrier (BBB) breakdown frequently follows head trauma. Cell death within the first day following TBI promotes release of brain proteins and their breakdown products (biomarkers) from injured cells into biofluids such as cerebrospinal fluid (CSF) and blood.
If you’ve studied LEAKY GUT SYNDROME, you understand how the intestinal barrier becomes hyper-permeable (again, Inflammation), allowing an array of substances into the bloodstream that would ordinarily be kept out. The Blood-Brain Barrier acts in a similar capacity, and is made up of cells called Astrocytes, which are a type of GLIAL CELL. An increase in the permeability of the BBB, coupled with certain kinds of proteins, tissues, and fluids floating around in the blood after a head injury is a bad combination. It’s not difficult to understand why.
After TBI and rupture of the BBB, brain proteins released from damaged brain cells enter the bloodstream where they may trigger an immune response. Autoimmunity involves the development of antibodies against self-antigens, or autoantibodies. Depending on subtype, antibodies can be maintained within the bloodstream for years. The role of systemic autoimmunity in human traumatic brain injury (TBI) and other forms of brain injuries is recognized but not well understood. In this study, a systematic investigation was performed to identify serum autoantibody responses to brain-specific proteins after TBI in humans.
This paragraph is fairly self explanatory. The proteins, fluids, and tissues that are released post-TBI trigger an Autoimmune Response. In other words, even though the tissue is your own, because it’s not where is should be, the body may view it as a foreign invader (“antigen“) and create Inflammation and Immune System responses against it / them in the form of antibodies. In other words, your body is now making antibodies against itself. And in similar fashion to the the way most people only get Chicken Pox one time in their life (they maintain antibodies to fight it off), so you tend to “maintain” antibodies against these faux foes made up of your own tissues — probably for the rest of your life. In case you don’t realize the implications of having a war raging in your body at all times………
Multiple sclerosis (MS) is an example of an autoimmune disease that involves a central nervous system (CNS) antigen. Reports have documented brain-directed autoimmunity in neurological and neurodegenerative diseases such as Alzheimer’s disease, stroke, epilepsy, and paraneoplastic syndromes [crazy Immune System responses triggered by Cancer]. Additional studies have reported autoimmune responses in spinal cord injury.
Ask anyone who deals with them (or the people who take care of the people with them); MS, EPILEPSY, and ALZHEIMER’S can be a nightmare. This is a great spot to throw my two cents in about the relationship of Autoimmunity to GLUTEN. For reasons we are just beginning to understand (HERE and HERE), lots of people are having Immune System reactions (making antibodies) against Gluten. Unfortunately, most of these Immune System responses to Gluten are neurological (HERE) —- even in the absence of full-blown Celiac Disease (HERE). This intimate relationship between Gluten and Autoimmunity is not something brand new, and has been discussed for decades (HERE). In a nutshell, Gluten can act synergistically with various sorts Autoimmune Responses to crush people’s health.
The important implication for TBI patients is that GFAP-BDPs [the byproducts of the break down of the Glial Cells that make up the BBB] may persist within degenerating astrocytes in the brain, thus facilitating it becoming a predominant immune target. In addition, we found that anti-GFAP autoantibody can gain entry to live glia cells in culture. This is consistent with previous work showing that anti-nuclear autoantibodies can also enter cells. We further found that incubation with anti-GFAP autoserum causes cytotoxicity [cellular toxicity] in glial cells. Taken together, these data suggest that the presence of autoantibody to GFAP can be potentially pathogenic [potentially causing a wide array of “pathologies”] during the recovery phase of TBI.
Although this sounds really technical, it’s easy to follow. GLIAL CELLS break down following a TBI, allowing “stuff” to get into the blood that should not be there (according to Snell’s Clinical Neuro-Anatomy, the Glial Cells outnumber neurons by as much as 10 times, comprising half the total volume of both the brain and spinal cord). Unfortunately, the subsequent antibody response is not contained to the blood, but can actually gain entrance into the cells themselves. This is why the ER sending people home after a head injury and telling them they’ll be fine in a couple of days, is so misleading. Fortunately……..
TBI patients showed an average 3.77 fold increase in anti-GFAP autoantibody levels from early (0–1 days) to late (7–10 days) times post injury. Changes in autoantibody levels were negatively correlated with outcomes measured at 6 months, suggesting that TBI patients with greater anti-GFAP immune-responses had worse outcomes. Due to the long lasting nature of IgG, a test to detect anti-GFAP autoantibodies is likely to prolong the temporal window for assessment of brain damage in human patients. Quantitative detection of these biomarkers in biofluids would support a relatively simple and straightforward means of detecting brain injury. Because TBI diagnosis currently relies primarily on MRI and/or CT scans and neurological assessments, blood-based biomarker tests would represent a valuable new clinical tool.
In other words, there is now a blood test that allows us to see not only if there is cellular damage that has taken place in people with TBI’s, but how much damage. But this itself presents a rather significant problem. What to do next?
GREAT; I KNOW WHAT’S WRONG WITH ME
BUT WHAT DO I DO NEXT?
If you look at the governmental guidelines for TBI or MTBI as it is sometimes referred to (
Care of the Patient with Mild Traumatic Brain Injury), you’ll see that they talk about MRI’s, CT’s, other Brain Scans, sleep disturbances, HEADACHES, VERTIGO, and any number of other neurological issues and standardized tests. Despite the PLoS study we just discussed, our governmental guidelines currently state that, “Biomarkers are not routinely recommended“.Like me, you are probably not so interested in someone looking at you and telling you what you already know (you are a dizzy INSOMNIAC with MIGRAINE HEADACHES, whose eyes are bouncing back and forth with a nystagmus). Only they say it in big words you can’t understand, enabling them to charge obscene amounts of money. I understand that neurological symptoms cannot be ignored, but I’m mostly interested in what can be done to engage and speed up the healing process. The problem is, when you go to the doctor for TBI, you can’t count on anything that will aid the later.
Case in point, a five year old study found in the British Columbia Medical Journal (
Pharmacological Interventions for Traumatic Brain Injury). Their recommendations for those with TBI involve “fun” drugs like ANTIDEPRESSANTS, various forms of METHAMPHETAMINE which they categorize as “psychostimulants”, Anti-PARKINSON’S drugs, ANTI-CONVULSANTS, SLEEP MODULATORS, BETA-BLOCKERS, and an array of others.Is it just me, or does covering the symptoms of a TBI without doing anything meaningful to solve the underlying cause of those symptoms and their subsequent metabolic consequences, seem absurdly unscientific and counter-productive in this day and age of EVIDENCE-BASED MEDICINE? Although drugs are exactly what the authors recommend, on at least some level they agree they are double-minded in this area by concluding that, “
The nature of TBI sequelae, whether psychiatric, cognitive, or behavioral, is poorly understood. Likewise, the use of pharmacological interventions to improve symptoms, function, and outcome is still under development.” Fortunately, there is another way — a better way.What do I recommend to people dealing with unresolved residual symptoms of a TBI? As you might imagine, I would first recommend you start clicking links on this page. Knowledge is power, and it is critical for you to learn how to control the amount of Inflammation you are living with, so that you can get your “barriers” (gut, brain, lungs, etc) healed and intact. I’ve only written about a hundred posts on this particular topic, but HERE is a generic entry that has something for everyone.
However, for those of you who are truly struggling neurologically, I would seriously contemplate finding a Chiropractor trained by Dr. Carrick’s Institute. I have spent some time around a number of Functional Neurologists, and they are collectively some of the most brilliant people I have ever met — particularly when it comes to UNDERSTANDING THE BRAIN.