DIAGNOSING AND TREATING PEOPLE WITH SLAP TEARS OF THE GLENOID LABRUM: AVOID SHOULDER SURGERY!
 |
 |
“Non-operative treatment may help a large percentage of patients with a superior labral tear.”The opening statement of the SLAP lesion web page for the massive East Coast physician’s group, Rothman Orthopedics (Non-operative Superior Labrum Anterior to Posterior (SLAP)
Before we get into the meat and potatoes of what tears of the shoulder’s glenoid labrum (the notorious SLAP tear) entail, let’s get something straight. Although these tears (often referred to as ‘lesions’) have historically been dealt with in a surgical manner, there is a significant movement afoot — much of it by elite-level orthopedists and therapists — that in many cases; arguably most cases, surgery is not required. If you are willing to do what it takes to help heal your shoulder, you could potentially avoid the lengthy, brutal and expensive rehab associated with a SLAP.
This means that if you are diagnosed with a SLAP lesion, it may behoove you to get multiple opinions (including your own) because facts like this, even though supported by the preponderance of peer review, are often ignored by work-a-day ‘Joe Physician’. To put it another way, far too many people are being told that surgery is their only option.
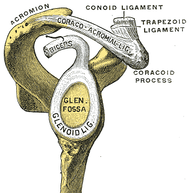
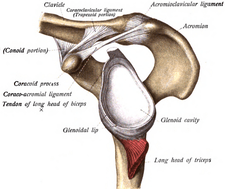
What is the glenoid (shoulder) labrum? The Latin word “lab” such as seen in words like labia, labrum, labrus, labium, labella, etc, means lips. Thus, the glenoid labrum is the soft and pliable cartilaginous ‘lip-like’ cup that helps to cushion and actually ‘suck’ the head of the humerus (the ball of the shoulder) up against the shoulder’s cartilage socket (the glenoid fossa).
And while labrum can certainly tear due to overuse (particularly true in overhead athletes such as pitchers, swimmers, climbers, etc), the most common cause pf the SLAP tear is probably trauma — a fall onto an outstretched arm, getting the arm jerked by a dog on a leash or water ski tow-rope, an UGLY CAR ACCIDENT, or any number of others. All of which begs the question; what exactly is a SLAP lesion?
SLAP is an acronym for Superior Labrum, Anterior to Posterior. Although the labrum can tear anywhere (a Bankhart Tear is one such example), the most common place for it to tear is along the top (superior) margin, with the tear running horizontally (anterior to posterior). Honestly, they could just have easily called it posterior to anterior, a ‘SLPA lesion’ doesn’t sound as catchy as a SLAP. There are four chief kinds of SLAP tears.
Research has shown that SLAP tears are not always easily classified and that there is frequently a great deal of crossover from one lesion to the next. Also remember that unlike most classification systems (think ANKLE SPRAINS or ACROMIOCLAVICULAR SEPARATIONS here), this one is purely based on injury type, and not injury severity. In other words, a Type III labral tear is not necessarily worse than a Type II.
- TYPE I SLAP TEAR: These are characterized by fraying and soft tissue degenerative changes and are not considered a surgical problem because the labrum and biceps tendon is still anchored to the bone (if surgery is required it’s simple debridement that does not necessitate re-anchoring the labrum to the bone. In similar fashion to the ASYMPTOMATIC DISC HERNIATION, it is thought that the majority of individuals over the age of fifty have some degree of a Type I SLAP Tear. The Type I tear is typically worse in the posterior aspect (back) of the labrum, meaning it’s likely your pain will be in the back of the shoulder — not so much the shoulder blade but the back of the shoulder itself. Honestly; if you have a SLAP this is the SLAP you would rather have. While all areas of the labrum have a poor blood supply, the posterior aspect is better-supplied than the anterior (front), giving it the best hope for healing without surgery.
- TYPE II SLAP TEAR: This type of tear is the most common, the most associated with the term SLAP, and the most frequent to be dealt with surgically. It involves a tearing away of the BICEPS TENDON (the long head of the biceps) at it’s upper attachment. According to Harvard grad and sports orthopedic surgeon, Dr. Patrick McCulloch, most Type II SLAP Tears occur in the posterior labrum as well, although I’ve seen plenty of experts touting the opposite (as you’ll soon see, disagreement is the norm when it comes to diagnosing and treating SLAP tears). Many surgeons caution that while a surgical repair may be appropriate for younger patients, increasing caution is advised as far as surgical intervention for the over-40 crowd. If surgery is required, the Type II SLAP is definitely an ordeal, requiring several weeks in an immobility sling followed by several months of therapy.
