SHOULDER IMPINGEMENT SYMPTOMS
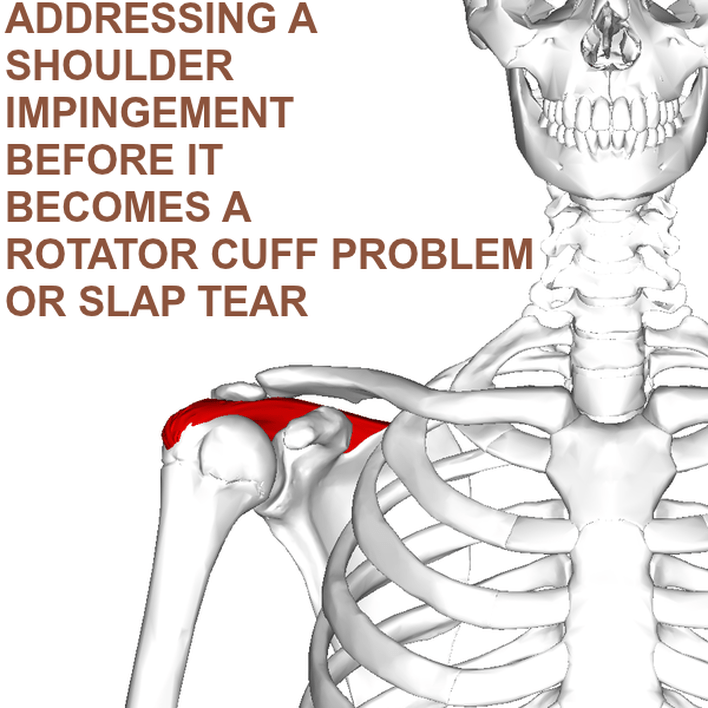
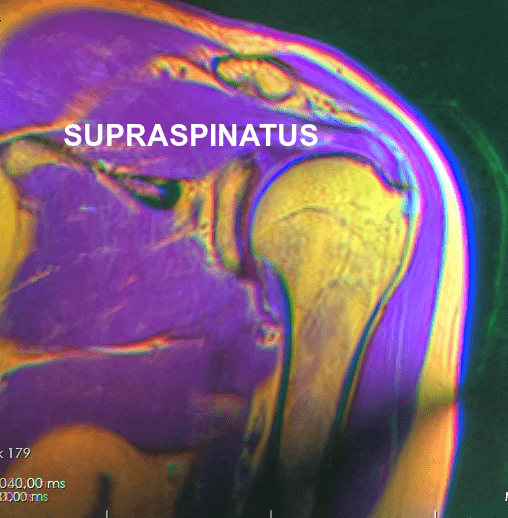
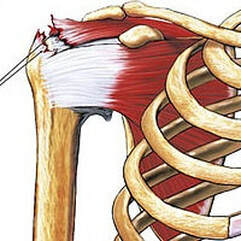
Anatomography “Neer first introduced the concept of rotator cuff impingement in 1972. He believed the etiology to be impingement of the rotator cuff tendons under the acromion and the rigid coracoacromial arch [see pic above], eventually leading to degeneration and tearing of the rotator cuff tendon, which are more common in older populations. The increased forces and repetitive overhead motions can cause attritional changes in the distal part of the supraspinatus tendon, which is most at risk due to its poor blood supply.”Cherry-picked from a 2004 issue of Physical Medicine and Rehabilitation Clinics of North America (Shoulder Impingement Syndrome)
“Shoulder pain is the third most common musculoskeletal complaint in orthopedic practice, and impingement syndrome is one of the more common underlying diagnoses. Shoulder impingement is a clinical syndrome in which soft tissues become painfully entrapped in the area of the shoulder joint.” From the November 2017 issue of Deutsches Arzteblatt International (Impingement Syndrome of the Shoulder) As you can see from the quote above, shoulder problems of all kinds are common (HERE). Dog common. There are DISLOCATIONS & SEPARATIONS. There are numerous TENDINOPATHIES, including that of the ROTATOR CUFF and BICEPS TENDON. And there is the dreaded SLAP lesion — the torn labrum (Superior Labrum, Anterior to Posterior). Remember this, however. It was the distinguished orthopedic sports surgeon, DR. JAMES ANDREWS, who famously said, “if you need an excuse to do shoulder surgery, just do an MRI“. Which brings me to shoulder impingement.
