FASCIAL ADHESIONS, CHRONIC PAIN, AND CUTANEOUS NERVE ENTRAPMENTS: MORE COMMON THAN YOU EVER DREAMED!
I’ve talked at length here about the way that SCAR TISSUE (the FIBROSIS that in essence causes MICROSCOPICALLY ADHESED FASCIA) is not only a major cause of CHRONIC PAIN, but that said tissue has the potential to be as much as 1,000 times or more pain-sensitive than normal tissue (HERE is the research). Before talking about the ways that Fascial Adhesions entrap cutaneous nerves, I want to take a moment to discuss several distinct types of pain patterns; dermatomal, myotomal, and scleratomal or scleratogenous, all of which arise from a developing part of the embryo known as the somite.
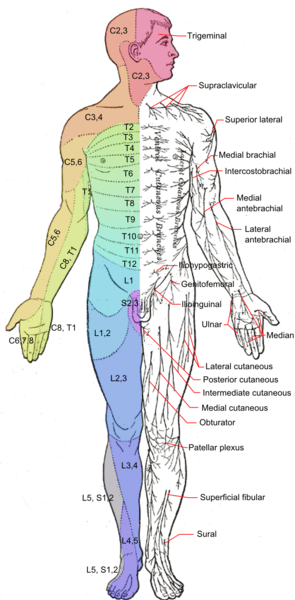
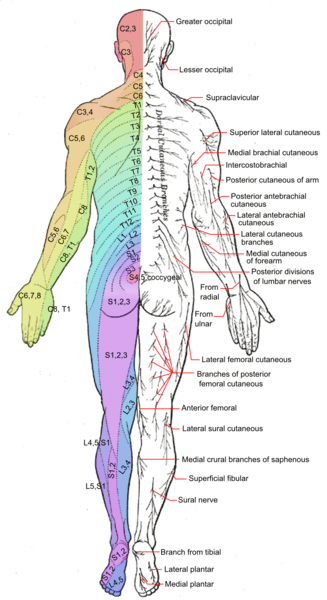
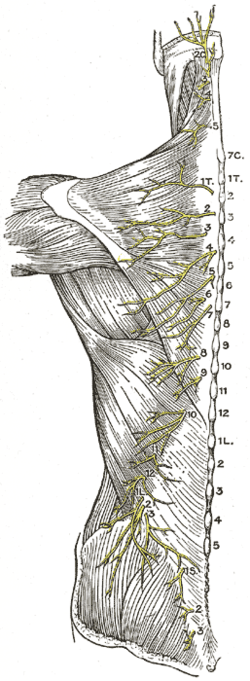
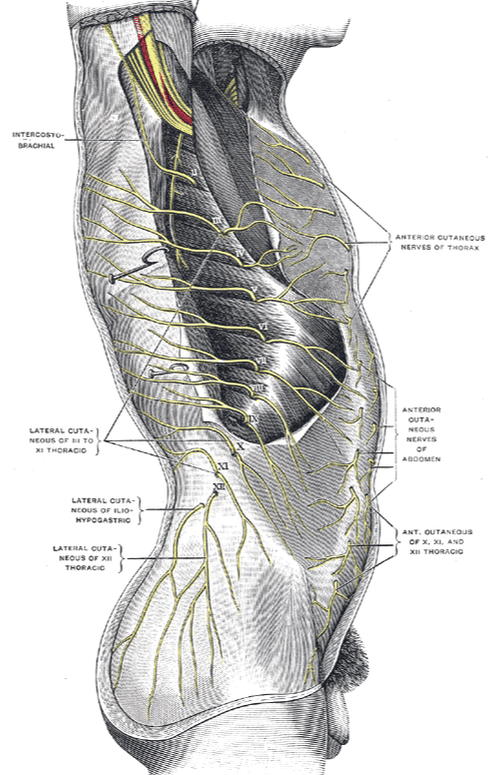
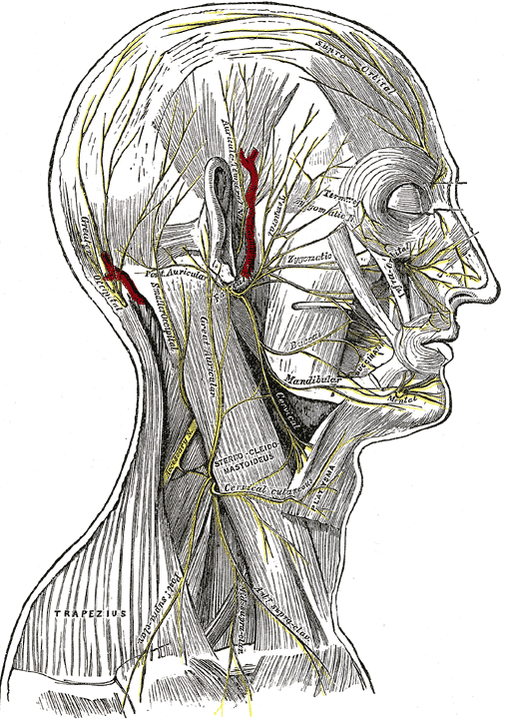
- DERMATOMAL PAIN PATTERNS: In the same way that we know which nerves control what organs, we also know what specific areas of sensation are controlled by each spinal nerve. These areas are known as dermatomes. In other words, a dermatome refers to the area of skin innervated by a single spinal nerve. For instance, if a person had severe pain in a dermatomal pattern on their abdomen, it would not be a shock to see them break out with SHINGLES a day or two later (the herpes zoster / chickenpox virus hides in the nerve root and attacks the length of said nerve if a person BECOMES OVER-STRESSED or has a weakened immune system). Dermatomes are what allow us to look at what part of a patient’s hand is numb and tell what nerve is the likeliest one being pinched in the neck or upper back. Dermatomal patterns of sensation are seen in the pics above, and while cutaneous nerve entrapments will often create patterns similar to dermatomal patterns, they are usually not an exact match.
