STRUGGLING WITH LOW BACK PAIN? A NEW STUDY SHEDS LIGHT ON CAUSES AND SOLUTIONS (THORACOLUMBAR FASCIA)
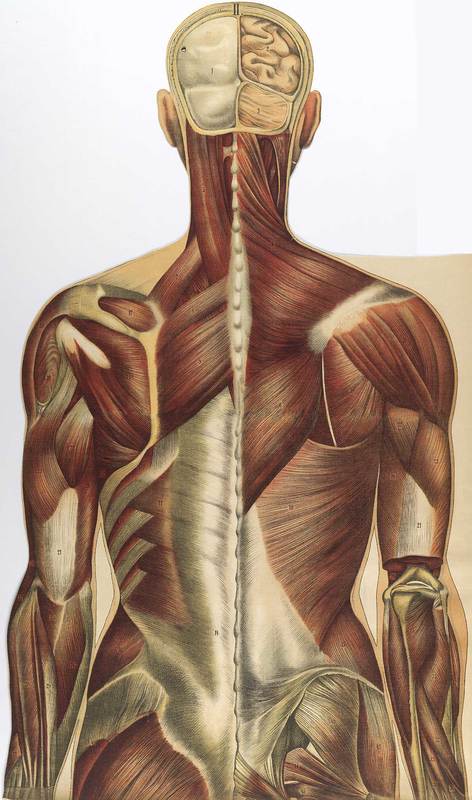

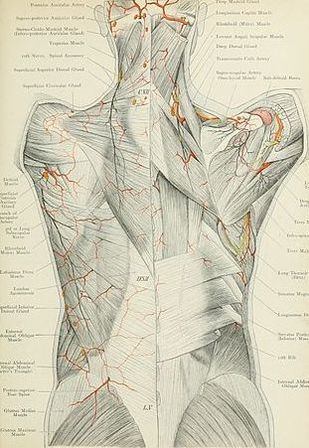
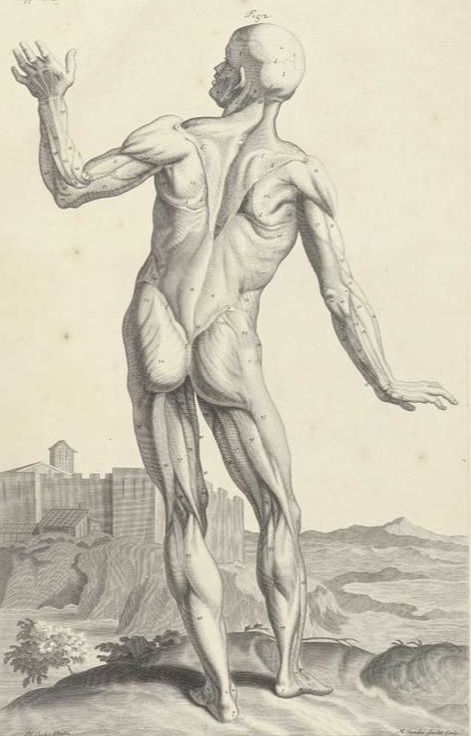
Today I am going to review a brand new, well-bibbed study (37 sources) from the medical journal BioMed Research International titled The Lumbodorsal Fascia as a Potential Source of Low Back Pain: A Narrative Review. FYI, when the authors of this study talk about the “Lumbodorsal Fascia,” what they are really talking about is more commonly known as the THORACOLUMBAR FASCIA as seen in the picture above as well as the provided link. Before we tackle today’s study however, listen to what Dr. Serge Gracovetsky of Concordia University in Montreal said nearly a decade ago in a study published in the Journal of Bodywork and Movement Therapies.
“The role of the lumbodorsal fascia is generally neglected in spine biomechanics. Yet it is perhaps the most important structure insuring the integrity of the spinal machinery. The viscoelastic property of its collagen has a direct impact on the way the muscles are used and forces are channeled from the ground to the upper extremities. As a controller of the forces distribution between muscles and fascia, lordosis is the prime candidate for rehabilitation in the event of injury.”
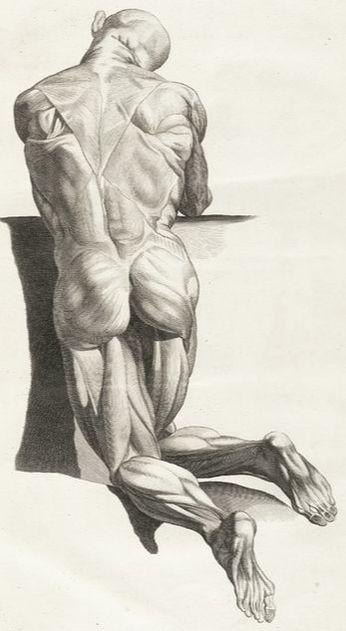
Let’s take just a moment and talk about Gracovetsky’s statement. In light of what we know about CHRONIC NECK PAIN and the relationship to loss of the neck’s NORMAL LORDOTIC CURVE, it is highly intriguing that Gracovetsky is talking about the importance of the lordotic curve in the lumbar spine (low back) as well. In other words, whether you have no lordosis (a straight low back when looking from the side) or a hyperlordosis (a “sway back”), it is likely affecting the integrity of the FASCIAL BIOMECHANICS —- even if you do not currently have pain.