- TYPE III SLAP TEAR: This is the “bucket handle tear” where the top part of the labrum peels away from the bone without tearing the biceps tendon as occurs in the Type II. In most cases the Type III SLAPS are not surgical cases, and in concert with the Type I, will only require debridement if surgery is needed.
- TYPE IV SLAP TEAR: This is a combination between the Type II and Type III. There is a “bucket handle tear,” and peeling away of the top of the labrum from the glenoid fossa, but there is also damage to the biceps tendon.
- OTHER SLAP TEARS: There are at least six more classifications of SLAP tears (V-X), with some having numerous sub-classifications.
All good to know but the chief question people want answered is how to determine whether or not they may have a tear of their glenoid labrum? Let’s first look to the symptoms of a SLAP tear. I must warn you that they are not super helpful because they are similar to the symptoms of other shoulder problems; pain, restricted motions (particularly overhead motions) as well as weakness. Also, like other shoulder problems, there is an increased incidence of popping, grinding, or clunking of the joint that can, in some instances, cause it to catch.
The next step is to run through some simple orthopedic tests to try and differentiate what might be going on. Although these tests can be helpful on some level, they do not provide slam-dunk diagnosis as some have claimed. For instance……
“MEDLINE, EMBASE, and The Cochrane data bases were searched for studies published between January 1970 and June 2004 (total yield, 260 articles). Additional studies were sought in the reference lists of relevant articles. Of 29 potentially relevant studies, 15 were selected when the full text was reviewed.
The physical tests included from 1 to 6 of the anterior slide test, SLAPprehension test, biceps load tests, crank test, O’Brien test, active compression, compression rotation, Speed’s test, Yergason’s test, Jobe test, bicippital groove pain, and pain provocation. The likelihood ratios for these tests could not rule in, or rule out, the presence of a SLAP lesion.” From a 2010 issue of the Clinical Journal of Sports Medicine (Physical Examination Tests are not Valid for Diagnosing SLAP Tears: A Review)
“Shoulder pain is a common clinical problem, and numerous tests are used to diagnose structural pathology. MEDLINE, PEDro, AMED, PsychInfo, Cochrane Library (2009) and CINAHL were searched from the earliest record on the database to June 2009. Thirty-six studies were included with a mean methods score of 57%. Seventeen studies were deemed to be of high quality; high-quality studies were less likely to meet the pre-agreed level of reliability.
The majority of studies indicated poor reliability for all procedures investigated. Overall, the evidence regarding reliability was contradictory. There is no consistent evidence that any examination procedure used in shoulder assessments has acceptable levels of reliability.” From a 2010 issue of Physiotherapy (Reliability of Physical Examination Tests Used in the Assessment of Patients with Shoulder Problems: A Systematic Review)
“Ninety-three patients underwent physical examination for SLAP lesions. When using the presence of a SLAP lesion as disease positive, none of the tests was sensitive. None of the tests was found to be clinically useful for predicting repairable SLAP lesions….
Our study demonstrates that the physical examination tests for SLAP lesions are poor diagnostic indicators of disease. Performing a combination of tests will likely help, although the magnitude of the improvement is minimal. These authors caution clinicians placing confidence in the physical examination tests for SLAP lesions.” From the October 2017 issue of the Surgery Journal (Clinical Assessment of Physical Examination Maneuvers for Superior Labral Anterior to Posterior Lesions)
“The literature currently used as a reference for teaching in medical schools and continuing education lacks the necessary validity to help rule in or out a SLAP lesion or biceps tendon involvement. Based on the results from the systematic review conducted by Calvert, no tests clinically diagnose a SLAP lesion. This is a cause for concern as magnetic resonance imaging or magnetic resonance arthrography, which are frequently used to assess a possible SLAP lesion, may also have diagnostic flaws and may be cost prohibitive.