- MYOTOMAL PATTERNS OF DYSFUNCTION: Myotomes are the muscle’s equivalent of the dermatome, except that they are measures of motor function instead of sensory. In other words, a myotome is muscle or group of muscles controlled by a specific spinal nerve. So if we’ve figured out what dermatome is affected in our patient, we can start testing things like grip strength, the ability to spread one’s fingers against resistance, or maybe the ability to stand on one’s heels or toes, to see if the dermatomal level of lesion matches the myotomal level. Again, myotomes are a motor issue, not sensory (which does not mean that muscles cannot be a source of pain).
- SCLERATOMAL OR SCLERATOGENOUS PAIN PATTERNS: The Scleratome refers to all the deep tissues that are controlled / innervated by a specific spinal nerve. Scleratogenous patterns of pain go back to embryonic development (again, the somite) and encompasses the specific referral patterns of specific deep tissues (bone, cartilage, LIGAMENTS, TENDONS) controlled by a specific spinal nerve.
- TRIGGER POINT PAIN REFERRAL PATTERNS AND TENDER POINTS: I have written extensively about TRIGGER POINTS and their pain referral patterns (“Tender Points” are said to be Trigger Points that do not refer pain, but are locally painful).
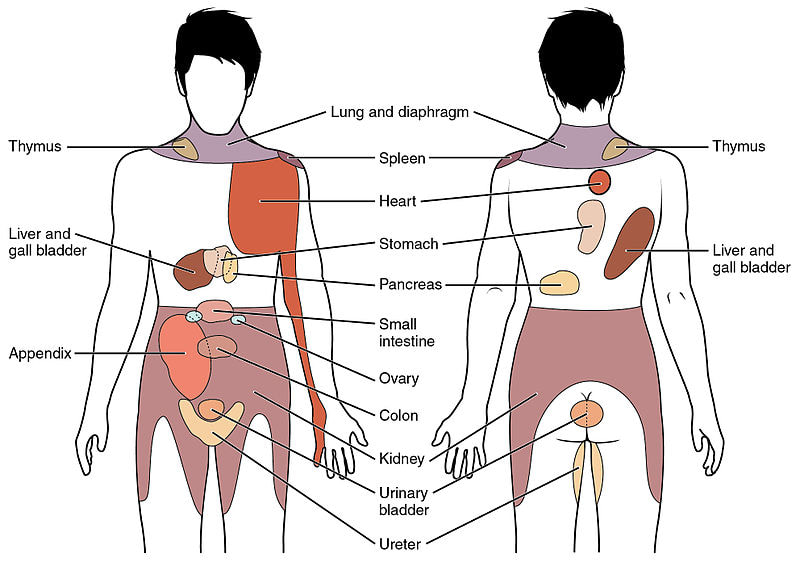
- VISCERAL PAIN REFERRAL PATTERNS: The soma refers to the body (think “somite” here) and the viscera refers to the organs. And yes, organs have specific referral patterns as well, although far less is known about them than somatic pain referral. Visceral referral is thought to arise from a combination of embryological origins, the level of spinal cord innervation / nerve supply, and yes, the fascial connections that are found throughout the organ systems (the last pic at the bottom of the post has a diagram showing visceral pain referral patterns from specific organs).
As you can see, there are a lot of ways to refer pain, which is why it can sometimes be difficult to nail down exactly what is going on in a suffering individual. What I want to do now is talk about still another mode of potential pain referral — the entrapment of cutaneous nerves in superficial connective tissues, i.e fascia.