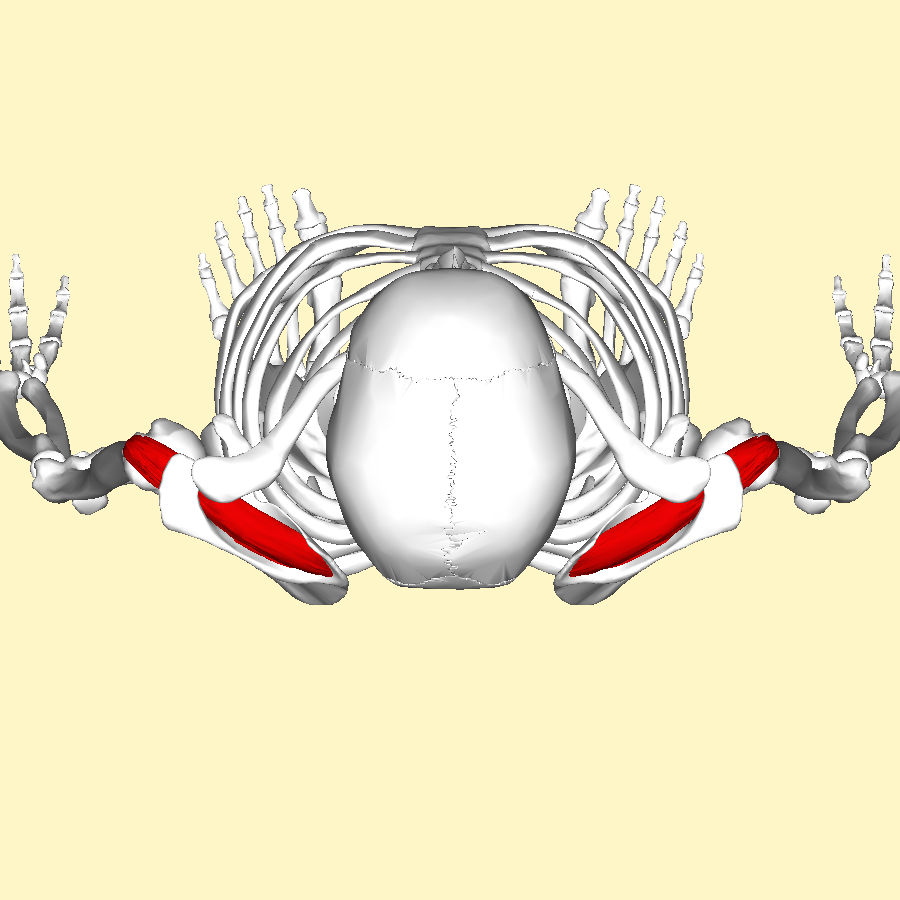
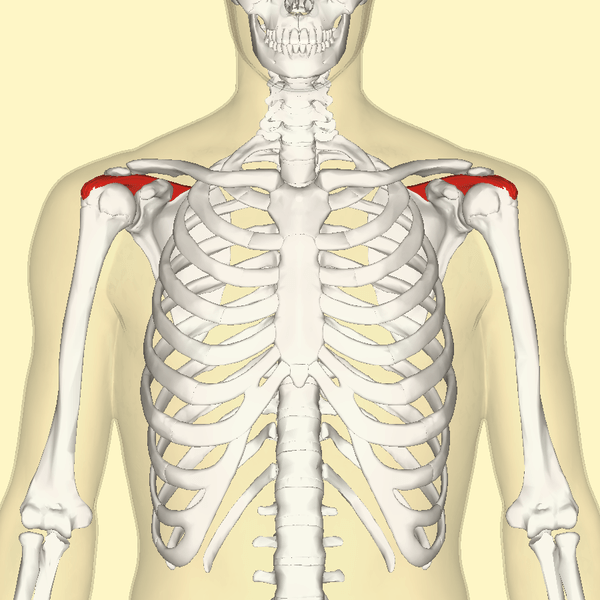
The most common muscle of the rotator cuff group-of-four to be injured — the supraspinatus, seen in red in the pics — takes a path that runs underneath the AC joint (the acromio-clavicular joint, where the collar bone attaches to the knob of bone coming over the top of the shoulder blade), attaching it’s distal or ‘distant’ tendon (the one with the poor blood supply mentioned above) to the upper outside part of the shoulder (again, see pictures). This is why most cases of shoulder impingement hurt at — you guessed it — the upper, outer part of the shoulder; frequently running to just above the elbow (BUT DO NOT CONFUSE THIS WITH CERVICAL RADICOLOPATHY). All of this begs the question, how common are shoulder impingements?
