CHRONIC LOW BACK PAIN, STRETCHING, AND THE THORACOLUMBAR FASCIA
I’ve written several very cool posts concerning the Thoracolumbar Fascia (HERE, HERE, and probably the best one — HERE), but this one is different yet. Co-authored by endocrinologist / neurologist / fascia researcher, DR. HELENE LANGEVIN, the January 2016 edition of PLoS One carried a study called Ultrasound Evaluation of the Combined Effects of Thoracolumbar Fascia Injury and Movement Restriction in a Porcine Model. In this study, the authors started out by saying…
“The persistence of back pain following acute back ‘sprains’ is a serious public health problem with poorly understood pathophysiology. The recent finding that human subjects with chronic low back pain (LBP) have increased thickness and decreased mobility of the thoracolumbar fascia measured with ultrasound suggest that the fasciae of the back may be involved in LBP pathophysiology.”
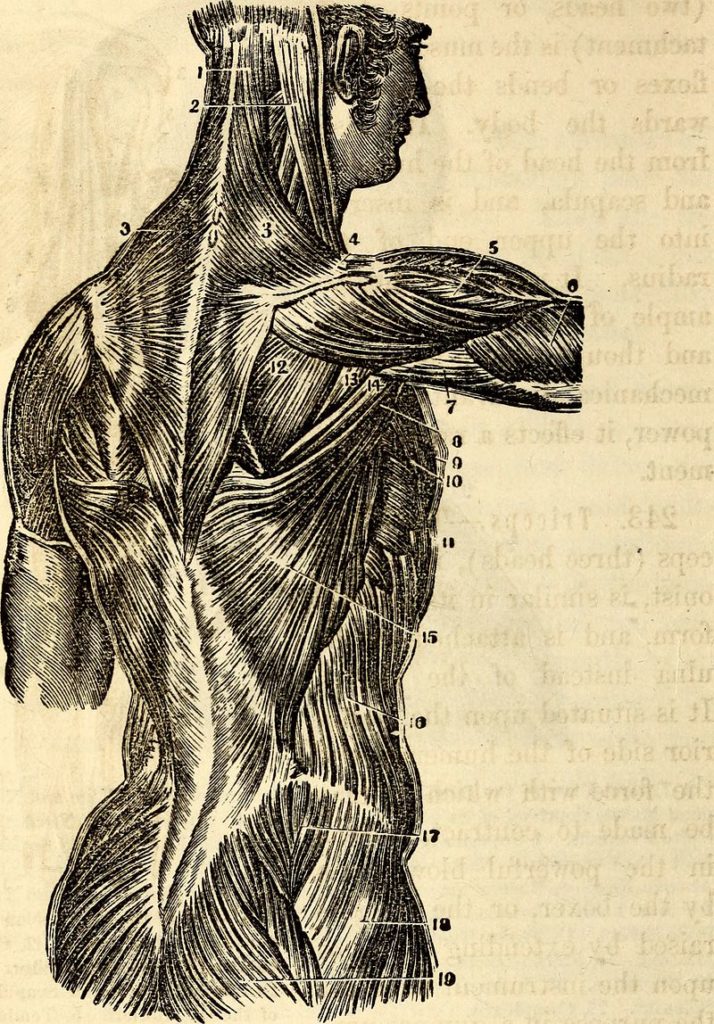
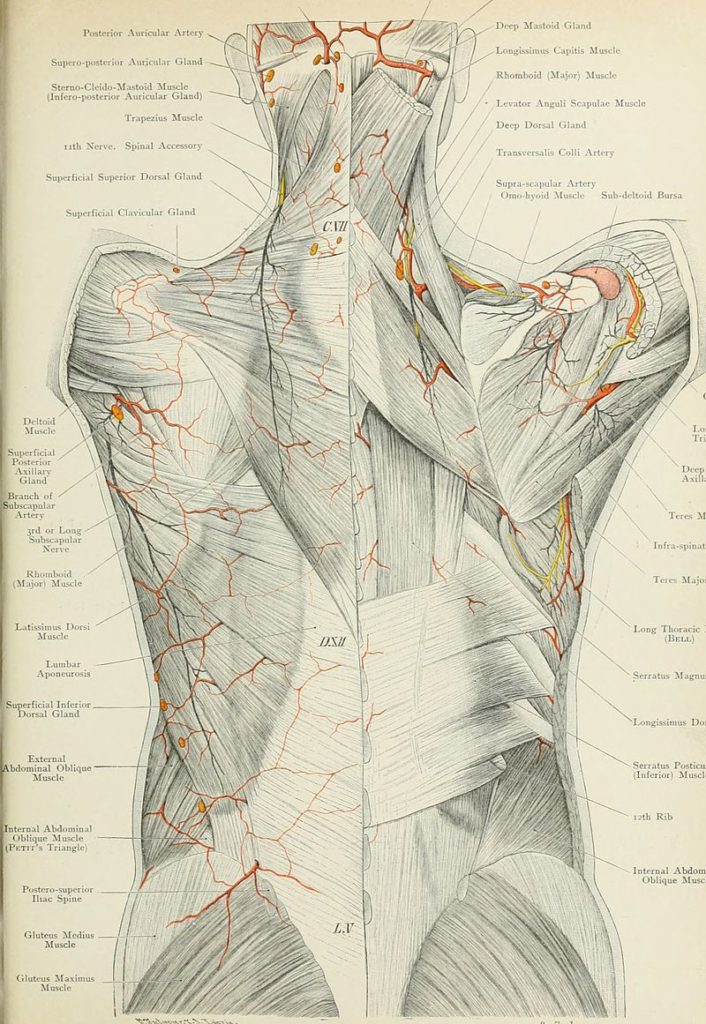
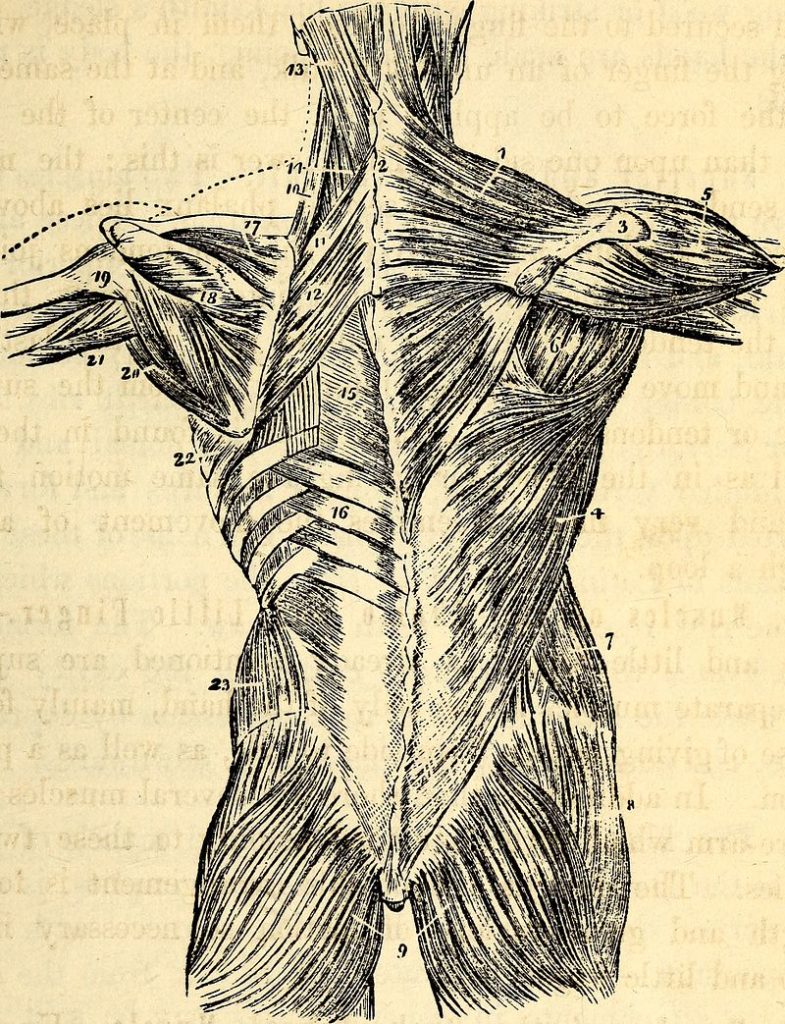
What is a sprain? A sprain is essentially an injury (usually a microscopic tearing) of soft tissues (usually LIGAMENTS) whereby the result is varying degrees of tissue damage (the Thoracolumbar Fascia is very much like a group of ligaments or even TENDONS or RETINACULUM, and is the diamond-shaped area of white tissue seen at the very lowest part of the back). In this study, the authors took anesthetized pigs, and using blunted surgical instruments, created a “fascia injury” about two inches square by detaching layers of fascia from each other.
The study looked at these “injured” pigs in relationship to whether they were hobbled (hobbles are devices used to prevent animals from kicking or walking normally) -vs- injured pigs that were not hobbled. The authors used gait analysis as well as DIAGNOSTIC ULTRASOUND — the standard for imaging fascia — for their determinations. What sorts of differences were noted in the two groups after the hobbles were removed? (conclusions are cherry-picked due to restraints on time and space.)
“There was a significant main effect of movement restriction on gait speed with hobbling. The thickness of deep subcutaneous tissue and perimuscular fascia was significantly greater in the injured pigs compared with the non-injured groups…. similar to those observed in a study of humans with chronic LBP. Restricted fascia mobility may cause altered proprioception and movement patterns, and thus could be involved in low back pain pathophysiology without being the direct source of nociceptive input.
Injury alone caused both a significant increase in fascia thickness and decrease in fascia mobility on the non-injured side, demonstrating the presence of a pathological process involving the thoracolumbar fascia extending beyond the injured area. Adding movement restriction to a soft tissue injury can worsen an already increased tendency of fasciae to adhere together and lose shear plane mobility.
