Back in June a team of Swedish researchers put together a study for the Journal of Pain Research titled Exploring Patients’ Experiences of the Whiplash Injury-Recovery Process. Knowing what we already know about recovery from whiplash injuries (OVER 50% OF THOSE INJURED — MOSTLY WOMEN — WILL DEAL WITH CHRONIC SYMPTOMS FOR THE REST OF THEIR LIVES), listen to how these authors described the feelings that are found hand-in-hand with whiplash. Before you write someone off who has been “whiplashed,” read through this CHERRY-PICKED paragraph a couple of times…..
“Approximately 50% of patients with WAD (whiplash-associated disorders) have long-term symptoms after their injury, and a large proportion are reported to have poor quality of life. Additionally, 13–50% are unable to work or participate fully in their daily activities. Changes in self-image were difficult to cope with and likely led to perceived stigmatization. Struggling with feelings of loss of control appeared to lead to low confidence and insecurity. The participants talked about pain and other symptoms interfering with their lives and about the loss of hope, ability, social roles, autonomy, and spontaneity. The participants also noted that it was difficult to continue exercising even though they believed exercise was beneficial. The participants believed that they had lost the physical capacity they had before the injury, and they felt sad and helpless about all physical, psychological, and social losses that were consequences of WAD. The participants struggled with their confidence in their ability to control their pain and daily life. Low perceived control appeared to lead to low confidence and insecurity regarding the ability to manage injury-related problems and the future. The perceived severity, manageability, and realistic expectations of symptom development also influenced the participants’ feelings of control. Severe symptoms were difficult to tolerate and manage and decreased the participants’ beliefs and confidence regarding their ability to control the situation. The participants did not always know what worsened pain and other WAD-related symptoms. The participants tried to determine how to control their situation but did not often succeed. Returning to work was perceived as a challenging outcome. The combination of expectations regarding recovery and daily experiences of fluctuating symptoms decreased the participants’ confidence concerning the future and their return to work.”
Thus, it’s not too surprising that the same study went on to use these words / terms when describing the effect that chronic whiplash symptoms have on people.
“Loss of ability, loss of confidence, loss of freedom, loss of hope, slavery [to pain] abandoned by those around, loss of social roles, frustration, fear, distress, sadness, worry, negative moods, stigma, chaos, mystery, a riddle needing answers, incongruities, unsure about future, changed self-image, struggling with control…..”
Unless you deal with these types of patients on a day-to-day basis, it doesn’t make sense. It seems overblown. Over-the-top. Exaggerated. Pretentious hyperbole. Not only is it not an elaboration, the above quotes should help one understand a concept commonly seen in those injured by whiplash — something known as “catastrophizing“.
Catastrophizing is the belief that something, one’s pain, the ability to function, or possibly even the future, is or may be much worse or bleaker than it actually is or will be. Also known as “cognitive distortion,” Wikipedia describes it as “exaggerated or irrational thought patterns involved in the onset and perpetuation of psychopathological states, especially in those more influenced by psychosocial factors, such as depression and anxiety.” All the more important to understand once you realize how often DEPRESSION and ANXIETY plague whiplash sufferers. Allow me to show you just how real this phenomenon of catastrophizing really is in many trying to cope with chronic neck pain.
Lat month’s issue of Somatosensory & Motor Research (Observing Neck Movements Evokes an Excitatory Response in the Sympathetic Nervous System Associated with Fear of Movement in Patients with Chronic Neck Pain) showed that for someone with serious neck pain related to movement, just looking at neck movements (pics or video) can invoke a fear-based response of the SYMPATHETIC NERVOUS SYSTEM (fight or flight).