Largely a function of UPPER-CROSSED SYNDROME (a combination of POOR POSTURE and upper extremity muscle imbalance) and CHRONIC OVERUSE (work, sports, swimming, lifting weights, etc, etc) — particularly in those who do lots of overhead activities — shoulder impingement (often referred to as SAPS — Sub-Acromial Pain Syndrome, or SIS — Subacromial Impingement Syndrome) is the number one reason reason for shoulder pain, accounting for as much as 65% of it according to some studies, with those numbers getting larger as the birthdays pile up (the most common decade of life for this problem is the fifties). All great to know, but what is a shoulder impingement?
The first thing to remember is that you will often see shoulder impingements spoken of as either primary or secondary. The primary impingement occurs because of a compression by bone spurs at the AC joint or a congenital anomaly of the bony structure of the shoulder. Primary impingements are not as common and not really what we are talking about today (see first embedded YouTube video below). The subject of today’s post is the secondary shoulder impingement.
If you simply look at the pictures (especially the overhead view below left) you will notice that the SUPRASPINATUS runs underneath the AC joint. Although INFLAMMATION leads to swelling, swelling is not the only reason for impingement; not by a long shot. Besides what we’ve already mentioned, the biggest factors in developing shoulder impingement syndrome include things like ARTHRITIS, THICKENING of the connective tissues in the area (including the FASCIA), which leads to tightness, SUBACROMIAL BURSITIS. However, one could argue that the number one reason for shoulder impingement is POOR BIOMECHANICS of the shoulder blade (aka scapular dyskinesis), which is fantastic because there are relatively simple ways to address it, which we’ll get to shortly. How can you tell you may have a shoulder impingement?
Although you could opt for an MRI, just remember that significant numbers of musculoskeletal pathologies do not image well on MRI, with an equal number of people who have no pain showing, as Dr. Andrews insinuated earlier, an array of abnormalities (HERE), making imaging far from a sure thing as far as determining the source of one’s shoulder pain is concerned. The best bet may be to look for the obvious by answering some simple questions.
- Do you regularly or have you ever engaged in significant amounts of repetitive shoulder motions?
- Are you currently or have you been either sedentary or abusive as far as your shoulders are concerned?
- Do you currently or have you spent lots of time working at a computer, a desk job, or factory job that requires leaning forward / looking down?
- Do you have “THE POSTURE OF AGE” (which is also the posture of chronic illness and chronic pain)?
- Do certain movements cause pain; particularly overhead reaching, scratching your back, grabbing your seat belt, etc?
- Do you feel weakness when doing certain shoulder movements or activities?
- Have you lost range of motion in your affected shoulder compared to your non-affected shoulder?
- Do you fear the pain enough that you have altered or avoid normal activities?
- Do you have the “PAINFUL ARC“?
- Do you have a positive HAWKINS-KENNEDY TEST or NEER TEST?
- Are your shoulders internally rotated? In other words, do you have a POSITIVE PENCIL TEST? (stand in front of a mirror with a pencil in your hand or with a fist, thumbs out. If the pencils / thumbs are pointed inward, your shoulders are internally rotated.)
- Does sleeping on the affected side cause discomfort?
