IMPLICATIONS OF FASCIA’S ABILITY TO CONTRACT
Although it’s not a totally new concept (I’ve spoken of it on several occasions — HERE, HERE, and HERE), a brand new study shed even more light on fascia’s ability to act as a contractile tissue. DR. ROBERT SCHLEIP led a team of 10 researchers from Europe and Australia that published a study on this topic (Fascia Is Able to Actively Contract and May Thereby Influence Musculoskeletal Dynamics: A Histochemical and Mechanographic Investigation) in this month’s issue of Frontiers in Physiology.
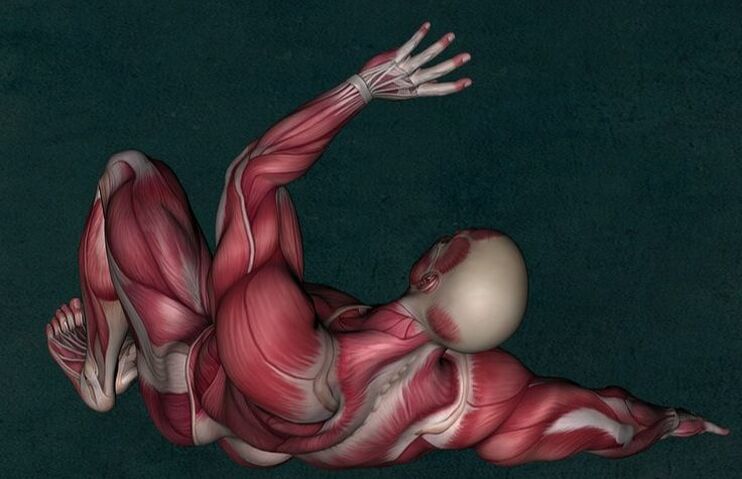
Despite the recent work on this subject (not to mention the fact that physiologists are well aware of its ability to transmit mechanical forces), FASCIA is still largely believed to be “inert” — a tissue of biomechanical importance, but “only serving a passive role“. Take a look at this, however. For the better part of three decades, studies — numerous studies — have shown that certain types of connective tissues can, in similar fashion to muscles (but on a much smaller scale) contract…..
“In contrast to this common assumption there have been sporadic indications of a more active role of fascia due to an inherent ability to actively contract. These indications include the reported phenomenon of ‘ligament contraction’ of human lumbar fascia in response to repeated isometric strain application in vitro, the documented presence of interspersed cells with smooth muscle-like appearance in the human fascia cruris, and the clinical experience of seemingly animated fascial tonus changes in response to fascia manipulation treatments frequently reported by manual therapists and acupuncturists.”
While these authors spoke of the tissue shortening and constricture that occurs in FIBROTIC PROCESSES and microscopic “SCAR TISSUE,” the sort of contractile ability (contractility) we are going to discuss today is not only that which is functionally pathological, but that which is considered normal. While we will certainly deal with the former, please realize that depending on context, fascial ‘contraction’ is a normal part of the physiological process of FASCIA BIOMECHANICS. How did these scientists prove this once and for all?
The researchers took tissue slides of fascia from human cadavers that had no known pathologies, from the right FASCIA LATA, PLANTAR FASCIA, and the THORACOLUMBAR FASCIA lateral to L3 for comparisons. The thoracolumbar fascia was then dissected out of 40 rats and hooked up to sensitive force-measuring devices in baths of a type of Ringer’s solution to see what would happen (contraction or not) when exposed to certain chemical stimulus added to the bath.
“Our immunohistochemical plus mechanographic findings and related force calculations suggest… active cellular contractility of fascial tissues may be able to impact musculoskeletal dynamics. Our findings suggest that, due to the contractile behavior of inherent myofibroblasts, human lumbar fascia may be able to change its stiffness in a time frame of minutes to hours and thereby possibly affect motoneuronal coordination.”
That was a mouthful, but allow me to break it down for you. It’s known that MYOFIBROBLASTS (a special kind of FIBROBLAST — cells that create both COLLAGEN and the EXTRACELLULAR MATRIX) have contractile properties. These authors discovered that when the thoracolumbar fascia is exposed to certain types of inflammatory mediators (although there were many, TGF-BETA was the most important of these, while caffeine was the most well known), it “contracts“.
Where are myofibroblasts found in the greatest numbers? Not surprisingly, the thoracolumbar fascia (see earlier link). This is one more reason that the “disc” model of low back pain, while certainly not going away entirely, is slowly but surely being relegated to second fiddle (HERE). Some of the features of thoracolumbar-induced low back pain include….
- “The finding of clearly nociceptive nerve endings in human lumbar fascia“. This leads to pain, which I wrote about HERE.
- “A reduction in thoracolumbar shearing motion has been described in chronic low back pain patients compared with healthy controls.” WATCH IT in action in these two seven second videos.
- “Toughness of the perimysium” is a likely factor as well. The PERIMYSIUM is the fascia layer that surrounds bundles of muscle fibers (LIKE THIS) and is a factor seen in both age and injury / overuse (although this study showed less correlation to age than previous studies). “Several myofascial pathologies associated with increased myofascial stiffness are associated with changes in the perimysium.” Be aware that this increased stiffness runs hand in hand with INCREASED FASCIAL THICKENING and even “FASCIA DENSIFICATION,” which are both heavily associated with CHRONIC TRIGGER POINTS as shown by these authors.