“The objective of this study was to evaluate the response of the sympathetic-excitatory nervous system in patients with chronic neck pain compared with a control group of asymptomatic subjects who underwent an intervention of watching activities involving movements in the neck region. The ANOVA test revealed significant differences in the increase in skin conductance in the chronic neck pain group after observing the activities (both in the photographs and video) at the end of the observation and 5 minutes after the intervention. Ultimately, the correlation analysis revealed a moderate positive correlation between kinesiophobia [fear of movement] and skin conductance at 30 seconds and at 60 seconds of observing the activities in the video for the chronic neck pain group. Based on the results of the present study, we suggest that observing activities involving neck movements causes an activation of the sympathetic-excitatory nervous system in patients with chronic neck pain. These changes could be related to a fear of movement when faced with visual exposure to neck movements that could be interpreted as ‘harmful’ or ‘dangerous’.”
Although some may balk at using the term PTSD (post-traumatic stress disorder) to describe whiplash sufferers, whiplash and MVA (motor vehicle accidents) have been widely recognized as a common cause for decades. Less than a month ago, the European Journal of Pain (Trajectories of Post-Traumatic Stress Symptoms After Whiplash) came to some shocking conclusions. The Danish research team looked at PTSD ‘predictors’ (“pain, fear-avoidance-beliefs, pain-catastrophizing, depression……“) and determined that although most people (75%) involved in a whiplash accident showed little or no signs of PTSD, 25% did. Of that 25%, about 40% recovered fully from the PTSD within six months.
However, the rest of the rest (60%) were labeled “chronic,” and were described as having, “high initial PTSD symptom levels and a small increase over time. Initial higher pain and depression levels predicted the recovering and chronic trajectories. The chronic trajectory suggested that a significant subset of people does not recover from PTSD symptoms. This class also reported more pain-related disability.” In other words, about 15 out of 100 who had at least a degree of PTSD got worse. 15% may not seem like a big number until you start grasping that there are several million such injuries each year.
What’s regrettable about this situation is how these individuals are dealt with by the largest portion of the medical community. Even though whiplash research abounds, the chief forms of medical treatment have remained the same as they were since long before I was in practice (I graduated in 1991). In fact, things may have gotten worse. Case in point, a study from last month’s issue of Emergency Medicine Australasia (Use of and Attitudes to the Role of Medication for Acute Whiplash Injury: A Preliminary Survey of Emergency Department Doctors) looked at the most commonly prescribed drugs for WAD in an ER setting (NSAIDS — 78% of the time, PARACETAMOL, what the rest of the world calls acetaminophen — 75% of the time, OPIOIDS — 44% of the time, and benzos — 11% of the time). The authors also concluded that “most [ER docs] were comfortable to prescribe pregabalin” and that “opioids appear to be over-prescribed“. For the record, pregabalin (LYRICA) is a terrible drug for most people (HERE). Bottom line, far too many people end up on “THE BIG FIVE” or worse after an MVA.
Although there are an almost unlimited number of ways that people end up being “WHIPLASHED,” MVA (motor vehicle accidents) are far and away the most common. Although there are many potential tissue culprits as far as the source(s) of said pain, the CERVICAL FASCIA is arguably one of the most common causes — particularly when it comes to CHRONIC NECK PAIN. The only reason I use the word ‘arguably’ is because since the CF does not show up on standard advanced imaging such as MRI (HERE), it’s completely off the radar of the average physician. It’s a large part of what makes fascia chronic pain’s PERFECT STORM. And although the authors were talking about TRIGGER POINTS as opposed to the flip side of the myofascial syndrome (SCAR TISSUE / FIBROSIS), listen to what the National Fibromyalgia & Chronic Pain Association (Cervical Myofascial Pain) said about this phenomenon — a phenomenon you will see as a common theme in today’s post. “The diagnosis of this syndrome is clinical, with no confirmatory imaging or laboratory tests available.”