It’s not rocket science. The more of these questions you answered yes to, the greater the chance you have a shoulder impingement. Follow along as we dig a bit deeper.
SHOULDER IMPINGEMENT SYNDROME
WHAT DOES THE PEER-REVIEWED RESEARCH HAVE TO SAY?
Although some of you may want to skip this section and head directly to the last section on solving the problem, many of you — particularly those of you struggling with shoulder impingement and who want to continue with the repetitive activities / sports that got you here in the first place — may actually need to take notes. Why is it important to deal with this problem early, hopefully before you ever have symptoms, or at least before you become functionally limited? Realize that many shoulder problems that end up bad enough to lead you to a surgeon’s office could have been headed off at the pass with a little bit of specialized knowledge that was put to good use.
For instance, one of last year’s issues of Knee Surgery, Sports Traumatology, Arthroscopy (More Histologic and Ultrastructural Degenerative Signs in the Subscapularis Tendon and the Joint Capsule in Male Patients with Shoulder Impingement) revealed that patients with shoulder impingement have more degenerative changes than patients who have shoulder degeneration due to trauma. While there are likely many reasons for this, this article spoke of two factors that I beat like a drum on my site and in my clinic; factors that are intimately related to each other — inflammation and tissue thickening (links provided in previous section). “With time, its thickening causes conflict and pain between the acromion and the rotator cuff.” Never forget that inflammation always leads to fibrosis, which is the medical word for tissue adhesion and thickening, which functionally is scar tissue (HERE).
Be aware that there are several kinds and causes of shoulder impingement, and that this results in a number of different (and sometimes confusing) manifestations and symptoms. Last February’s issue of International Orthopedics (Redefining Anterior Shoulder Impingement: A Literature Review) stated this very thing. “There are many different subtypes of anterior impingements in the shoulder, and awareness of their existence is critical as they vary in their nature and treatment.” According to a 2003 issue of The Journal of Bone and Joint Surgery (Shoulder Impingement Presenting as Neck Pain) one of these is NECK PAIN. “In selected patients, chronic neck pain may be caused by shoulder impingement.” It’s a phenomenon that’s far more common than these authors realized. And as you’ll see in a moment, the reverse is true as well —- chronic neck dysfunctions can lead to shoulder impingements.
That’s right folks; posture is a big deal when it comes to shoulder impingements. For verification simply look at this Japanese study of over 2,100 individuals older than 40 by 9 authors from several different universities in Japan (Association Between Kyphosis and Subacromial Impingement Syndrome: LOHAS Study) and published in the December 2014 issue of the Journal of Shoulder and Elbow Surgery.
“Kyphosis [a forward rounded upper back and shoulders] is a cause of scapular dyskinesis, which can induce various shoulder disorders, including shoulder impingement. Age- and gender-adjusted logistic regression analysis demonstrated significant association between subacromial impingement syndrome (SIS) and the wall-occiput test for thoracic kyphosis. There was also significant association between subacromial impingement syndrome and reduction in shoulder elevation (RSE). RSE plays a key role in the development of SIS, and thoracic kyphosis might influence the development of SIS indirectly by reducing shoulder elevation induced by the restriction of the thoracic spine extension and scapular dyskinesis.”
Although we will deal with scapular issues in the next section, let’s move on to something near and dear to my heart; proprioception. PROPRIOCEPTION is a critical function of connective tissues, particularly the fascia, and when you don’t have it, bad things happen, including increased amounts of bony and soft-tissue degeneration (HERE). A team of eight researchers from Turkey’s Dokuz Eylul University published a study in a 2017 issue of the Journal of Back and Musculoskeletal Rehabilitation (Shoulder Proprioception in Patients with Subacromial Impingement Syndrome) that came to some interesting conclusions regarding proprioception and kinesthesia (the body’s ability to sense where it’s at in space via sensory organs in joints and soft tissues called proprioceptors / mechanoreceptors) in 61 patients, average age almost 50.
