NON-CARDIAC CHEST PAIN
NO, YOU’RE NOT CRAZY!

“Chest pain presents a diagnostic challenge in outpatient family medicine. Non-cardiac causes are common.”From the November 2005 issue of the American Family Physician (Diagnosing the Cause of Chest Pain) In my clinic I treat lots and lots of people who suffer from various sorts of non-cardiac, musculoskeletal chest pain and rib tissue pain.
How common is the phenomenon of rib or chest pain not related to heart or cardiovascular issues? Here is what several physicians from California’s Mount Sinai Hospital, writing in a 2013 issue of Primary Care: Clinics in Office Practice (Evaluation and Treatment of Musculoskeletal Chest Pain), had to say.
“Chest pain is one of the most common reasons for seeking medical attention world-wide. In the United States alone, there are about 7.16 million visits annually to the emergency room with chest pain. Most of these patients have non-cardiac causes of chest pain.”
Did you catch that? “Most” (the majority — over 50%) of chest pain patients do not have pain coming from their heart. According to these authors, the number one reason for chest pain is (drum roll please)….. “Musculoskeletal chest pain, making it the most common cause of chest pain.“
Thirty years ago, a 1988 issue of the journal, Primary Care (Approach to Musculoskeletal Chest Wall Pain) made some very important points in regards to this topic. Firstly, they said that “Pain in the chest may be the presenting feature of a diverse number of musculoskeletal chest wall conditions.”
What were the most common of these “conditions“? “Trauma to the chest wall, benign overuse myalgia [muscle pain], fibrositis, referred pain.” By the way, although fibrositis and myalgia would today be referencing TRIGGER POINTS, back then it’s likely they were discussing what we today call FIBROMYALGIA, both of which are known to cause referred pain.
Furthermore, “these disorders are often mistaken for angina pectoris and other serious disorders.” In other words, they are frequently mistaken for heart or cardio related pain.
Why do you think that people — especially people whose mechanism of onset points away from cardiac problems (i.e. they were injured, they frequently overwork, or they don’t really fit a cardiac profile) — end up being repeatedly run through every heart test imaginable (HERE and HERE are examples) only to be told there is nothing wrong with them?
It’s why these authors went on to state that, “Knowledge and understanding of the underlying pathogenic mechanisms of these musculoskeletal disorders is important for optimal management.” Today I am going to hit you with quotes from numerous studies over the past half century (as always, many are CHERRY-PICKED) showing just how common this phenomenon of non-cardiac chest / rib pain really is. Pay attention because if you are reading this post because a Google search brought you here, you’ll likely see yourself in many of them.
“Chest pain in ambulatory setting is predominantly not heart-associated. Most patients suffer from musculoskeletal…. chest pain.” From the January 2015 issue of the German journal, Therapeutiche Umschau (Chest Pain)
“The musculoskeletal system is a recognized source of chest pain. However, despite the apparently benign origin, patients with musculoskeletal chest pain remain under-diagnosed, untreated, and potentially continuously disabled in terms of anxiety, depression, and activities of daily living.” From a 2010 issue of Medical Clinics of North America (Chest Pain in Focal Musculoskeletal Disorders)
“Chest pain is a common presenting problem to general practitioners and accident and emergency departments. Such a symptom generates anxiety in both patients and their medical attendants, for fear that this symptom represents a life threatening event. Numerous investigations often ensue, adding to the physical and financial burden on an already stressed health system. Musculoskeletal causes of chest pain are common but frequently overlooked. Careful history taking to identify red flag conditions differentiates those who require further investigation.
Historical features suggesting a musculoskeletal cause include pain on specific postures or physical activities. A musculoskeletal diagnosis can usually be confirmed by clinical examination alone, the key to which is reproducing the patient’s pain by either a movement or more specifically palpation over the structure that is the source of the pain.” From a 2001 issue of the Australian Family Physician (Musculoskeletal Causes of Chest Pain)
“Mechanical chest wall pain is a common presenting complaint in the primary care office, emergency room, and specialty clinic. Diagnostic testing is often expensive due to similar presenting symptoms that may involve the heart or lungs. Since the chest wall biomechanics are poorly understood by many clinicians, few effective treatments are offered to patients with rib-related acute pain, which may lead to chronic pain.