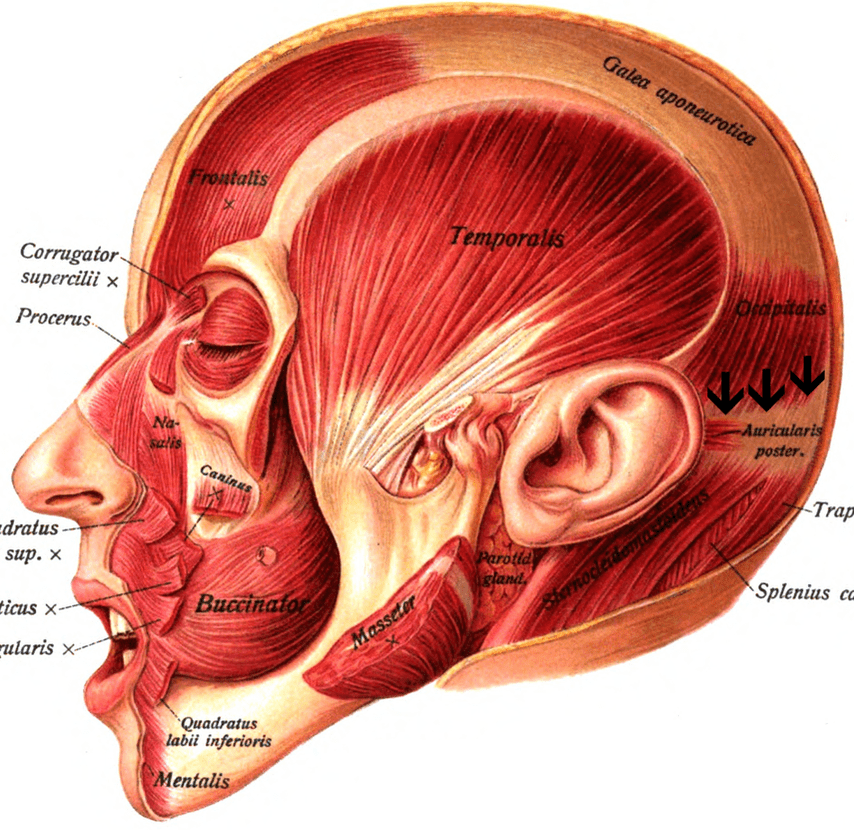
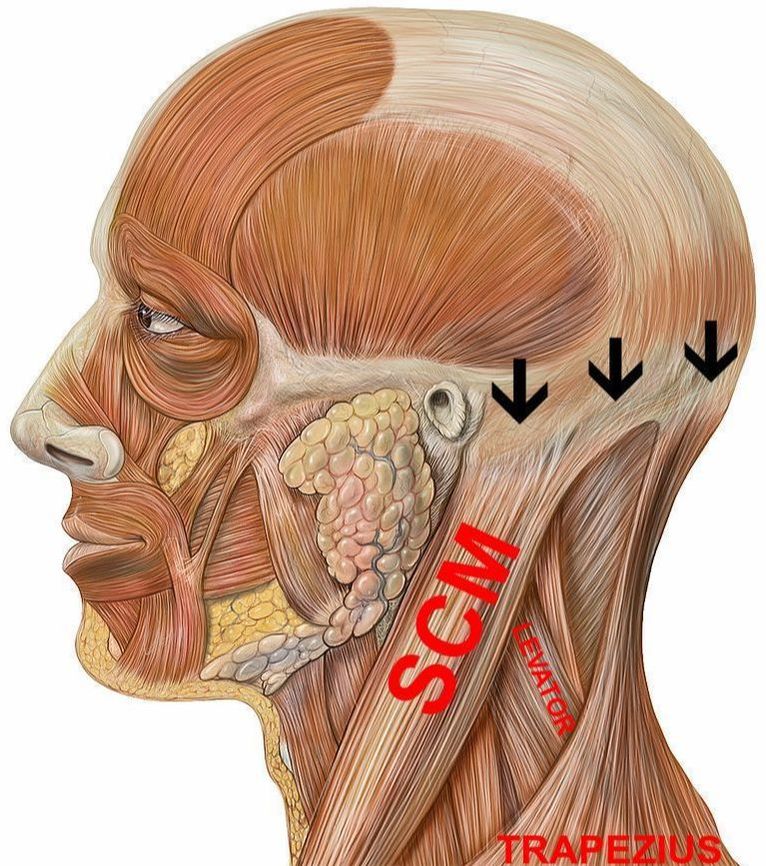
Although the pictures below do not show much fascia (aside from the GALENA APONEUROTICA — the fascia on top of the skull), don’t forget that it’s there. The large arrow in the middle of the page is where the external occipital protuberance (EOP) is, which happens to be the center of the occipital ridge (see arrows on all three pictures). As you can see, a number of large muscles anchor to this ridge, and thanks to Wolf’s Law (bone grows in response to mechanical stress, whether that stress is normal or abnormal), you can feel these attachment points — particularly if you have been living with extensive amounts of mechanical stress (excessive pulling) in your neck region (FHP is one of the more common of these). Just how big is this problem of Forward Head Posture (perpetual cervical flexion)?