The very first thing we need to know about this phenomenon is what cutaneous nerves are. The word “cutaneous” simply means having to do with the skin (think cuticle here — the word “cutis” is Latin for skin). Thus, cutaneous nerves are the end-branches of larger nerves, which essentially supply sensation to the surface of the body — i.e. the skin.
Don’t be fooled however, because when you adversely affect a cutaneous nerve you will probably affect a whole host of motor functions that most of us never think about. Some of these include functions associated with the healing of wounds, immune system functions / inflammation, blood flow, tissue growth and repair, secretion of sweat and oils, barrier activity, temperature regulation, goosebumps, and any number of others.
Are entrapment syndromes of the cutaneous nerves real, or am I blowing a lot of hot air here. Although YESTERDAY’S POST on entrapment of the Superior Cluneal Nerve (SCN) should have answered this question, we’ll delve in a bit deeper today and talk about other entrapment syndromes regarding other cutaneous nerves. Before we do, I want you to understand that it is in the cutaneous nerves where we find SMALL FIBER NEUROPATHY — one of the hallmarks of FIBROMYALGIA (the only surefire way of testing for this problem is via biopsy).
People with small fiber neuropathy typically struggle with numbness, tingling, burning, and other paresthesias of the extremities, and it’s not uncommon that they have hypersensitivity to heat, cold, or both, as well. Whatever the source of pain, science is increasingly insistent that dealing with it is critical in order to diminish the chances of developing CENTRAL SENSITIZATION.
“Nerves travel to the upper and lower extremities and traverse the various joints along their paths. Unfortunately, these nerves can become compressed or entrapped at various regions of the extremities, especially at “tunnel” regions, where they may be predisposed or vulnerable to compression. Neurosurgeons, among other surgical specialists treat these entrapment neuropathies, which can account for 10-20% of a practice’s cases.” From a September 2017 article for Medscape (Nerve Entrapment Syndromes) written by a group of neurosurgeons, orthopedic surgeons, and plastic surgeons.
Now that we’ve ascertained that nerve entrapments are not only real, but common as well, it would be helpful to have some kind of idea of how common they are — particularly entrapments of the cutaneous nerves. Some are so common that they have their own name.
For instance, when there is entrapment of the Lateral Femoral Cutaneous Nerve (LFCN), it is known as ‘Meralgia Paraesthetica’ (MP). Although its symptoms are different (sensitivity to light touch, sensitivity to temperature extremes, buttock or groin pain, problem worse with tight pants, constant pain, burning, stinging, etc), MP is sometimes confused with IT-BAND issues due to its proximity.
Because one of the more common types of pain is abdominal pain, it is likewise important to realize that the RIB CAGE and ABDOMEN are not uncommon areas to find entrapments of cutaneous nerves. For instance, the May 2014 issue of Continuing Education in Anaesthesia Critical Care & Pain (Abdominal Cutaneous Nerve Entrapment Syndrome) stated,
“Abdominal cutaneous nerve entrapment syndrome is a frequently overlooked diagnosis in patients with abdominal pain. Patients have often undergone a plethora of investigations, including diagnostic surgery and psychiatric review, before referral to Pain Management Services… resulting in significant anxiety, distress, and loss of work days for the patient. Up to 30% of patients with chronic abdominal pain have pain originating in the abdominal wall and abdominal cutaneous nerve entrapment syndrome (ACNES) is the most frequent cause of pain in these cases.”
When thinking about what I see in my clinic, I am not surprised at these numbers.
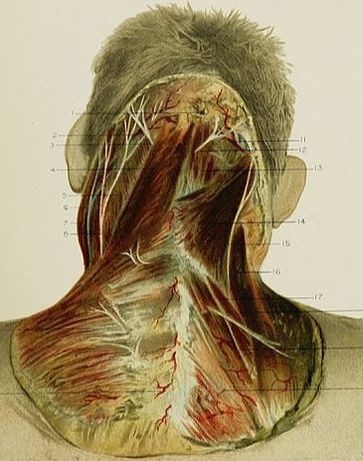
Other common cutaneous nerve entrapment syndromes involve various cutaneous nerves of the SKULL AND NECK. Take for instance the occipital nerves (those nerves at the back of the head). A study from the April 2016 issue of Headache (Occipital Neuralgia Diagnosis and Treatment: The Role of Ultrasound) had this to say.
“Occipital neuralgia is a form of neuropathic type of pain in the distribution of occipital nerves. Occipital neuralgia frequently occurs as a result of nerve entrapment or irritation by a tight muscle or vascular structure, or nerve trauma during whiplash injury. Ultrasound not only allows distinguishing normal from abnormal entrapped occipital nerves, it can identify the level and the cause of entrapment as well.”
Which leads into the next topic concerning cutaneous nerve entrapments — imaging.
