PATELLO-FEMORAL SYNDROME
WHAT IT IS AND HOW TO DEAL WITH IT EFFECTIVELY?
“Consensus is lacking regarding the cause and treatment of the syndrome. Many theories have been proposed to explain the etiology of patellofemoral pain. These include biomechanical, muscular and overuse theories. In general, the literature and clinical experience suggest that the etiology of patellofemoral pain syndrome is multifactorial.” Dr Mark S. Juhn of Seattle’s University of Washington School of Medicine from an article published for the November 1999 issue of the American Family Physician (Patellofemoral Pain Syndrome: A Review and Guidelines for Treatment).
“Historically, clinicians have used a myriad of interventions, many of which have little, if any, supporting evidence.” Drs. Lori Bolga and Michelle Boling from 2011’s An Update for the Conservative Management of Patellofemoral Pain Syndrome: A Systematic Review of the Literature from 2000 to 2010
As I continue our series on THE MOST COMMON PROBLEMS I SEE at Schierling Chiropractic, LLC, today we will tackle a very common problem — something most frequently called “Patellofemoral Syndrome”.
Depending on whose research you believe, the number one or number two reason that people visit “Sports Physicians” is Palellofemoral Syndrome (aka Patellar Tracking Syndrome, Chontromalacia Patella, and several others). The quote at the top of the page was written over 15 years ago, and comes from a paper that is still widely considered to be the definitive word on the topic. The pain itself is found most commonly in the front of the knee and is thought to arise from contact between the underside of the patella (knee-cap) and the thigh bone (femur). It occurs most often in younger female athletes, although it is commonly found in runners of all ages (male as well), basketball players, as well as athletes from various other sports.
Although there are a wide array of treatment options for this problem, the “gold standard” involves various exercises to strengthen the quadriceps (front thigh muscles). My goal today is to show you why this is not necessarily always the best or only option — particularly if you are one of those who may have been told that a Lateral Release Surgery is your only option. Let me first say that many of those I see diagnosed with Patellar Tracking Syndrome actually have some form of TENDINOSIS (it is important to understand the difference BETWEEN TENDINITIS AND TENDINOSIS). This Tendinosis can occur in several different places (click on image at left) and my be a concurrent problem, or may mean the person was misdiagnosed. Just understand that when we talk about Tendinosis of the knee, this can be in the form of Quadriceps Tendinosis or Patellar Tendon Tendinosis (HERE — named according to the specific tendon it’s found in). Sometimes, this can be confused with OSGOOD SCHLATTER SYNDROME — particularly in a child or youth who has not yet developed the large “Tibial Tubercle”.
As you might imagine, most sources will tell you that Patellofemoral Syndrome is caused by weak quadriceps (front thigh muscles). I am personally not convinced that this is always the case. In fact, I would say that this assessment is often times blatantly incorrect.
I see a lot of people with Patellar Tracking Syndrome and more often than not, find the opposite to be true (weak hamstrings being overpowered by the quads, which are — or at least should be — the strongest muscle group in the body). This is particularly true in athletes. In most athletes (particularly those who are well-trained or weight lifters) the quadriceps are significantly stronger than the hamstrings. Not only that, but when people train their legs in the weight room, most of the common exercises for legs (squats, hack squats, presses on the leg sled, leg extensions) mostly or entirely work the quadriceps. In fact, other than maybe doing some hamstrings curls, I find that many athletes are doing very little for their hamstrings.
Below is a video of Jennifer that was shot three days ago. Although I had treated Jennifer for Patellofemoral Syndrome over a decade ago, it only took one treatment to solve a (severe) knee problem that she had dealt with for five years. I do not actually remember doing this treatment, but when I recently suggested that she might have Fasical Adhesions in her neck, she reminded me of the Fascial Adhesions that she had in her knee. I told her that I would be doing an article on that particular problem on Monday, so she agreed to do a video for us (thanks Jennifer!).
Besides the quadriceps strengthening exercises, one of the most common methods of treating people with with Patellar Tracking Syndrome involves the use of NSAIDS. As you might guess, I am not a big fan. And as for CORTICOSTEROID INJECTIONS; because the cartilage surface of the underside of the knee may already be ‘soft’ (Chondromalacia Patella), the last conceivable thing you would ever want to put into the knee is something that is likely to make it softer or degenerative, which is exactly what Corticosteroids do.
Symptoms of Patellofemoral Syndrome include pain in and around the knee. This is because, according to a 2009 article by Tom Plamodon, “The cause of pain and dysfunction often results from abnormal forces (e.g. increased pull of the lateral quadricep retinaculum with acute or chronic lateral PF subluxation / dislocation)“. In light of the fact that this is the medical community’s current thought process on this matter, this is an important statement to understand. And in order to grasp it, you’ll first have to understand what a RETINACULUM is. A Retinaculum (often referred to as an APNONEUROSIS) is simply a very wide, flattened or thin, fascia-like tendon. Listen to Wikipedia’s definition of a common treatment for Patellar Tracking Syndrome; the Lateral Release.
“A Lateral Release Surgery (also called a “Lateral Retinacular Release”) is a surgical procedure to release tight capsular structures (lateral retinaculum) on the outer aspect (lateral aspect) of the kneecap (patella). This is usually performed because of knee pain related to the kneecap being pulled over to the outer (lateral) side and not being able to run properly in the center of the groove of the femur bone as the knee bends and straightens.”
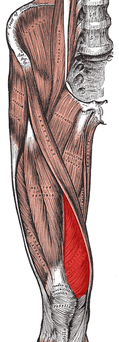
I want you to look at the picture to the right (the muscle in red is the vastus medialis) and think about something for a moment. If, as Dr. Plamodon above says, the lateral quadricep retinaculum has an “increased pull“, we need to ask ourselves why. Although we are almost always told that this is due to a weakness in the vastus medialis (the muscle on the inside front of the lower thigh opposite the vastus lateralis), I find that this is often not the case — or at least it does not tell the entire story. Instead, the problem is that there is very often ADHESED FASCIA (retinaculum) in and around the area of the vastus lateralis. This area of adhesion can encompass the lower ITB as well. What causes this? Although I am not certain, I would speculate that it has to do with the fact that FASCIA can be broken down and scarred by either chronic repetition (i.e. running) or traumatic injuries — both being exceedingly common in athletes.
Although strengthening of the quadriceps usually solves this particular pain, it can actually worsen the imbalance between the quadriceps and the hamstrings. It was not that long ago that I read an article talking about the incredible increase in the numbers of cases of non-contact knee ruptures seen in today’s athletes — particularly female athletes. The authors touted the fact that the number one cause of non-tramatic ACL ruptures in the female population, the quads were overpowering the hamstrings.
For more information about PATELLO-FEMORAL SYNDROME and how to avoid a “Lateral Release” surgery, just take a few minutes to click and read the link. You may want to look at our COLD LASER PAGE as well.