“When involved shoulders of the patient group were compared to the control group, kinesthesia, active and passive joint position senses were significantly impaired in involved shoulders in patient group at all angles. When uninvolved shoulders of the patient group were compared to the control group, kinesthesia at 10° was significantly impaired. This study showed that shoulder proprioception was impaired in patients with SIS. This proprioceptive impairment was found not only in involved shoulders but also in uninvolved shoulders in patients with SIS.”
Did you catch that? There is neurological crossover taking place. In the same way that mirror-image therapy can aid stroke victims via the crossover phenomenon; in this study, affecting one shoulder adversely automatically adversely affected the other! In another study, this one from a 2010 issue of the British Journal of Medicine (Posterior Superior Internal Impingement: An Evidence-Based Review) both “contracture of the posterior [shoulder] capsule and reduced humeral retroversion” were put forth as causes of shoulder impingement. What does this mean and why are these two entities so intimately related to each other?
First, the shoulder capsule is the fluid-filled ligamentous capsule that surrounds the shoulder joint, lubricating it and allowing it to glide freely. As you would expect, it should be supple and have some play in it (key word, some). As elite athletic trainer, Eric Cressey, said in his 2010 article, Why President Obama Throws Like a Girl, “For the lay population out there, think of retroversion as a bony positioning that allows for more shoulder external rotation. As we age, we actually gradually lose retroversion.” How closely linked are these two entities, shoulder retroversion and tightness / thickening of the back of the shoulder capsule?
The July 2012 issue of the Journal of Shoulder and Elbow Surgery (Humeral Retroversion and its Association with Posterior Capsule Thickness in Collegiate Baseball Players) provides an idea by concluding “A significant positive correlation was also found between humeral retroversion and posterior capsule tightness. This study suggests that humeral retroversion may be contributing to the negative adaptation of posterior capsule tightness.” It’s only common sense, as tissues “thicken” (and subsequently tighten) due to mechanical stresses placed upon them — DAVIS’ LAW. This is what TISSUE DEFORMATION (or HERE) is all about, and can either work for or against you, depending on the circumstances and context.
At the 55th Annual Meeting of the Orthopaedic Research Society, a group of biomechanical scientists presented a paper (Posterior Capsule Tightness Affects the Subacromial Contact Behavior during Shoulder Motion) saying, “Based on these findings it is speculated that higher contact pressure could be generated in the tissues between the coracoacromial arch and humeral head by posterior capsule tightness and injure them during shoulder flexion.” For the record, shoulder flexion is what occurs as one is raising their arm out in front of them.
Another study, this one from a 2017 issue of the Journal of Back and Musculoskeletal Rehabilitation (The Presence and Influence of Posterior Capsule Tightness on Different Shoulder Problems) looked at 125 patients, comparing posterior capsule tightness in shoulder pain patients to patients without pain. “It was found that the affected side of the posterior capsules of the patients with subacromial impingement syndrome, partial rotator cuff tear and frozen shoulder was stiffer than their healthy side. All range of motion of the shoulder including the hand-behind-the-back test and the posterior capsule tightness of the affected side are found to be correlated.” The authors of a 2012 study in Shoulder Elbow put it this way. “Clinically, [posterior capsule] contracture manifests as a reduction in glenohumeral internal rotation and/or cross body adduction range of motion. Stretching and manual techniques are used to improve range of motion and often decrease symptoms in painful shoulders.” Hang on because we will get to these stretches in a moment.
Posterior humeral glide is the ability of the head of the humerus (the top arm bone) to move backwards. Although there are several ways to asses this, one is to stand behind someone (I like to do it while they are seated, although I just as frequently do it while they are standing), have them put their arm out in front of them and flex their arm all the way (like a maxed out bicep curl) so that they are facing forward with their elbow sticking straight out in front of them. I will then put my chest against the opposite side of their back, reach around them and grab their affected elbow with both hands and gently pull straight back to my body to check for lack of glide. A tight posterior (back) shoulder capsule is one of several things that can hinder this motion. Shoulder biomechanics is a complex subject, but suffice it to say that if the back part of the shoulder is tight, it can cause or at least contribute to subacromial impingement syndrome.