Performing arthroscopy on every patient to rule the condition in or out is unethical, especially if a SLAP lesion is not present.” From the December 2013 issue of the Journal of Athletic Training (Special Physical Examination Tests for Superior Labrum Anterior-Posterior Shoulder Tears: An Examination of Clinical Usefulness)
“The combination of the anterior slide test with a history of popping, clicking, or catching had moderate diagnostic utility for confirming type II to IV SLAP lesions. No single item or combination of history items and physical examination tests had diagnostic utility for type I SLAP lesions.” From a 2011 issue of the Journal of Athletic Training (Diagnostic Accuracy of History and Physical Examination of Superior Labrum Anterior- Posterior Lesions)
So; if these tests aren’t wonderful, what should you do? Run them anyway because some studies show that the more of them that are positive (cause pain) the greater the chances a SLAP lesion is present. Rather than me explain each and every one, I am simply going to provide you with a link to a YouTube video that will explain the test and show you how to do it. Again, according to the most current research available, take the results of these tests with a grain of salt.
- O’Brien’s Test (aka Active Compression Test) —- HERE.
- Passive Distraction Test — HERE.
- Biceps Load Test — HERE.
- Dynamic Labral Shear Test — HERE.
- Compression Rotation Test (Grind Test) — HERE. This test is similar to the ANTERIOR SLIDE TEST.
- Shoulder Apprehension Test (Crank Test) — HERE.
- Clunk Test — HERE.
- Biceps Muscle Tests (SPEED’S TEST & YEARGASON’S TEST)
SLAP LESION SCHZOPHRENIA, OR WHY CONSERVATIVE TREATMENT IS WARRANTED IF A SLAP TEAR IS SUSPECTED

The Proverbs tell us that a double-minded man is unstable in all his ways. As I will show you, when it comes to SLAP tears, things go way beyond double-mindedness —- almost to the point of full-blown schizophrenia. What do I mean? Only that the only consensus among orthopedic experts and the medical research community concerning SLAP lesions is that there is no consensus. None. Think I’m being harsh or making things up?
Why else would a 2015 issue of Arthroscopy carry a paper titled Lesions of the Superior Labrum From Anterior to Posterior (SLAP) Are a Slap in the Face to the Traditional Trinity of History, Examination, and Imaging, which concluded simply; “The current literature and practice for making the SLAP diagnosis are variable and inconsistent…..“?
Or you could take a peek at the conclusions of this past January’s issue of EFORT Open Reviews (SLAP Lesions: Current Controversies). “Despite the plethora of literature regarding SLAP lesions, their clinical diagnosis remains challenging for a number of reasons. The diagnostic value of many of the available physical examination tests is inconsistent and ambiguous. SLAP lesions have no specific associated pain pattern.”
In other words, even though there are hundreds upon hundreds of studies on SLAP lesions, tests (in the form of both orthopedic testing and as you’ll soon see, advanced imaging) don’t do a great job of creating a definitive diagnosis. Allow me to provide you with a number of similar statements taken straight from the mouths of some of the world’s foremost authorities on SLAP lesions (many are CHERRY-PICKED, of course, due to constraints on time and space).
“SLAP lesions were first classified by Snyder in 1990. Results of treatment have been controversial without clear consensus. Most SLAP lesion patients are ultimately treated non-operatively.” From the Open Orthopedics Journal — the July 2018 issue (SLAP Lesions, An Opinion Piece)
“Controversies exist in the classification and management of superior labral anterior and posterior (SLAP) lesions. There is low interobserver agreement in classifying SLAP lesions. The most common misdiagnosis of type I lesion was as a type II, and vice versa.” From the February 2018 issue of JSES Open Access (Current Trends in the Evaluation and Treatment of SLAP Lesions: Analysis of a Survey of Specialist Shoulder Surgeons).
Think about this for a moment — Type I SLAP’s are not usually a surgical problem (and if required, is minor) but are routinely confused with the SLAP that’s most likely to require surgery, Type II.
