YOUR ORAL MICROBIOME COULD INDICATE CANCER
When it comes to health, MICROBIOME is everything. And while we usually think of one’s Microbiome as the bacteria living in one’s gut, it’s much more than that. Every different part of the body (SKIN, GUT, VAGINA, etc, etc) contains a unique microbial fingerprint. Furthermore, we know that these microbes are responsible for just about ever conceivable aspect of one’s health. Alter your microbiome and you alter your PHYSIOLOGY / HOMEOSTASIS. While some of this is due to the fact that 80% of your immune system resides in your gut (HERE), there are others.
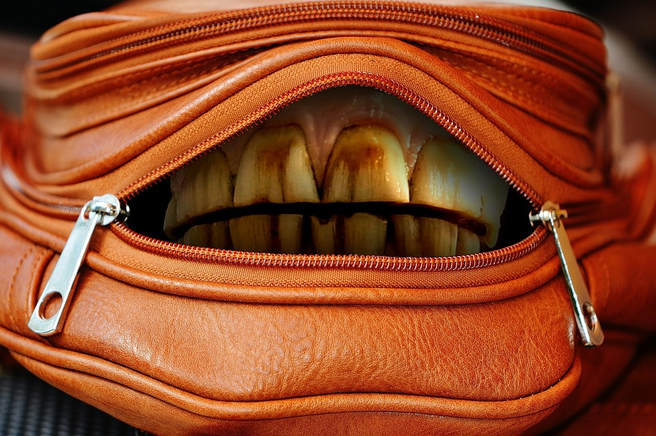
DR. WESTON PRICE showed everyone back in the 30’s, 40’s, and 50’s, how important whole foods were not only in keeping teeth healthy, but to actually maintain the bone structure of the jaw and face (HERE). Furthermore, he and DR. ROYAL LEE (they were both dentists) were warning of the dangers of ROOT CANALS decades before anyone else. We can now see the evidence that the germs in one’s mouth are actually linked to certain kinds of CANCER.
But before we make the jump to cancer, just remember that it’s a well known fact that periodontal gum disease is an inflammatory condition that has itself been associated with abnormal microbiome / microbiota. And as it’s other name (periodontitis) indicates by the suffix “itis,” it’s inflammatory. This is why it’s not surprising to see virtually every inflammatory disease on THIS LIST (cancer included) associated with gum disease and various sorts of DYSBIOSIS (in this case, oral dysbiosis).
In October of last year, Cancer Research gave us a massive and well-bibbed overview (440 sources) of this relationship called The Host Microbiome Regulates and Maintains Human Health: A Primer and Perspective for Non-Microbiologists that was done at least partially by dental researchers at Harvard. That same month, the journal Bioresearch Open Access (Gut Microbiota and Salivary Diagnostics: The Mouth Is Salivating to Tell Us Something) said that…
“The microbiome of the human body represents a symbiosis of microbial networks spanning multiple organ systems. Bacteria predominantly represent the diversity of human microbiota, but not to be forgotten are fungi, viruses, and protists. Consequently, it should not be surprising that gut dysbiosis can profoundly affect our wellbeing, lead to the manifestation of neuropsychiatric symptoms and conditions, and underlie a multitude of immune-related disorders (gut–brain-immune axis).
Gut dysbiosis may also exacerbate the progression of a number of common and often chronic diseases. Allergies, atherosclerosis, colorectal cancer, diabetes, inflammatory bowel disease, neurological conditions, and obesity are some examples. There is mounting evidence that the spectrum of microbial species living in the mouth is, both in diversity and in composition, a close representation of the microbiota inhabiting the upper GI tract.
Although the oral cavity is continuously subjected to a barrage of host and environmental insults, the oral microbiome remains relatively stable over time in healthy people. Given this fact, changes in the profile of the oral microbiome may provide correlative insight into the onset, progression, and recurrence of disease.”
Last year, the journal Medical Oncology published a study called Salivary Biomarkers in Cancer Detection in which they discussed various substances (many consisting of components of the microbiome) being used to detect various kinds of cancer. In August of last year, Seminars in Immunology published a study (Microbiota Dysbiosis in Select Human Cancers: Evidence of Association and Causality), where they talked about some of the cancers that have known microbial fingerprints, “colorectal cancer, head and neck cancer, pancreatic cancer, and lung cancer“.
The most amazing part of this study is found in the title — the authors suggested that there is a causal relationship between dysbiosis and various sorts of cancer — a relationship that in many cases, is proving to be bi-directional. Let’s now take a look at some of the cancers that are specifically associated with oral dysbiosis.