Next we move on to “Scapular Dyskinesis,” which is a fancy way of talking about abnormally functioning shoulder blades. Because there is a relationship between scapular winging and subacromial pain, let’s dig a little bit deeper. A 1984 issue of Clinical Orthopedics and Related Research (The Winged Scapula) said this. “Winging of the scapula is a surprisingly common physical sign, but because it is often asymptomatic it receives little attention. However, symptoms of pain, weakness, or cosmetic deformity may demand attention.” And while there are numerous causes of scapular winging, the most common is muscle imbalances — particularly true in cases of minor or moderate winging. Severe winging is more likely to be a NERVE ENTRAPMENT. The title of a study from the October 2015 issue of Revista Brazilian Orthopedics — “Syndrome of Fascial Incarceration of the Long Thoracic Nerve: Winged Scapula” — helps explain why I frequently use tissue remodeling techniques to address this aspect of the problem.
One of the best articles on the web concerning winged scapula is by Physical Therapist, Mark Wong (How to Fix a Winged Scapula), who lists “pec minor tightness/over-activity” first under the header, What Causes a Winged Scapula? This is doubly interesting because I have written about the absurd prevalence of LEVATOR TRIGGER POINTS (they may be more common than all other TP’s combined), which just happen to be intimately related to pec minor trigger points (see link). If you have a winged scapula, be sure to read MARK’S ARTICLE over at Posture Direct! As you might imagine, this shows that thickening and tightness in the front of the shoulder has the propensity to contribute to shoulder impingement as well. As you should be starting to see, it’s all about balance. In the famous words of Master Po, ‘Learn balance young grasshopper.’
A Y2K University of Minnesota study that was published in the journal, Physical Therapy, tells you everything you need to know via its title; Alterations in Shoulder Kinematics and Associated Muscle Activity in People with Symptoms of Shoulder Impingement. The authors of a Belgian study from 2011 (Scapular Positioning and Movement in Unimpaired Shoulders, Shoulder Impingement Syndrome, and Glenohumeral Instability) reviewed 30 scientific papers on the subject, concluding that although there was a lack of consensus as to the exact cause, there was overwhelming agreement that scapular winging and dyskenesis are strongly related to shoulder impingements. A study from a 2014 issue of the Journal of Electomyography and Kinesiology showed something similar……
“Patients with subacromial impingement syndrome (SIS) and glenohumeral instability display numerous variations in scapulothoracic muscle activity compared to healthy controls. In the SIS-group, the lower trapezius muscle and serratus anterior muscle activity is decreased. In addition, the upper trapezius muscle activity is increased among the SIS patients…”
Now let’s take a moment to briefly discuss the relationship between FORWARD HEAD POSTURE and shoulder impingment in the peer-reviewed literature. Listen to what renowned bodyworker, Erik Dalton, says of this relationship in relationship to upper crossed syndrome, which I mentioned earlier. From his article titled Janda Upper Crossed – Neck, Shoulder and Rotator Cuff Pain……
“The problem with a rounded shoulder posture is that the mechanical axis of rotation of the glenoid fossa becomes altered. The humerus now requires additional stabilization from muscles that are typically at rest, such as the upper trapezius, levator scapulae, pectoralis minor, subscapularis, supraspinatus muscles. Postural overdevelopment of these muscles creates a deltoid shear (crossing of rotator cuff under AC joint), leading to shoulder impingement, tendinitis and bursitis syndromes.”
Rather than going over a lot of research here, I’ll leave you with a couple of study titles as well as my post on extension therapy (link provided in next section). Some of these studies include 2005’s Subacromial Impingement Syndrome: The Effect of Changing Posture on Shoulder Range of Movement from JOSPT; 2016’s Cervical Contribution to Functional Shoulder Impingement… from IJSPT; and 2017’s Postural Alterations in Patients with Subacromial Impingement Syndromes from the same journal. Although I said it before, I’ll say it again; when it comes to shoulder impingements, posture really does matter!