The August issue of the Journal of Electromyography and Kinesiology described this relationship between PROPRIOCEPTION AND FASCIA and other connective tissues in a study titled Disturbance of Neck Proprioception and Feed-Forward Motor Control Following Static Neck Flexion in Healthy Young Adults. To understand how big a deal this study really is, it’s important to grasp the fact that CERVICAL EXTENSION (the opposite of cervical flexion, which describes one’s ability to tip one’s head backwards, hopefully to the point that the forehead is parallel to the floor) is arguably the most important range of motion in the body.
“The highly complex proprioceptive system provides neuromuscular control of the mobile cervical spine. Static neck flexion can induce the elongation of posterior tissues and altered sensory input from the mechanoreceptors…. Following flexion, the absolute and variable errors in head repositioning significantly increased. The results also showed that there was a significant delay in the onset of myoelectric activity of the cervical erector spinae muscles after flexion. The results of this study suggested that a 10-min static flexion can lead to changes in the neck proprioception and feed-forward control due to mechanical and neuromuscular changes in the viscoelastic cervical spine structures. These changes in sensory-motor control may be a risk factor for neck pain and injury.”
And if you already have pain and injury, there is great potential to form a vicious cycle of pain, dysfunction (including abnormal proprioception), and the subsequent degeneration that always follows close on their heels.
RESEARCH CONCERNING NECK,
WHIPLASH, AND HEADACHE SYMPTOMS

Because neck pain can be both debilitating and progressively degenerative (the “vicious cycle” mentioned above), it makes sense that drugs from the “Big Five” class are not going to help you, even though if you have read this far you have probably been prescribed all of them and then some. Something must be done to take mechanical stress off of the soft tissues and facet joints. While I am a huge fan of various forms of body work and massage, I frequently deal with the people who, while they might be helped by massage, chiropractic adjustments, or various forms of THERAPY, the relief is always short-lived (HERE), much of which is due to the nature of FASCIA and the subsequent “FASCIAL ADHESIONS” that can form in these tissues due to trauma, repetitive movements or jobs, or postural considerations.
As I’ve shown you in the past, the endproduct of inflammation is always fibrosis (HERE). While a certain amount of this is a good thing (LOCAL INFLAMMATION is critical for healing injured connective tissues), too much inflammation (SYSTEMIC INFLAMMATION) coursing through your body is not only detrimental but highly detrimental. This is why those of you struggling with situations like these or others (UPPER CROSSED SYNDROME, LOWER CROSSED SYNDROME, etc, etc) must get your act together as far as what you are eating, how you are living, as well as the chemicals you are exposing yourself to on a day-by-day basis. Before we delve more into the specific issue of what it might take to get you on the road to recovery, let’s take a few moments to look at the latest research on all things neck pain.
When you see the term “Cervicogenic Headache,” know that it refers to headaches that are being generated by abnormal structure or function of the cervical spine (chiros refer to this dysfunctional alignment and motion as “SUBLUXATION“). I bring this up because authors of an article from a June issue of the medical educational journal, StatPearls, wrote of the relationship between the nerves in the top of the neck and headaches. “A cervicogenic headache is thought to be referred pain arising from irritation caused by cervical structures innervated by spinal nerves C1, C2, and C3; therefore, any structure innervated by the C1–C3 spinal nerves could be the source for a cervicogenic headache. It is predominant in females. Pain can mimic primary headache syndromes such as tension headache or migraine headache.”