“Non-operative treatment with an appropriate regimen provided satisfactory clinical outcomes in middle-aged patients with symptomatic SLAP lesions and should be considered before recommending operative treatment. Non-operative management could be applied as primary treatment for patients with symptomatic SLAP.” From the October 2017 issue of Knee Surgery, Sports Traumatology and Arthroscopy (Clinical Outcomes of Non-Operative Treatment for Patients Presenting SLAP Lesions in Diagnostic Provocative Tests and MR Arthrography)
“Although many SLAP tears require surgery, the mainstay of initial treatment is nonoperative. In general, Type I and III lesions (intact biceps anchor) are suitable for simple debridement.” From JB & JS Orthopedic Education (Clinical Summary: Labral Tears of the Shoulder)
To sum things up, the diagnosis and care of SLAP lesions is not quite as it’s been historically portrayed by the practicing orthopedic community. For proof that this same principle pertains to diagnostic imaging, look no further than a study published in the June 2014 issue of the British Journal of Radiology (How Often do Surgeons Intervene on Shoulder Labral Lesions Detected at MR Examination? A Retrospective Review of MR Examinations Correlated with Arthroscopy).
After describing numerous studies with similar conclusions, and before a discussion of which SLAP lesions actually require “tacking” surgery as opposed to simply ‘cleaning up the joint’ (debridement), the author — a practicing ortho — made this statement…..
“In our practice, labral tears are commonly seen and described on MR examination…. However, some of these tears might not be considered clinically significant by a surgeon. In particular, a high percentage of SLAP and posterior labral tears described on MR examination were described as fraying at arthroscopy. Most of these tears did not have [require or need] surgical tacking performed.”
In another study, this one from a 2015 issue of the Open Access Journal of Sports Medicine (Magnetic Resonance Imaging Arthrography Following Type II Superior Labrum From Anterior to Posterior Repair: Interobserver and Intraobserver Reliability), researchers had three different individuals — two different radiologists and an elite shoulder orthopedic surgeon — independently review the diagnostic imaging both pre-surgery and two years post-surgery in order to see the level of agreement between the three.
“On average, 54% of MRAs were interpreted as healed SLAP repairs while 46% of MRAs were interpreted as having a re-torn SLAP repair. Overall, only 43% of the studies had 100% agreement across all interpretations. The interobserver reliability between readers ranged from 0.13 to 0.44. The routine use of MRA in the evaluation of type II SLAP lesion repair should be utilized with caution.”
As you might guess, between 13% and 44% agreement among highly trained professionals is not exactly a ringing endorsement of MRA. Speaking of MRA…..
This would be a good time to further discuss the chief ways that the medical community uses imaging to diagnose SLAP lesions — MRI, either with or without contrast (with contrast is called MRA or arthrography) or a CT SCAN with contrast dye.
However, after seeing some of the quotes above concerning conservative, non-surgical treatment to be the first option for addressing SLAP lesions, particularly in the older non-athlete or recreational athlete, does it make sense to run out and get an MRI right away — particularly with what we know about their accuracy when it comes to these types of shoulder problems?
Honestly, we could ask the very same thing of rotator cuff problems as well (SHOULDER IMPINGEMENT). For those who are wondering, let’s see what the peer reviewed science has to say about diagnosing SLAP tears using today’s most advanced imaging technology. You will note some overlap with the orthopedic tests we’ve already discussed.
“MRI was not accurate for the diagnosis of SLAP lesions.” Conclusions of a 2006 study from the Journal of Elbow & Shoulder Surgery (Magnetic Resonance Imaging Accuracy for the Diagnosis of Superior Labrum Anterior-Posterior Lesions in the Community Setting: Eighty-Three Arthroscopically Confirmed Cases)
“Superior labral tears are diagnosed with high frequency using MRI in 45 to 60-year-old individuals with asymptomatic shoulders.” From the January 2016 issue of the Orthopedic Journal of Sports Medicine (High Prevalence of Superior Labral Tears Diagnosed by MRI in Middle-Aged Patients With Asymptomatic Shoulders)
“83 of the 90 patients had glenoid labrum tears at arthroscopy. Only 54 were correctly identified at MRA. All normal glenoid labra were identified at MRA. This gave a sensitivity of 65% in identification of all types of glenoid labrum tear. 74 patients had anterior glenoid labral tears that were detected at an even lower rate of sensitivity (58%).
The sensitivity of MRA in this series was substantially lower than previously published, suggesting that MRA may not be as reliable a diagnostic imaging modality in glenohumeral instability as previously thought.” From the June 2012 issue of Acta Orthopedica (Is MRA an Unnecessary Expense in the Management of a Clinically Unstable Shoulder? A Comparison of MRA and Arthroscopic Findings in 90 Patients)
“There are several tests that the physician can perform that may indicate a torn labrum, but these tests are not always accurate. Some physicians feel very confident that they can make the diagnosis of a labral tear upon physical examination, but this is controversial. As a result of this uncertainty, other studies can be done to confirm the diagnosis if it is suspected.