Manual diagnostic and therapeutic skills can be learned by physicians to treat biomechanically complex rib-related chest wall pain in combination with interventional image-guided techniques. Pain physicians should learn certain basic manual manipulation skills both for diagnostic and therapeutic purposes.” From the March 2016 issue of Pain Physician (Multi-Modal Treatment Approach to Painful Rib Syndrome: Case Series and Review of the Literature)
These quotes mention examinations several times. The problems is, competent examinations are rapidly becoming a thing of the past. Just yesterday I asked a patient who is a truck driver — he’s an old timer who’s been driving for the better part of sixty years — how much work he could do on his own trucks these days.
Specifically, I asked him whether there was anything he couldn’t do on a truck (I am loosely quoting him here). “I can’t do everything anymore, but I used to be able to. But I hate taking my trucks to the shop. The people there rely almost totally on technology to diagnose your problem and can no longer think for themselves.”
I’ve heard essentially this same thing said of the medical community from physicians who have been in the field a long time (LIKE THIS ONE) — take away their technology and they can’t function or make an accurate diagnosis. Why not?
The massive replacement of competent examinations with technology (cardiac testing and x-rays or advanced imaging techniques that rarely provide an ah ha moment — HERE and HERE) has in many ways been a disservice to suffering patients.
The result is that people are written off, often times as having some sort of psychogenic pain that can be cured by things like (ahem) “MINDFULNESS“. This sort of scenario is especially common with CHRONIC RIB TISSUE PAIN as you will see if you click the link. Follow along as I show you not only what the current research says (not to mention some older research), but why your problem might not be as hopeless as you have been led to believe.
MUSCULOSKELETAL CHEST PAIN
“Chest pain is a common symptom associated with a variety of underlying causes. It is estimated that more than six million people visit hospital energy departments in the United States annually because of chest pain. It is the second most frequently reported principal reason for visiting the emergency unit. The most common causes of chest pain are musculoskeletal (30-50%).”From 19 Important Causes of Chest Pain by Dr. Axel Sigurdsson MD
“Pain in the chest is a source of anxiety to both patient and doctor so long as its cause remains uncertain. Probably the most common cause is trauma to the rib cage from sporting activities, accidents, falls, or assault. X-ray films often show only about half the rib fractures that actually exist, given what is found at necropsy.” From the Valentine’s Day issue of the British Medical Journal (Rib Pain) 1976
“Chest pain in children is relatively common…..” From a 1984 issue of Pediatric Clinics of North America (Recurrent Chest Pain in Children)
“Chest wall tenderness is common but does not always reproduce the presenting symptoms.” Dr. Christopher Wise MD from his article Major Causes of Musculoskeletal Chest Pain in Adults
“Musculoskeletal chest pain or chest wall pain is the most common type of chest pain presenting to the primary care office.” From the February 2018 issue of Musculoskeletal Sports and Spine Disorders (Muscluloskeletal Chest Pain)
“Chest pain is a common general practice presentation, which, because of its diverse and potentially serious causes, requires careful and often urgent assessment. Although it is critical to rule out potentially life-threatening conditions, in the general practice/primary care setting, musculoskeletal conditions are the most common causes of chest pain.” From the August 2015 issue of the Australian Family Physician / Thorax (Musculoskeletal Chest Wall Pain)
Think about the quote directly above. We know that chest pain can be potentially serious, but we’ve also learned that it’s not only dog common, but that much of it — arguably most of it — is musculoskeletal in nature. What does this mean to the average ‘chest pain’ patient? Exactly what I explained earlier — spending time on the MEDICAL MERRY-GO-ROUND. A 2005 study from the European Journal of Internal Medicine (The Causes of Musculoskeletal Chest Pain in Patients Admitted to Hospital with Suspected Myocardial Infarction) reveals why.