Best way to solve this issue? “Manipulative therapy and therapeutic exercise regimen are effective in treating a cervicogenic headache. …..72% of patients had achieved a reduction of 50% or more in headache frequency at the 12-month follow-up, and 42% of patients reported 80% or higher relief of some sort.” Hang on because I will shortly address a common reason that adjustments don’t work (or don’t hold very long) for a significant portion of the population.
For the record, this study also stated that “the source of the pain must be in the neck and perceived in the head or face.” If you have followed my site you are already aware that I have written extensively about both SKULL PAIN and FACE PAIN. What I have found with face pain is that it’s more frequently solvable when it can be tied to a specific trauma. A recent study from Neuroimage Clinical helps spell out the reason for this — the pain can come from BRAIN ABNORMALITIES.
“Chronic orofacial pain (COFP) disorders are prevalent and debilitating pain conditions affecting the head, neck and face areas. Overall, these findings provide evidence of brain abnormalities in pain-related regions, namely the thalamus and insula, across different COFP disorders.”
This is of particular interest once you realize how important the role of the thalamus is in chronic pain that originates in the brain itself as opposed to injured tissues, and is otherwise known as CENTRAL SENSITIZATION. Without going into detail, suffice it to say there are numerous studies linking CS to whiplash.
We’ve briefly discussed cervicogenic headache, but what about cervicogenic dizziness? A study from last month’s issue of the European Archives of Otorhinolaryngology (Approach to Cervicogenic Dizziness: A Comprehensive Review of its Etiopathology and Management) stated that, “Though there is abundant literature on cervicogenic dizziness with at least half a dozen of review articles, the condition remains to be enigmatic for clinicians dealing with the dizzy patients.” Would it make sense that if the source of the dizziness is the same or at least similar to the source of cervicogenic headaches, you might want to try treating it the same way? Although this and similar situations might call for the expertise of a FUNCTIONAL NEUROLOGIST, this is typically a great starting point, with the potential to help many in this category.
Because MIGRAINE HEADACHES and TEMPOROMANDIBULAR DISORDERS are so frequently seen after whiplash as well, the importance of a study titled Muscle Tenderness Score in Temporomandibular Disorders Patients: A Case-Control Study from this month’s issue of the Journal of Oral Rehabilitation cannot be overlooked. Whiplash patients (again, mostly women) showed jaw muscle tenderness and trigger points that were associated with, “female sex, whiplash history, parafunction [poor or abnormal function], co-morbid pains such as headaches and body pain, pain intensity, onset, frequency, and duration.” And as for migraines, a study from the September issue of Musculoskeletal Science and Practice (Cervical Musculoskeletal Dysfunction in Headache: How Should it be Defined?) debated whether neck pain is the result of headache, or headache is the result of neck pain. I would argue that the point is moot because the nerve pathways are largely a two way street, with one almost always being able to cause the other (notice below that this study — by a team of Australian researchers — gave us an amazing definition of ‘subluxation,’ actually mentioning the difference between SEGMENTAL AND SECTIONAL NECK MOTION).
“Neck pain commonly accompanies migraine and tension-type headache. Reliance on pain sensitivity or the presence of neck tenderness/trigger points as measures be discarded, as they are not uniquely tied to a musculoskeletal disorder. Instead, place reliance on tests of musculoskeletal (dys)function. A typical presentation includes at a fundamental level, interrelated changes in cervical movement, segmental joint and muscle function.”
Another study, this one from Acta Neurologica Belgica (Neck Pain: Is it Part of a Migraine Attack or a Trigger Before a Migraine Attack?) pushed this issue even further when it stated, “Neck pain may actually be the most common migraine symptom despite the fact that it is rarely listed among usual symptoms such as nausea and light sensitivity.” The authors, however, could not answer the question posited in the study’s title because 90% of the participants said that they started at the same time. Before we head to the next section (treatment), I need to briefly mention a study on neck pain in athletes.