The best tests available to make the diagnosis of a labral tear are magnetic resonance imaging (MRI) scans or a test called a CT-arthrogram (the latter is a CAT scan preceded by an arthrogram where dye is injected into the shoulder)…. Neither of those tests is currently very good at making the diagnosis of a SLAP lesion.” From Johns Hopkins University (Shoulder Labrum Tear)
“In our retrospective study of 444 patients, sensitivity, specificity, and accuracy were all lower than previously reported in the literature for diagnosing SLAP lesions. Our data indicated that while MRI could exclude a SLAP lesion, MRI alone was not an accurate clinical tool. MR arthrography had a large number of false-positive readings in this study. We concluded that even with intra-articular contrast, MRI had limitations in the ability to diagnose surgically proven SLAP lesions.” From the September 2015 issue of Knee Surgery, Sports Traumatology and Arthroscopy (Accuracy of Magnetic Resonance Imaging to Diagnose Superior Labrum Anterior-Posterior Tears)
“Type II SLAP tears are considered the most common type of SLAP lesions. However, the management of type II SLAP tears in middle-aged patients is challenging because recent evidence suggests that there is a high prevalence of type II SLAP lesions in the asymptomatic middle-aged shoulder.” From the July 2018 issue of Arthroscopy (Editorial Commentary: Pursuit of Value-Based Care for SLAP Lesions: More Work to Be Done)
“As imaging continues to improve and more people undergo MRI studies, physicians are finding that a significant percentage of people within the general population have labral changes that do not cause symptoms or need repair. In particular, there are age-related changes that can cause degenerative splits and tears in the labrum. While they may not be symptomatic, visually they can mimic a SLAP lesion. When these appear in MRI studies, misleading assumptions may be made between the images and the patient symptoms….
The dynamic labral shear test has proved to be more reliable than MRI or arthroscopic findings in determining whether the patient’s symptoms are caused by SLAP lesions. It comes back to something we learn in orthopedics very early: Often the clinical assessment of the patient is the most reliable way to determine what is causing the pain.” From the Mayo Clinic’s article, Shoulder Pain: Raising the Level of Diagnostic Certainty About SLAP Lesions
“Miniaci found that 79% of asymptomatic professional pitchers (28/40) had ‘abnormal labrum” features and noted that “magnetic resonance imaging of the shoulder in asymptomatic high performance throwing athletes reveals abnormalities that may encompass a spectrum of ‘nonclinical’ findings.’ Yes, you can have a torn labrum and not be in pain. The general population may be even worse, particularly as folks age. Yes, you can have a torn labrum and not be in pain” From Eric Cressy’s article, Healthy Shoulders with Terrible MRIs?
One item of note here. Although there were studies doubting the veracity of MRA for assessing SLAP tears, there were also studies touting their benefits. Some studies showed that as long as your MRI was done in a machine that used a larger magnet (3 Tesla as opposed to 1.5 Tesla), results were not only better, but regular MRI was equal to MRA, meaning you may be able to get by without gadolinium dye injected into the shoulder.
Be aware that this is its own double-edged sword, considering that some experts have said that 100% of those getting an MRA will be diagnosed with a SLAP — another great example of OVERDIAGNOSIS & OVERTREATMENT and still another reason to try conservative methods first.
“Improved diagnostic accuracy for SLAP tears is seen with 3-T compared with 1.5-T MR imaging, with or without intra-articular contrast material. Regardless of MR findings, however, physicians should be cautious when recommending surgery in the patient with a vague clinical picture.” From last July’s issue of The Open Orthopedic Journal (MR Imaging of SLAP Lesions
Bottom line, advanced imaging does a good job of finding SLAP lesions. But as you have seen, this itself can be problematic considering just how many of these are asymptomatic — not the source of the shoulder pain. In fact, in light of the scientific literature there are some experts who believe SLAP tears are, at least in many cases, little more than a sign of normal aging.