After looking at fifty people who had been hospitalized for chest pain and then run through the gamut of cardiovascular tests, the authors revealed that, “Musculoskeletal causes for acute chest pain are common and varied. Most patients have an identifiable cause of pain, but accurate diagnosis is needed to select the most appropriate intervention. Anxiety and depression are frequent, with much self-reported pain and dysfunction.”
Once again, when all else fails blame it on ANXIETY & DEPRESSION. The harsh reality is that more often than not, pain and dysfunction are causing A&D, not the other way around as is usually touted by the medical community (it’s why anti-depressants are commonly prescribed to those with chronic pain and part of what I refer to as chronic pain’s ‘BIG FIVE’).
Two medical doctors, Jeffrey Oken and Aaron Hanyu-Deutmeyer, writing for PM&R Knowledge said this of something known as Chest Wall Pain Syndrome (CWPS).
“Chest wall pain syndrome is a painful condition that manifests as direct or referred pain to the chest wall as a result of stress/injury to the body. CWPS is used to describe a multitude of pathologies that may result in pain that can be self-limiting or chronic. CWPS is readily mistaken for more serious conditions, such as acute coronary syndrome and pulmonary embolism…. The most common cause of CWPS is musculoskeletal.”
Are you seeing a trend?
What about the neck’s relationship to chronic musculoskeletal chest pain? Clear back in 1985, the Canadian Medical Association Journal (Musculoskeletal Chest Wall Pain) said this of the affiliation. “The musculoskeletal structures of the thoracic wall and the neck are a relatively common source of chest pain.”
An excellent 2013 article by three physicians in Primary Care Clinics (Evaluation and Treatment of Musculoskeletal Chest Pain) agreed, taking this concept a step further by saying, “Pain can also radiate to the chest from the shoulders, cervical and thoracic spine, lower neck…..” What would make the neck a trigger for chronic chest or rib pain? All you really have to do is look at the anatomy.
For instance, the SCM, CERVICAL FASCIA, and PLATYSMA — three of the more commonly injured tissues of the cervical spine — attach to the clavicle (collar bone) which makes up the top margin of the chest. This means that they can be involved in much more than CHRONIC NECK PAIN (as we just saw, all of these, along with the THORACOLUMBAR FASCIA, refer pain to the tissues of the thoracic wall. But the pain can be referred from below as well.
For instance, ABDOMINAL MUSCLES (or HERE) and HIP FLEXOR ADHESIONS have the potential to pull at the tissues that attach to the thoracic cage / rib cage, potentially causing pain as well. The same thing can be said of the muscles that actually make up the thoracic cage (I commonly see SCAR TISSUE built up in the area where the chest muscles, shoulder muscles and biceps muscle come together).
What is the medical community doing to help people with chronic musculoskeletal chest or rib pain? You can take a guess, but the last study mentioned said it all. Despite the article providing a number of useful flow-charts for helping make an accurate diagnosis, their solution is about the same as it is for any number of pain-related issues. Their top-recommended ways to treat these problems?
After looking at 25 pages of different causes of chest and rib pain, as well as the treatments endorsed for each; over and over again we see that the most common treatment is PAIN MEDS and NSAIDS. Think about it this way; if this approach was really so wonderful, you likely wouldn’t be reading this with tears in your eyes at three AM. Things, however, may be starting to change.
Just last year, an MD — a retired cardiologist by the name of Daniel Gelfman (he is now working as a professor at an osteopathic college) — wrote an editorial for the American Journal of Medicine (Osteopathic Manipulation in Treatment of Musculoskeletal Chest Pain) in which he stated…
“Throughout most of my 29 years of practicing clinical cardiology, I was never really satisfied with treatments I employed in the treatment of musculoskeletal chest pain. This was especially true with the recognition of nonsteroidalanti-inflammatory drug (NSAID) complications. Now, at the end of primary clinical practice, I believe I have found a satisfactory treatment.