Not surprisingly, there are any number of opinions on what constitutes ‘normal’ in this context (there is a great article on this subject over at The Movement Fix called The Best Kept Secret: Why People HAVE to Squat Differently). Let’s see how much today’s study agrees with this premise.
The very first thing the authors do is talk about ASYMPTOMATIC DISC HERNIATIONS as a proof that a significant portion of chronic back pain is not arising from spinal discs — something that I have been talking about since around Y2K. One of the coolest things they discussed was the fact that despite MRI not necessarily being a good method of imaging the low back — particularly if the problem is fascia-related — diagnostic ultrasound might be (HERE), as there is a definite visible difference in the shear between the three layers of the Thoracolumbar Fascia in people with low back pain versus people without (click the link as it will provide the most informative 15 seconds of your day).
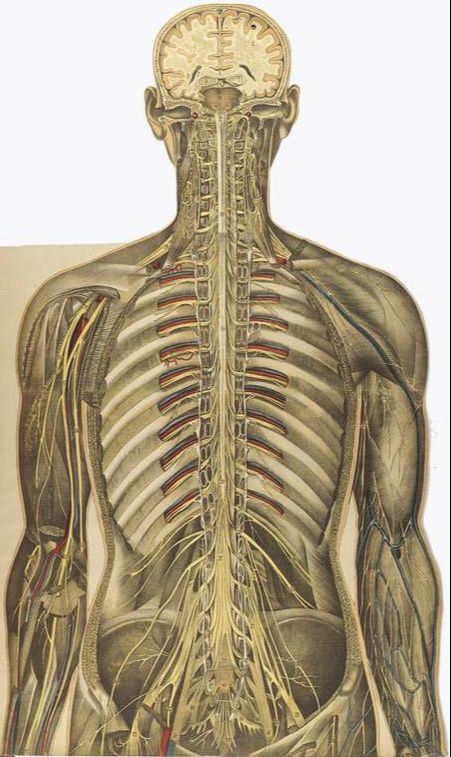
“The thoracolumbar fascia of both rodents and humans displays a dense innervation with nociceptive afferents. In addition, chemical stimulation of the lumbar fascia has been shown to elicit severe and particularly long-lasting sensitization processes. These studies indicate that the lumbar fascia exhibits a clear nociceptive neural capacity and therefore may be a source of pain in some cases of low back pain.
The nervous system seems to respond with a particularly strong and long-lasting sensitization towards mechanical, chemical, and electrical stimulation of the lumbar fascia. Taken together, these findings suggest that the lumbar fascia… represents a potential pain generator in patients with lumbar disorders.”
First off, the term nociceptive afferents is referring to pain-sensitive sensory nerves (as opposed to PROPRIOCEPTIVE SENSORY NERVES). When the inflammatory “sensitzation” process becomes especially long-lasting and intense it can turn into CENTRAL SENSITIZATION, best explained by the pain getting locked into the brain and playing on a continual loop. Furthermore, irritation to the Thoracolumbar Nerves can come from several sources. This nerve irritation can be MECHANICAL, ELECTRICAL (causes sciatica), or CHEMICAL. And yes, it’s not only possible to have all three simultaneously, it’s common.
The finale of this study was the authors sharing something you already know if you have followed my blog — spinal discs do not cause nearly as much pain as they are given credit for (HERE), as is also true with degenerative arthritis (HERE). So now that we know it’s likely that a great deal of chronic low back pain is arising from the Thoracolumbar Fascia instead of a “bad” disc, what can be done to heal it and make it better? Glad you asked!
Firstly, read my article TELL ME AGAIN WHY YOU WANT AN MRI?. Then realize that while I could give you a whole new post on the subject, why reinvent the wheel? HERE is the post I give my patients who are wanting to begin solving their chronic back issues on their own. Their goal is almost always the same.
They don’t want to live the rest of their lives on THE BIG FIVE, and if at all possible, to avoid SPINAL SURGERY (or another spinal surgery). This protocol is much more than suggesting some exercises and telling you to come back for A WEEKLY ADJUSTMENT. Oh; and if you like what you’re seeing, be sure to like, share, follow, or tag someone on FACEBOOK as it’s a fantastic way to reach the people you love and care about most.