WHAT YOU CAN DO ABOUT
SHOULDER IMPINGEMENT SYNDROME
“Rotator cuff disorders are considered to be among the most common causes of shoulder pain and disability encountered in both primary and secondary care. The general pathology of subacromial impingment generally relates to a chronic repetitive process in which the conjoint tendon of the rotator cuff undergoes repetitive compression and micro trauma as it passes under the coracoacromial arch. Studies show that conservative management of shoulder impingement syndrome resolves the problem in 70-90% of patients.”From the September 2013 issue of the Open Orthopedics Journal (The Painful Shoulder: Shoulder Impingement Syndrome)
“Operative management is variable depending on the exact pathology, but largely consists of rotator cuff debridement. Outcomes of operative treatment have been mixed, therefore intense non-operative treatment should remain the focus of treatment.” Taken from the December 2016 issue of the World Journal of Orthopedics (Evaluation and Treatment of Internal Impingement of the Shoulder in Overhead Athletes)
“Nonoperative rehabilitation programs for impingement syndrome have been reported in the literature, consisting of rest, rotator cuff and scapula strengthening, and manual techniques, with good outcomes. Conroy and Hayes demonstrated that after 3 weeks of treatment, participants receiving both exercises and manual therapy had less pain compared with participants who performed exercises only. Bang and Deyle reported on the outcomes of patients who performed strengthening and stretching compared with those who performed the same exercise program and received manual therapy to the cervical and thoracic spine and shoulder joint after 3–4 weeks of treatment. Subjects who received manual therapy plus stretches reported less pain and improved function and strength compared with the stretch-only group.” From the February 2014 issue of the Open Access Journal of Sports Medicine (Optimal Management of Shoulder Impingement Syndrome) If you’ve made it this far, you should have realized that firstly, the most common presentation of shoulder problems to healthcare professionals is related to subacromial shoulder impingement; and secondly, that the medical consensus is to get serious about non-surgical, conservative methods first, because they happen to be what actually work best. Shoulder surgery is not necessarily the end of the world, but the harsh reality is that recovery is always long and painful — a bad combination for active people or individuals who can’t miss work or have physical jobs / careers.
If you go to the local medical clinic, the first thing that will probably happen is some kind of imaging. And while the right x-ray view will show primary shoulder impingement in the form of bony spurring, it won’t do anything to show you the secondary causes — causes which are arguably far more common (see first video below). As for other imaging, I’ve already mentioned MRI. Be aware, however, that diagnostic ultrasound is gaining ground in this arena (HERE is an example with the thoracolumbar fascia). Just realize that with imaging, you’ll probably end up forking out a lot of money, while not necessarily achieving that desperately sought after “aha moment” (TELL ME AGAIN WHY YOU WANT AN MRI?). What’s next?
In the progression of things, you will almost assuredly be prescribed some goodies from the “BIG FIVE” class of drugs — particularly NSAIDS and CORTICOSTEROID INJECTIONS. And while you will never hear me say that these drugs don’t, at least on some level, do what they are supposed to do (diminish inflammation), be warned that they come with rather high SIDE-EFFECT PROFILES, that exponentially increase with increased exposure.
Next comes the recommendation for therapy. This is a good option, and depending on your level of personal motivation or how much money you are willing to spend out-of-pocket to see a therapist multiple times a week, there are at least a couple of options available here. You could visit a knowledgeable therapist or sports chiro, get evaluated, and go through their recommended protocol in their clinic. Or you could have them show you what to do and do it yourself on your own. Or you could simply bypass all that and try to do it yourself from the get-go. Like I said, it all depends on your situation and what you are willing (or able) to do on your own. What would my PLAN-OF-ACTION look like if I were in this boat?
- GET SERIOUS ABOUT RESOLVING INFLAMMATION: Remember that there are numerous ways to successfully address inflammation without resorting to DANGEROUS DRUGS. I’ve provided my patients and readers a generic protocol for doing so HERE. Nope; it’s not a panacea, but if you grasp the fact that — as I stated earlier — inflammation always causes fibrotic change that I refer to in my clinic as scar tissue (HERE), it only makes sense that getting serious about things that reduce inflammation could prove useful (yep, DIET is undoubtedly number one in this bullet point!).