The technique I employed for this specific chest discomfort is called myofascial release. I suspect many physicians are, as I previously was, unaware how effectively somatic dysfunction such as musculoskeletal chest pain can be treated with…. a multitude of gentle, non high-velocity low-amplitude techniques [adjustments]. This includes techniques such as muscle energy, strain counterstrain, myofascial release, soft tissue,and balanced ligamentous tension.”
While this is super cool, it’s nothing new outside of the mainstream medical arena — sort of like trying to convince an Egyptian that you discovered the pyramids.
RIB TISSUE & THORACIC WALL PAIN FROM OLD RIB FRACTURES
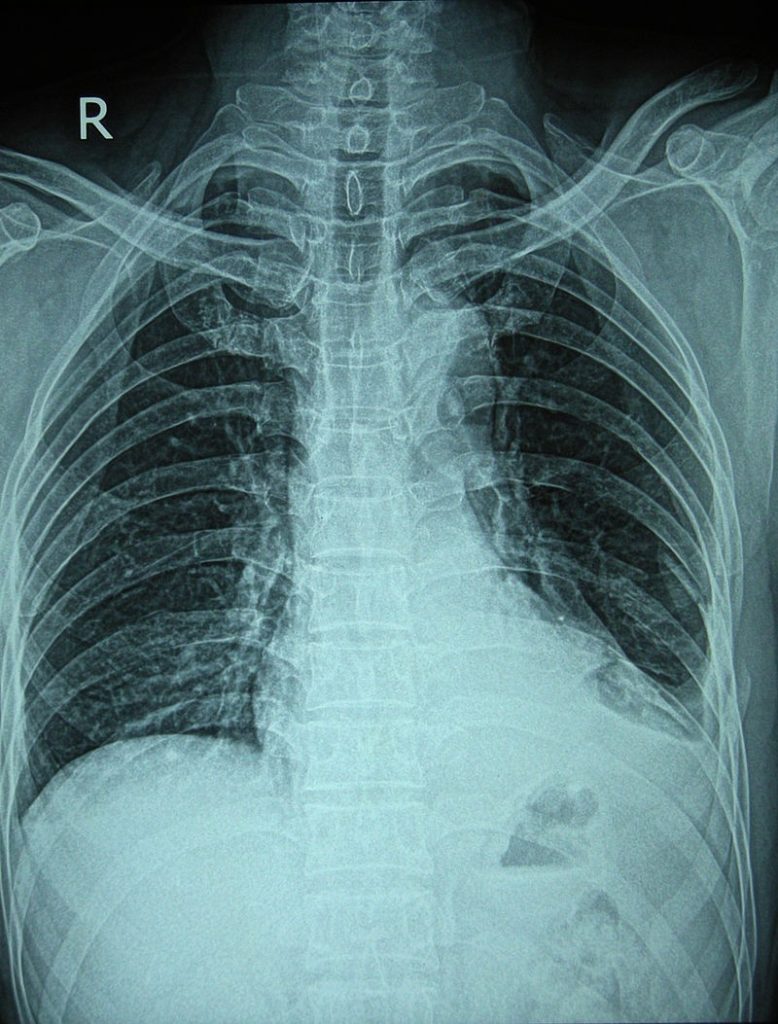
“Rib fractures are among the most common traumatic injury found in 20% of all patients who suffer thoracic trauma. The majority of these are a result of a blunt mechanism and are often associated with other traumatic injuries…. Rib fractures are the most common blunt thoracic traumatic injury.” From last April’s issue of the BMJ journal, Trauma Surgery and Acute Care Open
The thing that makes almost any sort of rib problem unique is how bad they can hurt. Unless you shatter ribs — the sort of injury that lands you in the ER — rib fractures are not generally dangerous like say a HERNIATED DISC can be; something with a significant chance of requiring surgery to repair.