- DIMINISHED PROPRIOCEPTION. “Any alteration of mechanosensation is potentially able to modify muscle coordination and reflex regulation of functional joint stability. Thus, we suggest that short-term stiffness changes in fasciae might possibly be sufficient to impact neuromuscular coordination. A temporarily increased fascial stiffness—e.g., due to an altered sympathetic nervous system activation and/or altered cytokine expression—might be able to modify or disrupt the accuracy of proprioception and coordination, which could possibly contribute to the likelihood of injuries and of subfailure injuries.” This is doubly significant considering we live in a heavily inflamed world (“increased cytokine expression” — HERE) as well as varying chronic states of SYMPATHETIC DOMINANCE.
- “We suggest that a local and/or temporal increase in fascial contractility might also contribute to long-term tissue contracture, which includes matrix remodeling.” In other words, the body’s connective tissues can be dragged into a vicious cycle leading to “permanent tissue contracture.” This is why REMODELING TISSUE back to it’s original structure / function — or as close as possible — is such a big deal. And for those who wonder if this method of treatment is effective; there is no need to wonder (HERE).
- “The presence of micro-injuries in human lumbar connective tissues and a resulting corrupted neuromuscular coordination in addition to other downstream effects have been suggested as novel explanations for some cases of low back pain…. The observed minor changes in lumbar fascia stiffness may possibly constitute a contributing factor to back stability and low back pain.” This is where the rubber meets the road in regards to back pain. Interestingly, these authors mentioned that studies have already shown that, “lumbar fascia from low back pain patients [has] myofibroblast density comparable to that found in frozen shoulder.” Think about that and let it soak in for a moment.
- The process is likely related to lumbopelvic SUBLUXATION. Subluxation is the chiropractic term meaning loss of alignment or motion and is analogous to something discovered by the OSTEOPATHIC PROFESSION about the same time the Palmers were defining and developing chiropractic. “Minor fascial stiffness changes, as observed in our study, could be involved in – at least some cases of – the phenomenon of vertebral somatic dysfunction described as a minor intervertebral disorder in the osteopathic literature.” This was mentioned in the same paragraph as the importance of POSTURE.
Listen to the author’s final conclusions….
“Our findings question the common clear distinction between active tissues and passive tissues in musculoskeletal dynamics. While the contraction forces observed in our study do not support a significant contribution of active fascial contractility in time frames of seconds (as are frequently considered, e.g., for locomotor dynamics), they suggest that active changes of fascial stiffness might play contributory roles to the motoneuronal coordination aspect of low back stability and other musculoskeletal parameters when viewed in a time-window of several minutes and longer.
As some chronic disorders develop asymptomatically over a large time frame and are characterized by increased tissue stiffness, the potential contribution of fascial MFB activity merits further investigation.”
This last sentence is critical to grasp — that chronic disorders can, and frequently do, develop slowly and asymptomatically over time. Until they are no longer asymptomatic. This is part of what leads people into the world of CHRONIC PAIN and even CENTRAL SENSITIZATION. It’s also why taking care of your body biomechanically and living an anti-inflammatory lifestyle are of such importance.
Fortunately for you, I have provided a NICE LIST of things you can be doing to help accomplish this — or at least start the process. How else do you really expect to get better? WITH DRUGS? And as always, if you appreciate what we’re doing here, be sure and spread the wealth by sharing this with the people you love and value most (just like, share, or follow on FACEBOOK!).

One Response
This is incredibly important research heading in the right direction, but when are even these leading researchers going to make the connection between a BODY-WIDE disruption in the fascia, and a common “mysterious” pain “syndrome” – Fibromyalgia?
I have hypothesized for years now, that my own pain and limitations are perfectly explained by a dysfunction in the fascia body-wide, where it is permanently “contractured”. Initially I thought it might be all about “adhesions”, related to interstitial fluids becoming more glue-like than lubricant-like. Maybe that is going on as well, but I have come to also believe that fascia through the whole body is “tight”, maybe this is because the fascial envelope is “shrunk”. So what is really going on, I am less inclined to think it is “involuntarily tensed” is the sense that red muscle tissue can be tensed by motor neurons, but rather that it has changed in its biochemical properties so that it is “shrunk”, like wet leather drying out.
Now my thinking is challenged by this new study which finds that this contracting of fascia can occur quite rapidly under certain conditions. But does this prove it can happen rapidly in real life, or did the conditions of the study enable a process that is normally slow, to be sped up?
I have been saying for years that if the body’s fascia could be modelled and then a slight shrinkage modelled, the resulting worst “pinch points” might be where the “tender spots” are in FM! Or alternatively, those tender spots might be where adhesions are naturally the worst due to complex intersections of muscle fibres that make the spot more prone to stagnation, toxicity and adhesions if the interstitial fluids become more viscose.
I’ve been getting better for 8 years now (after getting worse for 25 years), by using self-treatments that make sense under this hypothesis of “what is wrong”.