- USE A LASER: I’ve written about LOW LEVEL LASER THERAPY in numerous posts and use it in my clinic. Laser works by boosting MITOCHONDRIAL FUNCTION, which allows for significantly more healing in the treated area. Class III lasers can often be purchased by the public for “animal” use, but depending on how deep the impingement is, may not penetrate deeply enough, requiring a Class IIIB or Class IV. Although far from a cure-all, when laser works it’s amazing.
- CHIROPRACTIC AND PHYSICAL / MANUAL THERAPIES: While chiropractic adjustments are wonderful for a variety of issues (including most shoulder problems), what’s not wonderful are treatment plans that never seem to end (HERE). As I shared earlier, finding a knowledgeable professional to help get you started may be just what you need. Also, for many of you with shoulder, neck, or upper back problems, TISSUE REMODELING may be an excellent option (HERE). A study from a 2013 issue of Clinical Rheumatology (Scapular-Focused Treatment in Patients with Shoulder Impingement Syndrome: A Randomized Clinical Trial) concluded that, “A large clinically important treatment effect in favor of scapular motor control training was found in self-reported disability, and a moderate to large clinically important improvement in pain during the Neer test, Hawkins test, and empty can test. In addition, the experimental group demonstrated a moderate improvement in self-experienced pain at rest, whereas the control group did not change. The effects were maintained at three months follow-up.“
- EXERCISES, STRETCHES, AND POSTURE TRAINING: Just remember that for many of you, it was repetitively beating your body with exercise (poor mechanics and muscle imbalance) that put you here in the first place. This means that you’ll probably have to lay off your regular gym / pool / tennis court activities for awhile to focus on exercises that you might not exactly love. While there are many postural aids and specific strategies available, they generically encompass some of what’s found in THIS POST on getting your body out of flexion and into extension. Beyond that, there are a host of great websites and videos available to help you. A couple good ones can be found HERE and HERE.
Youtube is loaded with amazing information and DIY / self-help hints and pointers, in many cases by people with a great deal of expertise in their area. Be aware, however, that it is also loaded with a lot of info that’s not so amazing. Although there are undoubtedly other videos that many would argue are much better, I threw these on because they provide a taste of what’s out there and are certainly good enough to get you started in creating your plan. If you come across something amazing, drop me a link.
One warning. I always suggest adding one exercise at a time simply because if a particular exercise happens to aggravate your condition, you will immediately know the culprit. Add numerous exercises at one time, and if you get worse it’s tough to know what the aggravating factor is.
To start with, we have Bob and Brad reviewing Orthopedic Surgeon, DR. JOHN KIRSCH’S book, Shoulder Pain? The Solution & Prevention. I own this book and all I can say is that not only is it the bomb for most shoulder problems (unfortunately, probably not SLAP tears), but it’s so stupidly simple that anyone, and I do mean anyone can follow his program. If fact, this ten dollar paperback could have been one page long if it weren’t for the scientific explanation (including pictures) of what’s taking place physiologically / anatomically in the shoulders when you hang. His protocol is based on WOLFF’S LAW, and following these ridiculously simple principles may void your need for looking at any of the other videos below.
Watch as these same two physical therapists demonstrate four different orthopedic tests used to determine the likelihood that your shoulder problem is an impingement or something else (HERE).
“Instead of the roof of the subacromial space (the AC joint) coming down and pressing on the structures, I really think that most of it is that the floor (the glenoid ball of the shoulder) is coming up.” This means that inferior glide of the humeral head is a must!
Wow; that was somewhat overwhelming! But if you eat it the same way you eat the proverbial elephant, one bite at a time, it becomes manageable. I recommend you create your own written plan for getting out of shoulder pain, starting by going back, taking notes, and figuring out how you want to attack this beast. And if you appreciate the time, energy, and effort that goes into my site — especially on my BIRTHDAY for Pete’s sake — make sure to spread the wealth by liking, sharing or following on FACEBOOK, as it’s still an effective way to reach the people you love and care about most.