But ribs have the potential to cause pain like almost no other body part. And if you’ve had rib fractures (or even hard blows to the thoracic cage area that cause bruised ribs) it’s often times enough to cause massive amounts of pain. How much pain are we talking about, and maybe even more importantly, how long does the pain from old rib fractures last? Let’s look at some studies.
Fifteen years ago, the Journal of Trauma asked a question via a study title; Rib Fracture Pain and Disability: Can We Do Better? Their conclusions? Rib fractures, especially multiple rib fractures, have a shockingly high probability of causing long-term pain and dysfunction (disability).
“Rib fractures are a significant cause of pain and disability in patients with isolated thoracic injury and in patients with associated extrathoracic injuries. When compared with the chronically ill reference population of the RAND Medical Outcomes Study, our patients as a group were more disabled at 30 days in all categories except emotional stability, where they showed equivalent disability.”
As far as issues with emotional stability go, they usually tend to show up after a longer time of struggling with CHRONIC PAIN. A decade after this study, things had not changed much.
The May 2013 issue of the American Journal of Surgery (Prolonged Pain and Disability are Common After Rib Fractures) tells you most of what you need to know via its title. The authors — a group of acute care trauma surgeons from Oregon — went on to say, “The presence of significant associated injuries was predictive of prolonged disability. Prolonged chest wall pain is common, and the contribution of rib fractures to disability is greater than traditionally expected.”
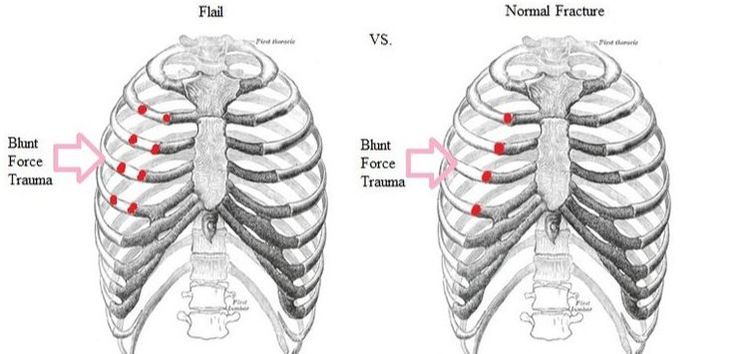
For the record, when you see the term “flail chest” used (see middle pic above), it indicates three or more broken ribs together, all fractured in two or more places. But what about thoracic cage injuries that are not considered “serious”? What about people who get a rib fracture or two, go to the ER and are subsequently released because there is little that doctors can do for MTI (Minor Thoracic Injury)?
The Academy of Emergency Medicine published a study a few months after the one above called Risk Factors of Significant Pain Syndrome 90 Days after Minor Thoracic Injury…. Almost 1 in 5 of the 735 individuals in the study “was experiencing clinically significant pain at 90 days after a MTI.” Unfortunately, 90 days is a threshold most often used to asses potential permanency of these sorts of problems.
For example, research shows that if you are still struggling 90 days out from a WHIPLASH INJURY due to a MOTOR VEHICLE ACCIDENT (or for that matter, other similar injuries from any number of sources) your odds of having that problem become, at least on some level, permanent, skyrockets. In the past few years, several studies have shown similar.
For instance, the May 2014 issue of the American Journal of Surgery (The Contribution of Rib Fractures to Chronic Pain and Disability). After following almost 100 rib injury (rib fracture) patients for six months, the authors (the same group of surgeons from Portland’s Health & Science University) said this…
“The prevalence of chronic pain was 22% and disability [dysfunction — these people were not necessarily “disabled”] was 53%. Associated injuries, bilateral rib fractures, injury severity score, and number of rib fractures were not predictive of chronic pain. No acute injury characteristics were predictive of disability. The prevalence of chronic pain was 28% and of disability was 40%. No injury characteristics predicted chronic pain. The contribution of rib fractures to chronic pain and disability is significant but unpredictable with conventional injury descriptors.”