Lat month, the Asian Spine Journal published a systematic review of the scientific literature titled Prevalence of Neck Pain among Athletes that encompassed numerous studies on the subject. “Neck pain was shown to be prevalent in athletes, with a 1-week prevalence ranging from 8% to 45%, a 1-year prevalence ranging from 38% to 73%, and a lifetime prevalence of about 48%. The prevalence of neck pain in athletes is high.” Although studies on prevalence of neck pain in the general population are all over the place, the statistics for athletes appear to be at least 10-20 percentage points higher.
RESEARCH CONCERNING NECK,
WHIPLASH, AND HEADACHE TREATMENT

What are some of the things we can say for sure about treatment of whiplash injuries? Although treatment theories abound, the rock-solid foundation of whiplash rehabilitation is that it’s critical to restore normal neck function / range of motion as quick as possible because research has shown that after ninety days, the odds of dramatic improvement plummet.
A few months ago the journal Scientific Reports (Neck-Specific Exercise May Reduce Radiating Pain and Signs of Neurological Deficits in Chronic Whiplash) provided some sobering figures before telling us how bad nerve-related whiplash problems can be. “Up to 90% of people with neurological deficits following a whiplash injury do not recover and cervical muscle dysfunction is common.” They concluded that neck-specific exercises are helpful in the recovery. Another study, this on from the journal Musculoskeletal Science and Practice (Relationship Between Neck Motion and Self-Reported Pain in Patients with Whiplash Associated Disorders During the Acute Phase), found that the level of neck pain a whiplash sufferer is dealing with can be mapped via “kinematic parameters of neck mobility tests, ranges of motion, motion velocities, repeatability and harmonicity of movements [proprioception].“
This summer the European Journal of Pain published a study titled Seeing the Site of Treatment Improves Habitual Pain but not Cervical Joint Position Sense Immediately after Manual Therapy in Chronic Neck Pain Patients, which concluded that it may actually be helpful for manual therapists to have a way of allowing their patient to visually see what they are doing. “Real-time visual feedback reduces habitual [chronic] pain immediately after the intervention.” Just remember that this will tend to throw some people into a sympathetic response that we discussed earlier. In a study titled Comparison of Ozone and Lidocaine Injection Efficacy vs Dry Needling in Myofascial Pain Syndrome Patients, researchers did exactly what the title suggests; observing 72 patients to determine that all injections were about the same efficacy — a characteristic of DRY NEEDLING that has proven that the action of the needle itself is far more important than the substance being injected through the needle. “No remarkable preference between them.“
As far a cupping and acupressure go, there were studies on both. After looking at 18 studies on cupping, a group of nine Korean researchers publishing in this month’s issue of BMJ Open (Is Cupping Therapy Effective in Patients with Neck Pain? A Systematic Review and Meta-Analysis) concluded that
“Neck pain is a significant condition that is second only to depression as a cause of years lived with disability worldwide. Cupping was found to reduce neck pain in patients compared with no intervention or active control groups, or as an add-on treatment. Depending on the type of control group, cupping was also associated with significant improvement in terms of function and quality of life…” In another Korean study, this one from the September issue of Integrative Medicine Research (Clinical Effects of Acupressure on Neck Pain Syndrome (nakchim): A Systematic Review), the authors looked at the effects of acupressure on a type of non-traumatic neck pain syndrome not associated with trauma they refer to as nakchim. Their conclusions? After looking at 15 studies of over 1,000 subjects, the authors determined that “acupressure may be effective on nakchim.”