- THE ORAL FUNGUS / PERIODONTAL DISEASE CONNECTION: It’s common knowledge that there is a relationship between periodontal disease and cancer. Likewise, the link between long term fungal infections and cancer is nothing new. We see these facts working together in a study (The Oral Fungal Mycobiome: Characteristics and Relation to Periodontitis) from last July’s issue of BMC Microbiology, where the authors concluded, “We observed trends of higher Candida abundance in participants with periodontal disease, and participants with greater tooth loss.” This should not be surprising in the least, especially once you realize that both candida (yeast) and cancer are both fed by sugar (HERE and HERE) as are all infections, dysbiotic or otherwise (HERE). Also be aware that while these various infections are fed by sugar, they frequently begin with antibiotics (HERE).
- ORAL MICROBIOME, CANDIDA YEAST, AND MOUTH CANCERS: The first thing I must mention here is that according to any number of sources (this one from 2016’s issue of Medicine — Oral Sex and Oropharyngeal Cancer) “Sixty percent of oropharyngeal cancer reported in the United States is associated with HPV infections. Individuals who practiced oral sex with multiple partners are at risk for developing oropharyngeal cancer.” Now that that’s out of the way….. Two studies from December’s issue of Scientific Reports (Variations in Oral Microbiota Associated with Oral Cancer and Alterations in Oral Bacterial Communities are Associated with Risk Factors for Oral and Oropharyngeal Cancer) both showed the same thing — that a dysbiotic oral microbiome is associated with oral cancers. December’s issue of Frontiers in Microbiology (The Microbiome of Potentially Malignant Oral Leukoplakia Exhibits Enrichment for Fusobacterium, Leptotrichia, Campylobacter, and Rothia Species) showed essentially the same thing. “Oral leukoplakia presents as a white patch on the oral mucosa and is recognized as having significant malignant potential. Colonization of these patches with Candida albicans is common.” After doing microscopic studies of these white patches, the authors concluded that “Oral leukoplakia exhibits an altered microbiota that has similarities to the microbiome of colorectal cancer.“
- ORAL MIBROBIOME AND TONGUE CANCERS: What we see time and time again is that when it comes to microbiome, the word “diversity” is not only good, it’s of critical importance for health. Typically speaking, the more diverse one’s microbiome (the larger the number of different species of microbes), the more healthy the microbiome, and the more healthy the individual. A few short months ago, Oncotarget (Bacteriome and Mycobiome Associations in Oral Tongue Cancer) revealed that, “Oral squamous cell carcinomas are a major cause of morbidity and mortality, and tobacco usage, alcohol consumption, and poor oral hygiene are established risk factors.” The authors, from various institutions in Cleveland, OH, concluded after looking at the tongues of 39 individuals with cancer and 39 without, that “Microbiome profiling, principal coordinate, and dissimilarity index analyses showed bacterial diversity and richness, and fungal richness, were significantly reduced in tumor tissue compared to their matched non-tumor tissues.“
- ORAL MICROBIOME AND HEAD & NECK CANCERS: Just a couple short weeks ago, JAMA Oncology (Association of Oral Microbiome With Risk for Incident Head and Neck Squamous Cell Cancer) showed that if people have increased amounts of certain bacteria in their mouths (in this case Corynebacterium and Kingella) they have a “decreased risk of head and neck squamous cell cancer.” I would assume that the opposite is true as well (can anyone say dysbiosis?)
- ORAL MICROBIOME AND ESOPHAGEAL CANCERS: As we make our way down the body, we get to the esophagus — the tube that connects your mouth to your stomach. Just last month, Cancer Research carried a study called Oral Microbiome Composition Reflects Prospective Risk for Esophageal Cancers, in which they concluded that, “the abundance of the periodontal pathogen Porphyromonas gingivalis trended with higher risk of esophageal squamous cell carcinoma, and depletion of the commensal genus Neisseria and the species Streptococcus pneumoniae was associated with lower esophageal adenocarcinoma risk.” In other words, certain strains of bacteria were a risk factor for esophageal cancer, while certain strains were protective against esophageal cancer.