One other tidbit in this study was that initially having worse pain was predictive of long-term problems.
in January of 2015, a group of Australian physicians and researchers published a study (Quality of Life After Major Trauma with Multiple Rib Fractures) in the journal Injury. Conclusions were that, “Rib fractures are a common injury presenting to major trauma centres and community hospitals. Aside from the acute impact of rib fracture injury, longer-term morbidity of pain, disability and deformity have been described. Despite this, the mainstay of management for the vast majority of rib fracture injuries remains supportive only with analgesia.”
In essence, there is little to do other than make sure people are comfortable. After following 400 multiple rib trauma patients for two years, the authors determined that, “Patients with multiple rib fractures demonstrated significantly lower quality of life at all time points measured. Return to work rates were poor with only 71% of those who were working prior to their accident, returning to any work. This study demonstrates a significant reduction in quality of life for rib fracture patients requiring admission to hospital…” Think about that — almost 1 in 3 was severe enough that after two years they were still not working.
A 2016 study from the Scandinavian Journal of Trauma, Resuscitation, and Emergency Medicine (Physical Function and Pain after Surgical or Conservative Management of Multiple Rib Fractures – A Follow-Up Study) looked at two groups of thirty subjects each — one group having surgeries for their multiple rib fractures and the other not, determining that…
“…concerning respiratory and physical function, pain, range of movement in the shoulders and thorax, shoulder function and kinesiophobia [fear of movement]… The results concerning pain, lung function, shoulder function and level of physical activity were similar in the two groups. Patients undergoing surgery have a similar long-term recovery to those who are treated conservatively except for a better range of motion in the thorax and fewer limitations in physical function. Surgery seems to be beneficial for some patients, the question remains which patients.“
In April of this year, a study by the French military (Chronic Chest Pain after Rib Fracture: Can it Cause a Disability?) was published in Revue de Pneumologie Clinique. The authors, six trauma physicians, concluded after following 40 patients for almost six years (most of them young males who had been in motor vehicle accidents)…
“The initial management consisted in the use of analgesics systemically in all patients. Persistent pain was noted in 60% of cases. This pain was triggered by simple to moderate effort to moderate in 55% of cases, and hard effort in 28% of cases. In 17% of patients, even at rest, the pain occurred intermittently. Impact in terms of disability was mild to moderate in 28% of cases and important in 17%.
Neuropathic pain was found in 3 patients. Our study confirms the persistence of chronic painful, sometimes lasting several years after the initial chest trauma. This pain is responsible of disability triggered most often after exercise.“
I could have kept going but you get the point. Firstly, lots (LOTS) of people break ribs for various reasons. And secondly, it’s exceedingly common for these fractures to lead to chronic pain. And if you think about what I’ve told you in the past (HOW DOES FASCIA TEAR), “impact injuries” are an ultra-common mode of soft-tissue and fascial injury (today’s articles spoke extensively of blunt force trauma).
To take this phenomenon to its logical conclusion, realize that it’s also common to see these same kinds of injuries over any fracture. For example, I have effectively treated numerous people (INCLUDING MY WIFE who broke her arm in a run-in with a drunk back in 2005) for pain at the site of old fracture(s).
OTHER CAUSES OF RIB OR MUSCULOSKELETAL CHEST PAIN
The first thing I want to talk about in this section (I mentioned in a study discussed earlier) is something known as “Painful Rib Syndrome” aka “Slipping Rib Syndrome. I reference this because I’ve seen a number of people who are diagnosed with it who don’t actually have it.
As you might imagine, with a name like Painful Rib Syndrome, it can easily become what I call a “bucket diagnosis”. Not sure what’s going on, throw it in a bucket labeled “arthritis,” “fibromyalgia,” or any number of others, including…. PRS. Here is what Healthline (Slipping Rib Syndrome) has to say about this phenomena.