While my knowledge of BIOMECHANICS would force me to to argue against this at least on some level, the fact remains that seeing a SLAP on a test can have much less bearing on your shoulder pain than you’ve been led to believe. This itself begs another question — the question many of you problem jumped ahead to.
WHAT CAN BE DONE TO ADDRESS SLAP TEARS NON-SURGICALLY?

There are many studies on SLAP tear surgeries that tout success rates of over 90%. What you need to understand, however, is that their criteria for success and your criteria for success may be radically different. It’s not difficult to find online articles explaining how these huge success rates are being manipulated.
If you are not aware of the ways that research can be manipulated to achieve a desired outcome, you need to spend some time reading my EVIDENCE-BASED MEDICINE column. For instance, numerous studies tout improvement of various test scores without really revealing how minimal these improvements really are. And then there are the guidelines for shoulder injuries.
Knowing what a huge fan of MEDICAL GUIDELINES I am (not), let’s see what they have to say concerning SLAP lesions. Guideline Central (Shoulder Conditions Diagnosis and Treatment Guidelines) essentially said that the criteria for SLAP repair surgery was a traumatic event leading to shoulder pain, pain with ortho tests, and a positive MRI, after at least trying six weeks of conservative care.
Firstly, we I’ve already shown you how poor provocative orthopedic testing is regarding diagnosis of SLAP tears. And secondly, six weeks of conservative care is not a lot of time when it comes to making changes in a shoulder.
Realize that my approach to shoulder care is different, as I will show you momentarily. I examine people and if I think I may be able to help, will treat patients once to see how they respond. If they respond favorably, more treatment may be needed. If not, this does not mean surgery is warranted — it simply means that a longer-term conservative approach may be called for. Probably longer than six weeks.
This was confirmed by the 2018 recommendations of the National Athletic Trainers’ Association (NATA), which stated that “Patients with SLAP lesions should undergo 3-6 months of nonoperative management with the goals of decreasing pain, improving shoulder function, and returning to previous activity levels.”
This tells me that not only is it possible to recover from a SLAP (particularly in light of THIS STUDY of professional baseball pitchers — “There were no significant differences in magnetic resonance imaging findings of the supraspinatus and infraspinatus tendons between the throwing and non-throwing shoulders. The labrum was abnormal in 79% of the 28 shoulders.”), but 3-6 months is a more realistic amount of time frame. Do conservative methods work?
The October 2015 issue of the World Journal of Orthopedics (Superior Labral Anterior Posterior Lesions of the Shoulder: Current Diagnostic and Therapeutic Standards) had this to say about the conservative care of SLAP tears, even though the authors — orthopedic surgeons — very much touted surgery.
“SLAP I lesions predispose to a conservative treatment in absence of other intra-articular pathologies. Non-operative treatment for SLAP tears in overhead athletes has been suggested by Edwards et al, who showed a 66% of throwers being able to return to play at the same or better level than before.”
This is similar to the conclusions of the August 2012 issue of Orthopedics Today, where the authors were providing commentary concerning a brand new study (a paper presented at 2012’s American Orthopaedic Society for Sports Medicine Annual Meeting in Nashville) on the use of conservative methods for treating professional baseball players with SLAP tears.
Listen to their conclusions. “Nonsurgical treatment for SLAP lesions in professional baseball players can result in a high rate of return to previous performance.” The kicker is that if the SLAP is dealt with surgically, experts know there is likely to be a significant dip in performance. Listen to the words of author John Kuhn, and ortho at Nashville’s Vanderbilt University…..
“Nonoperative treatment focused on treating scapular dyskinesis, and glenohumeral internal rotation deficits can be successful for many high-level throwers with SLAP Lesions. In those throwers who fail nonoperative treatment, the return to play level was surprisingly poor. With this information, it would appear that surgical treatment of SLAP lesions should only be performed after failure of appropriate rehabilitation, and that surgical treatment should be undertaken cautiously and as a career-salvaging option in the professional thrower.”
Allow me to show you some of the studies that don’t exactly provide a ringing endorsement of SLAP repair surgery. First, if you are seriously considering surgery without undergoing several months of appropriate rehab, be sure to first read the March 2015 issue of Current Reviews in Musculoskeletal Medicine (Complications After Arthroscopic Labral Repair for Shoulder Instability), which discussed some of the SIDE EFFECTS that have been associated with this surgery… “nerve injury, infection, problems associated with suture anchors, chondrolysis (the rapid destruction of articular cartilage), osteoarthritis, post-operative stiffness, and recurrant instability.”