- ORAL MICROBIOME AND LUNG CANCER: Back in 2015, a group of 14 Chinese researchers published a study in the American Journal of Cancer Research (Discovery and Validation of Potential Bacterial Biomarkers for Lung Cancer) showing a relationship there as well. In this case the species “Capnocytophaga and Veillonella were significantly higher in the saliva from lung cancer patients, which may serve as potential biomarkers for the disease detection/classification.“
- ORAL MICROBIOME AND STOMACH CANCERS: The Journal of Periodontology Online (Chronic Periodontal Disease, Periodontal Pathogen Colonization, and Increased Risk of Precancerous Gastric Lesions) concluded that “Compared with the control group, patients with precancerous lesions of gastric cancer experienced higher prevalence of bleeding on probing, higher levels of T. denticola and A. actinomycetemcomitans, and less bacterial diversity in their saliva. Findings of the present study provide new evidence suggesting that periodontal pathogen burdens and bacterial diversity in the oral cavity are important factors contributing to a potentially increased risk of developing precancerous gastric lesions.” In other words, protective microbiomal diversity is crowded out by increased numbers of pathogenic bacteria (the definition of dysbiosis).
- ORAL MICROBIOME AND BREAST CANCER: Thanks to our over-the-top sugar consumption, massive exposure to ENDOCRINE DISRUPTORS (including chlorine, which is there for the express purpose of killing bacteria), BREAST CANCER is an increasingly common problem among Westernized women. A brand new study from Oncotarget (Breast Tissue, Oral and Urinary Microbiomes in Breast Cancer) showed abnormal urinary and fecal microbiota, as well as differences in the microbiomes of the tumors themselves. However, there were no noted differences in the oral microbiomes. However, other studies, such as Periodontal Disease and Breast Cancer: Prospective Cohort Study of Postmenopausal Women from last summer’s issue of Cancer Epidemiology, Biomarkers & Prevention, have been more adamant about a link. These Harvard researchers stated, “Periodontal disease, a common chronic inflammatory disorder, was associated with increased risk of postmenopausal breast cancer, particularly among former smokers who quit in the past 20 years.“
- ORAL MICROBIOME AND PANCREATIC CANCER: With a 7% chance of living five years, pancreatic cancer carries one of the worst prognoses in cancer. Last month’s issue of the Cancer Journal (Oral Health and the Oral Microbiome in Pancreatic Cancer: An Overview of Epidemiological Studies) revealed that “Analyses of antibodies to pathogenic and/or commensal oral bacteria in prediagnostic blood provided evidence that some oral bacteria and oral microbial diversity may be related to pancreatic cancer. Overall, the data present a plausible but complex relationship among pancreatic cancer, the oral microbiome, periodontal disease, and other risk factors that might be explained by systemic effects on immune and inflammatory processes.” In a study (Human Oral Microbiome and Prospective Risk for Pancreatic Cancer: A Population-Based Nested Case-Control Study) from this month’s issue of Gut, the authors were a bit more blunt about their their conclusions. After comparing the oral bacterial content of over 700 individuals with and without pancreatic cancer, they concluded that “oral pathogens were associated with higher risk of pancreatic cancer. This study provides supportive evidence that oral microbiota may play a role in the etiology of pancreatic cancer.” The authors went on to explain which bacteria appeared problematic and which appeared protective.
- ORAL MICROBIOME AND COLON CANCER: Three months ago, the same journal — Gut (The Oral Microbiota in Colorectal Cancer is Distinctive and Predictive) carried an Irish study that stated, “Microbiota alterations are linked with colorectal cancer and notably higher abundance of putative oral bacteria on colonic tumours. Several oral taxa were differentially abundant in colorectal cancer compared with controls. Combining the data from fecal microbiota and oral swab microbiota increased the sensitivity of this model to 76%.” In other words, a simple stool sample and swab of the mouth could determine whether or not colon cancer was present over three quarters of the time. Watch as those numbers get even crazier in the issue of NPJ Biofilms and Microbiomes that came out two months ago today (High-Resolution Bacterial 16S rRNA Gene Profile Meta-Analysis and Biofilm Status Reveal Common Colorectal Cancer Consortia). “Colorectal cancer (CRC) remains the third most common cancer worldwide, with a growing incidence among young adults. Multiple studies have presented associations between the gut microbiome and CRC, suggesting a link with cancer risk. Results from the Malaysian cohort and the expanded meta-analysis confirm that CRC tissues are enriched for invasive biofilms and oral pathogens. Overall, our meta-analysis demonstrates that the vast majority (over 80%) of CRC cases contain aberrant microbial signatures indicative of dysbiosis.” Did you catch that? If you have colon cancer, you have greater than a 4 out of 5 chance of having a concurrent DYSBIOTIC SITUATION. Not sure what a BIOFILM is? Click the link.
What are you going to do to keep your body free of dysbiosis and the invariable “LEAKINESS” (not to mention cancer) that always seems to follow? Easy; make sure to live a healthy lifestyle. Fortunately for you, I’ve given you plenty of information on what this entails and how to get there from here (HERE). I would suggest you start creating your very own EXIT STRATEGY today! And like, share or follow on FACEBOOK while you are at it!