“Slipping rib syndrome occurs when the cartilage on a person’s lower ribs slips and moves, leading to pain in their chest or upper abdomen. Slipping rib syndrome goes by many names, including clicking rib, displaced ribs, rib tip syndrome, nerve nipping, painful rib syndrome, and interchondral subluxation, among others. It mostly affects middle-aged people. Overall, the syndrome is considered rare.”
According to the Indian Journal of Anesthesia, however (The Painful Rib Syndrome), it’s not so rare. “Painful rib syndrome is a fairly common condition. The painful rib syndrome is thought to arise from the inadequacy or rupture of the interchondral fibrous attachments of the anterior ribs. This disruption allows for the subluxation of costal cartilage tips, impinging on the intercostal nerves. This may cause a variety of somatic and visceral complaints.”
In other words, the FASCIA covering the ribs, for whatever reason (there are many, and in many cases the reason is unknown) fails to hold the tips of the ribs in place, allowing them to move out of position and not only cause pain, but organ issues as well. How do you diagnose this problem?
In doing this research I found several sources (both articles and journals) saying that the “Hooking Maneuver” is really the only way to make a correct diagnosis. It’s not difficult. Simply reach under your bottom front ribs, hook your fingers and pull out and up. If it reproduces your pain, this is likely the cause. Confirmation comes from having a nerve block and seeing if it hides the pain caused by the Hooking Maneuver.
As far as treatment, the medical literature abounds with choices. First is usually, you guessed it, NSAIDS, followed by various sorts of INJECTIONS, and in some cases, actually removing the offending rib. A 1993 study from Gut (Painful Rib Syndrome–A Review of 76 Cases) said that of every one of the patients sent to pain management for this problem, all were “without relief of symptoms“.
There are other causes of non-cardiac rib or chest pain as well. Because you can easily look them up online, there is Tietze’s Syndrome -vs- Costochondritis. I found dozens of studies on rib pain and muscluloskeletal chest pain in competitive rowers. I also discovered studies on these sorts of pain issues related to surgical ports.
I even found two different studies on rib pain and mechanical chest pain caused by deficiency of Vitamin D (Vitamin D Deficiency: An Unrecognized Cause of Flank Pain in a 2017 issue of Bone and Mineral Metabolism as well as Association Between Nonspecific Skeletal Pain and Vitamin D Deficiency in a 2010 issue of the International Journal of Rheumatic Disease). It will be no shock to see that those struggling with COPD usually deal with this sort of pain. In other words, there are numerous potential causes of this kind of pain.
My rule of thumb is that if the pain can be reproduced either by a certain posture (for instance, sitting) or by certain movements (sometimes these movements must be forced with some intensity), it’s much more likely that the problem is something I can help. In other words, it’s more likely that it’s in the THORACIC WALL AND NOT THE THORACIC CAVITY.
WHAT CAUSES RIB TISSUE PAIN AND MUSCLULOSKELETAL CHEST PAIN?
WHY DOES IT HURT SO BAD BUT NO ONE SEE IT OR TELL ME WHY?

If you look at my previous work on RIB TISSUE AND MUSCULOSKELETAL CHEST PAIN, you quickly see from the pics that ribs are covered in tissue, including MUSCLES and FASCIA. A quick peek at the anatomy of both ribs and the rib cage shows just how much fascia there is in several different layers on the ribs and thoracic cage (HERE is a one minute video showing this fact).
While there is new technology that’s starting to be used to image fascia in certain places like the low back (THORACOLUMBAR FASCIA) there is no good imaging tests for the rest of the body — not a good thing for a tissue that’s not only the most common connective tissue in the body, but also happens to be the chief culprit in chronic pain’s “PERFECT STORM“.
So, beyond doing the things it takes to cut systemic inflammation from your life (HERE), a trip to see me might just be in order. After all, who else tells you that you will know from a single treatment whether or not my approach will help you (HERE). If you liked today’s post, be sure to like, share, or follow on FACEBOOK.