First, realize that you are simply not going to see nerve entrapments of any kind, let alone of the cutaneous nerves, with plain film x-ray (anyone who has been on the medical merry-go-round due to NECK PAIN and HEADACHES caused by WHIPLASH already knows this).
Secondly, while you can sometimes see entrapments of larger nerves with MRI (for instance CARPAL TUNNEL SYNDROME — the most common nerve compression syndrome in the body), but you will not see entrapped cutaneous nerves (the median nerve that is compressed in CTS is not cutaneous). Imaging is slowly coming around, however, thanks to a improvements in an older technology, DIAGNIOSTIC ULTRASOUND. However, in many cases, even the newest units are not going to reveal the source of the pain. Why not?
After mentioning some of the things that can cause entrapment of cutaneous nerves (fibrous bands, scar tissue, fibrosis, masses, bony calluses, external compression, inflammation, and others), sports medicine physician, Phillip M. Steele, showed via his 64 page online seminar notes (Nerve Entrapments: Frequently Seen, Commonly Missed) exactly what’s stated in the title; these problems are common.
I’m going to go out on a limb here and say that cutaneous nerve entrapments are probably even more common than experts like Dr. Steele believe. Why? Because when you start talking about things like SCAR TISSUE / FIBROSIS as causes of cutaneous entrapment, all bets are off. Simply imagine how much easier it would be to bind a nerve in soft tissues that are deranged and TETHERED due to it looking / acting more like a HAIRBALL, than in healthy elastic tissue that looks more like well-combed hair under a microscope.
Which begs yet another question; what can be done to effectively deal with these entrapments? as ou probably already guessed, the peer-reviewed literature is definitely slanted towards invasive procedures such as INJECTIONS, NSAIDS, and various forms of tissue releases (surgery).
While I would never argue against the fact that in some cases — maybe even many cases — drastic measures like these might be required; likewise, in many cases — probably the majority of cases — the problems could be dealt with conservatively using various MANIPULATIVE TECHNIQUES, MASSAGE, or TISSUE REMODELING (for examples, CLICK HERE). And as I’ve written concerning treating those who might already be “CENTRALIZED,” what have you got to lose? Worst case scenario YOU TRY A TREATMENT and see what happens. It will either help or it won’t; it’s not going to somehow make you worse.
Be aware, however, that there are any number of societal issues at play that have undoubtedly led to a sharp spike in said nerve entrapments. Not surprisingly, INFLAMMATION has been mentioned as a causal factor many times in this post by people far smarter than I (inflammation always leads to fibrosis, which always leads to degeneration — HERE).
And with the vast majority of our adult population either OVERWEIGHT OR OBESE, this creates its own risk factors for cutaneous nerve entrapment simply because there is a SUBSTANTIAL LAYER OF FAT just under the skin (sub-cutaneous). Similarly, because so many Americans are both sedentary and HUNCHED OVER ALL DAY in the posture of chronic pain, chronic illness, and age; nerve entrapments occur easier as well (motion is lotion when it comes to the musculoskeletal and nervous systems).
All of this together is why an important part of almost anything I do involves educating patients or others who are willing to learn, about the things they can do to help them help themselves (HERE). Oh; and for those of you who love reading about fascia, check out my FASCIA SUPER POST with all 140 of my articles on fascia neatly organized and categorized.
People are complaining about my site — complaining that they are spending more time than they intended to spend. Feel free to join them. And while you’re at it, be sure to share the wealth. One of the best ways to reach those you love and care about most with pertinent health-related information (all completely free) is by liking, sharing, or following on FACEBOOK.

One Response
I’ve been hypothesizing for years, that the “tender points” in Fibromyalgia could be found to be at the very spots where the alignments of muscle strands, in complex junctions, will experience pressure should the fascia be contractured or adhered.
“…Whatever the source of pain, science is increasingly insistent that dealing with it is critical in order to diminish the chances of developing CENTRAL SENSITIZATION…”
And yet we have a whole institution very slow to move on from the hypothesis that common pain “syndromes” are “because of” a CNS dysfunction, rather than the CNS dysfunction being because of sources of REAL PAIN that they are too dam incompetent or intransigent to identify. The better I get, the more I need to manage my anger at the loss of so much of my life to this dam incompetence.
In fact I started saying years ago, and believe this more strongly than ever now, that there is SO MUCH PAIN in people with FM as a result of a BODY WIDE fascia dysfunction, that the CNS cannot possibly handle it. The FM sufferer is only ever aware of the one or two most painful spots on their body. But palpating almost anywhere, is like palpating a raw wound, and the palpation increases the pain at that spot so that it “breaks through” the CNS pain prioritization cascade. There IS real pain “like that of a raw wound” throughout the entire body. There IS a solid explanation for this pain. The health establishment needs to stop gaslighting us.