What about chiropractic care? The West Coast’s giant managed care organization (Kaiser Permanente), along with several major universities, published a study in a recent issue of the Journal of General Internal Medicine (Comparative Effectiveness of Usual Care With or Without Chiropractic Care in Patients with Recurrent Musculoskeletal Back and Neck Pain). Not surprisingly, the care for the chiropractic group cost about half that of usual medical care. “As clinical outcomes were similar, and the provision of chiropractic care did not increase costs, making chiropractic services available provided an additional viable option for patients who prefer this type of care, at no additional expense.” It costs less, but was it as effective?
After saying that “Neck pain is prevalent, costly and disabling,” a team of European researchers from several universities and facilities concluded that,
“mobilisation participants reported significantly better global perceived effect and improvements in movement associated pain. Mobilisations produced a significant increase in ROM in side flexion and rotation when compared with placebo…. 29-47% of all movement associated pains were resolved following mobilisations and 11-27% following placebo. Patients in both groups showed a significant increase in movement velocity…. Cervical mobilisations are effective in improving movement-associated pain, increasing ROM and velocity, and patient perceived improvement when applied to patients with neck pain… Their use should be advocated.“
In another study — A collaboration between RAND and the UCLA School of Medicine (Group and Individual-level Change on Health-related Quality of Life in Chiropractic Patients with Chronic Low Back or Neck Pain) that was published in last month’s copy of Spine — the idea of trying to determine responders from non-responders was put forth. After doing interviews and evaluations (“physical function, pain, fatigue, sleep disturbance, social health, emotional distress and physical and mental health summary scores“) with over 2,000 patients at 125 chiropractic clinics throughout the United Stated, the authors concluded that….
“Chiropractic care was associated with significant group-level improvement in health-related quality of life over time, especially in pain. But only a minority of the individuals in the sample got significantly better (“responders”). This study suggests some benefits of chiropractic on functioning and well-being of patients with low back pain or neck pain.”
Let’s talk about these “responders” for a moment and try and flesh out why someone might fall into this category, while the next person, with a seemingly identical situation and symptoms, might wind up labeled a non-responder. First, let me say that 30% of those surveyed showed significant improvement in their “Mental Health Summary Score” — a big deal for a class of patients, that as I have shown you, struggle with the twin terrors of chronic pain and mental health issues (I have always suggested that chronic pain tends to lead to depression). As far as the “significant,” but far from earth-shattering results of chiropractic adjustments on these sorts of patients, I have two thoughts on this, inflammation and scar tissue.
I have heard old timers (chiros) say that getting the average patient better used to be easier (HERE). Much of this has to do with the fact that today’s average patient is inflamed beyond belief; here is a simple SELF TEST. Inflammation is not only at the root of virtually all our most common health-related problems (including most we would rather blame on “BAD GENES“), as I showed you earlier, it always leads to the fibrosis (I call it scar tissue) that is arguably the world’s number one cause of death (HERE). When this microscopic, fibrotic, adhesed, scarring builds up in compromised connective tissues, the result is a “TETHERING EFFECT” that prevents normal ranges of motion, which thanks to loss of proprioception (see earlier link) perpetuates the cycle of degeneration (calcification, bone spurs, thinning joints and discs).
When it comes to chronic neck pain (as well as most other problems not related to a herniated disc), I run my clinic in much different fashion than the average chiropractor. Because of this different approach, I tell patients that they will know after a treatment whether or not I can help them. There is no trying to up-sell you on drawn out or expensive care plans. It’s simple; you come in, I talk with you and examine you. If I think there is a good chance of being able to help you, we go from my office to a treatment room and I do my thing. While one treatment may certainly not be enough to do everything that needs to be done, THIS POST (not to mention my hundreds of TESTIMONIALS) shows what makes us different. And if you are interested in taking that extra step to deal with the chronic inflammation that’s wreaking havoc on your life, you can READ THIS FREE POST in your spare time and see what you think.
My goal is to remove as many roadblocks to the healing process as possible, while empowering you to step up and do those things that unfortunately, no one else — your doctors included — can do for you. If you appreciate our site and would like to see more people reached with life-changing information, be sure to like, share or follow on FACEBOOK since it’s one of the easiest possible ways to reach the people you love and care about most!