Be aware that some of these findings are present in shoulders of patients whose surgeries have been deemed “successful”. What other tidbits can we glean from looking at studies on surgeries for repairing SLAP tears?
“There are no advantages in repairing a type II SLAP lesion when associated with a rotator cuff tear in patients over 50 years of age.” From a 2008 issue of The American Journal of Sports Medicine (No Advantages in Repairing a Type II Superior Labrum Anterior and Posterior (SLAP) Lesion when Associated with Rotator Cuff Repair in Patients Over Age 50: A Randomized Controlled Trial)
“This review (Twenty-six papers were included; 54% did not report indications for surgery and 89% of papers did not report the criteria for determining completeness of the repair) demonstrated a wide variability in the reported surgical aspects and that a relatively high percentage of papers did not report many of the details.
This lack of precision and consistency makes analysis of individual papers and comparison between papers and their outcomes difficult and does not allow a consensus regarding current practice to be developed. These findings may be some of the factors responsible for the variability in treatment outcomes.” From the abstract of the April 2016 issue of the ortho journal, Arthroscopy (Current Practice for the Surgical Treatment of SLAP Lesions: A Systematic Review)
“A double-blind, sham-controlled trial was conducted with 118 surgical candidates (mean age 40 years), with patient history, clinical symptoms and MRI arthrography indicating an isolated type II SLAP lesion. Patients were randomly assigned to either labral repair, biceps tenodesis or sham surgery if arthroscopy revealed an isolated SLAP II lesion. There were no significant between-group differences at any follow-up in any outcome at 2 years.
Neither labral repair nor biceps tenodesis had any significant clinical benefit over sham surgery for patients with SLAP II lesions in the population studied.” From the December 2017 issue of the British Journal of Sports Medicine (Sham Surgery Versus Labral Repair or Biceps Tenodesis for Type II SLAP Lesions of the Shoulder: A Three-Armed Randomised Clinical Trial)
“Over a 4-year period, 225 patients with a type 2 SLAP tear were prospectively enrolled. Two sports/shoulder-fellowship-trained orthopaedic surgeons performed repairs. 179 of 225 patients completed the follow-up for the study at a mean of 40.4 months.
The mean postoperative range of motion was less than the mean preoperative range of motion. Of the 179 patients, 66 patients (36.8%) met failure criteria. A reliable return to the previous activity level is limited. Age greater than 36 years was associated with a higher chance of failure.” From the April 2013 issue of the American Journal of Sports Medicine (A Prospective Analysis of 179 Type 2 superior Labrum Anterior and Posterior Repairs: Outcomes and Factors Associated with Success and Failure)
“At an average follow-up of 3.1 years in the non-operative group, function improved significantly. Quality of life also improved following treatment. Pain relief was also significant, as visual analog pain scores decreased from 4.6 to 1.9. All eighteen patients reported a return to sports following non-operative treatment, although three did not return to pre-injury levels.
These results were compared to those of a group of 19 patients who had surgical treatment over the same period, and no statistically significant differences were observed in pain relief or functional improvement. Using validated, patient-derived outcome instruments, the present study validates the non-operative treatment of superior labral tears, with improved pain relief and functional outcomes comparable to those seen with operative treatment.
Based on these findings, an initial trial of non-operative treatment may be considered in patients with the diagnosis of isolated superior labral tear.” From a 2007 issue of Arthroscopy (Improved Outcomes with Non-Operative Treatment of Superior Labral Tears)
Whether the SLAP diagnosis is confirmed by an expert or not, not everyone is going to respond to conservative care. But as you can see, the average person has nothing to lose by trying. This is because the literature is clear on two points. First, diagnosing SLAP lesions is extremely difficult in the best of circumstances. Second, virtually all expert recommendations suggest surgery after conservative methods have been tried and failed. In other words, time after time we see studies end with advice to physicians / orthopedists to try conservative care with their SLAP patients first — especially if those patients are over 35.
The following is a list of things that might (emphasis on the word might) help someone with a SLAP lesion — a big deal for those who cannot afford to be off work for the 3 months or more required after a Type-II surgery. This list is not necessarily what I would recommend you do if you thought you had a SLAP tear, but some of what I might consider trying if it were me.