It is well known clinically that restricting movement of joints causes adhesions in periarticular connective tissue, especially after an injury or surgery. Our previous studies in humans, and the results of our porcine model, indicate that a similar pathology can occur in the fasciae of the dorsal trunk in response to a mild fascia injury, especially in the presence of movement restriction.”
- INJURED TISSUES SHOW RESTRICTED MOTION: When it comes to chronic musculoskeletal pain that is the result of some sort of injury as opposed to SYSTEMIC INFLAMMATION, we must look for aberrant biomechanics. Joint restriction (HERE for example) is usually (but NOT ALWAYS) easy to see, and is the starting point for numerous CHRONIC PAIN CONDITIONS. It is important to understand that this restriction comes in two distinct flavors (HERE) — flavors that cannot effectively be addressed in identical fashion.
- INJURED FASCIA THICKENS: This is the phenomenon that many in the profession have referred to as DENSIFICATION.
- THE THORACOLUMBAR MODEL OF LOW BACK PAIN IN HUMANS LOOKS SIMILAR TO THIS MODEL: Sure, these authors used pigs in this study, but we see the same thing in humans (HERE).
- FASCIAL INJURIES ARE LIKELY ASSOCIATED W/ ABNORMAL BIOMECHANICS AND PROPRIOCEPTIVE LOSS: We already talked about the former in the first bullet (by the way, the end-product of abnormal biomechanics is always degeneration). Much of this degeneration is simply due to loss of proprioception (HERE). If you want to see what this process looks like on a metabolic level, take a look at my COLLAGEN SUPER PAGE. I would also challenge you to read a short post concerning the fact that at least one of the authors of the two papers being discussed today believes that ADHESED FASCIA COULD BE THE UNIVERSAL CAUSE OF DISEASE, simply due to loss of proprioception. Yes; this bullet is a bigger deal than you ever could have imagined (HERE). And the kicker is that this is all happening without ever directly stimulating pain receptors (nociception).
- IMMOBILIZING INJURIES MAKES THEM WORSE: Yes, I am still an old-school fan of using ice on injured tissues (HERE). And sometimes you will be forced to get off it or immobilize it for a brief period of time. However, I firmly believe that early restoration of motion is critical, and that this motion must be both segmental as well as sectional (HERE). As I showed earlier, the end-product of abnormal motion over time is always degeneration. Unfortunately, degeneration always leads to loss of abnormal motion. Can anyone see a vicious cycle starting to form? FYI; when researchers want to create degenerative arthritis to study in the lab, they immobilize whatever body part of whatever animals they are studying, and presto — kind of like the hobbling thing
Just days ago, the current issue of the journal Physical Medicine & Rehabilitation published a similar study by the same authors called Effect of Stretching on Thoracolumbar Fascia Injury and Movement Restriction in a Porcine Model. After going through much of what they did in the first study, they took the “injured & hobbled” pigs and tried adding 10 minutes of stretching a day for a month. It didn’t matter. Note that while the injury appeared to improve on the surface, deeper analysis showed this was not the case.
“Removing hobbles restored normal gait speed but did not restore fascia mobility. Daily passive stretching was not superior to removing hobbles, as there was no significant improvement in fascia mobility with either treatment group (removed hobble or stretching). Reduced fascia mobility in response to injury and movement restriction worsens over time and persists even when movement is restored. Reversing fascia abnormalities may require either longer than 1 mo or a different treatment “dose” or modality.”
What’s my opinion? Of their three potential conclusions, I feel that the middle one is most correct — a “different treatment” is needed. While I am a fan of certain modalities (LLLT for instance), my opinion is that most are a waste of time, energy, and money. And in our modern era, if people think they are helpful, it would probably be cheaper to just buy an electrical stim machine or ultrasound device on E-bay.
In more severe cases, someone is going to have to manually “break” these adhesions. Just remember that the worse the FASCIAL ADHESION, the less the chance that standard fare such as THERAPY or CHIROPRACTIC ADJUSTMENTS will accomplish this.
Also, the greater the adhesion, the greater the force needed to break said adhesions. This is why I have repeatedly said that breaking severely adhesed fascia is kind of like PLAYING A CARNIVAL GAME. The idea that a whole lot of small (sub-threshold) treatment can somehow add up to big results is, in most cases, erroneous. Once the tissue is broken, it is much easier (in many cases it’s finally possible) to reduce CHRONIC SUBLUXATIONS and deal with underlying mechanical issues such as LOWER CROSSED SYNDROME or UPPER CROSSED SYNDROME.
For the record, if you really want to keep this junk from coming back / returning, continuing to build FIBROSIS, DEGENERATING, and along the way CAUSING CHRONIC PAIN, many of you will have to adjust your lifestyles. All this means is that you’ll need to figure out the sources (especially the hidden or occult sources) of inflammation in your life. Diet is, of course, the low-hanging fruit — the easiest thing to change and the quickest thing to see results from. But there are potentially many others.
To get a glimpse of what this might look like, just take a look at THIS POST. And if you want to see an ordered list of the nearly 150 posts I’ve authored on fascia, simply click THIS LINK. And be sure to like, share or follow on FACEBOOK while you are at it.