As always, decisions are best made as a joint effort between you and your primary health care provider. Speaking of healthcare providers, before reading the list, listen to this short conversation between two practicing orthopedic sports surgeons (“The Boneheads”) talking candidly about SLAP lesion confusion. https://www.youtube.com/embed/Cd_MqGWzjnA?wmode=opaque
- FIRST MAKE SURE YOU ARE NOT DEALING WITH AN EASILY-FIXED PROBLEM: It might be beneficial to come see me and see if I can help. Not only do we address lots of people’s chronic issues very quickly (HERE or HERE), I frequently see people with shoulder problems (HERE). This goes for at least some of you who have been through shoulder surgery and are still having issues (HERE is a prime example) as well as many who have been diagnosed with who-knows-what shoulder problems. As you should have realized from what you’ve read so far, it’s not uncommon for SIMPLER SHOULDER PROBLEMS to mimic more complex shoulder problems.
- REDUCE INFLAMMATION & TAKE THE RIGHT SUPPLEMENTS: This is mostly about diet, but also involves nutritional supplements such as collagen / bone broth, Ligaplex, fish oil, tumeric, coconut oil, etc, etc, etc.
- WHAT KIND(S) OF INJECTIONS TO CONSIDER? While you can be certain that doctors will recommend a CORTICOSTEROID INJECTION to reduce the inflammation in your shoulder, a quick look at four decades of studies shows just how misguided this really is. Instead, you might want to see someone who is versed in injecting shoulder joints with substances like BPC-157, HGH, PRP, Stem Cells or the German homeopathic remedy, TRAUMEEL. I have seen instances where physicians who practice this way “stack” several of these together to create something can can potentially generate true healing synergy. Used correctly we are talking about very low side effect profiles and a fighting chance to provide a healing boost to the blood-starved labrum. While I’m not really a fan of injections, they are much better than surgery.
- USE YOUTUBE TO YOUR ADVANTAGE: I can’t begin to tell you how the times that my son and I have fixed vehicles, appliances, and done who knows what kinds of repairs to the house or office by using information from YouTube videos. Is it all good, helpful or beneficial? No. But there is a lot of material on there that is both excellent and free — a good combination for the average person who understands what it’s like to ride the MEDICAL MERRY-GO-ROUND. SmashWeRx has three videos that have some great stretches and exercises (HERE, HERE, and HERE). Phase I and Phase II rehab of SLAP shoulders can be found HERE and HERE. DR. JO and DR. QUINN both have nice offerings in this department. WOD DOC and LIVESTONG each have something to offer as well. And while it’s not a YouTube video, THE CLIMBING DOC also offers a nice tutorial. My advice when starting a rehab program is to start slow and not add too many things in at once so you know what works and what may be an aggravating factor.
- CHECK OUT MY DIY ANTI-INFLAMMATION, RETURN-TO-HEALTH PAGE: Look folks, whether you have a SLAP tear or MS, I don’t claim for even one second to have the solution for everyone. However, when you start living your life differently, good things start to happen (HERE).
- OTHERS: This list is far from comprehensive. LOW LEVEL LASER THERAPY (may require a Class IV) might prove extremely effective. There are any number of supplements and exercises / stretches that were not mentioned that might prove beneficial. And that’s just for starters. Never get complacent — continue your quest to heal your shoulder without surgery because a solution may be right around the corner. Remember that most of the pain is not caused by the torn labrum itself, but by the TRIGGER POINTS in response to the funky mechanics that may very well have led to the labral tear in the first place. These can be found in all ROTAOR CUFF MUSCLES, the LEVATOR & PEC MINOR, TRAPEZUIS and several others. This is why you must deal with underlying causes of the SLAP such as GIRD (glenohumeral internal rotation deficit) and scapular dyskinesis (tons of YouTube Videos for each). And if you do wind up needing surgery, find the best-qualified, most conservative-minded person you can, and make sure to go into the surgery WITH THIS MINDSET.
Since shoulder problems are said to be the number two or three most-common musculoskeletal problem seen by doctors, we all know people who could benefit from this information. Be sure and spread this message by liking, sharing or following on FACEBOOK since it’s a nice way to reach the people you love and value most!
