SCAR TISSUE, STRETCHMARKS, FASCIAL ADHESIONS, CHRONIC PAIN, AND CHRONIC RESTRICTION; KELOIDAL SCARS -vs- HYPERTROPHIC SCARS
 | 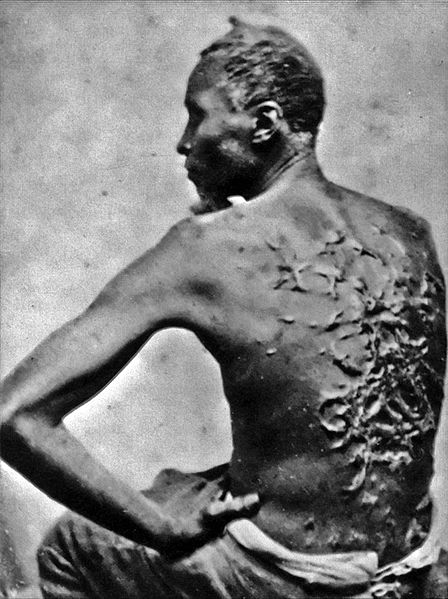 |  |
Let me start by saying that I am not trying to equate the back of the 16 year old male or the left of the 30 year old female on the right to the back of “Gordon” — the escaped Louisiana slave whose photo was taken at the height of the Civil War in 1863.
Realize that the photo on the left does not do justice to what is really going on with this kid, as it is difficult to convey the fact that the stretch marks are ‘welted’ off of his back about a quarter inch. As for the scars on the far right; this individual was complaining of chronic low back pain that would not respond to adjustments. Her scars were completely “invisible” until I started working on her, and her relief was immediate upon breaking the tissue.
There are two kinds of scar tissue that I want to talk about today, Hypertrophic Scars as we see in the pictures on the left and right, and the Keloids seen in the middle pic. Both involve an overgrowth of something called Granulation Tissue. Granulation Tissue is part of a normal healing process (see diagram below).
In a normal healing process, INFLAMMATION gets the ball rolling by attracting the chemicals and compounds that will repair the damaged tissue, which is exactly what it is supposed to do. After the inflammatory phase, the next step is ‘Fibroplasia and Granulations Tissue Formation’. The website Advanced Tissue says of Granulation Tissue….
“Granulating tissue is the new connective tissue that is created when the surface area is healing from an injury or wound. Due to the number of tiny blood vessels that appear at the surface of this new skin, the granulating tissue will be light red or pink in hue, and will be moist. Most is raised higher than the surrounding flesh, and oftentimes, it is bumpy (hence the term, granulating). Some people say it looks very similar to red grapefruit flesh. Despite its bright color, granulating flesh is healthy, and means that your body is working to provide a strong, protective new layer of flesh.”
Mere hours after the initial injury, FIBROBLASTS (or HERE) start laying down Granulation Tissue (Type III Collagen — a weak and inelastic form of Collagen) that will later be replaced by the stronger and more elastic Type I Collagen in a process called ‘Remodeling’ (SEE OUR COLLAGEN SUPER PAGE for more on the process of Tissue Remodeling). Not surprisingly, research says that Keloid Scars can cause restriction of joint motion if found around joints.
What you have to remember here is that anything that causes restriction has the potential to cause pain via loss of proprioception (HERE). Please understand that I am not saying that the Keloid itself is necessarily causing the pain, but that the restriction creates an increased potential for causing pain. This is why the combination of restricted movement and / or unbridled inflammation can be extremely problematic as far as joint health is concerned (HERE).
A March 2016 Medscape article by Otolaryngologist, Dr. Mimi Kokaska (Hypertrophic Scarring and Keloids) went on to say of Keloids, “they are frequently associated with negative wound healing factors, such as infection, excessive tension, foreign bodies, and repetitive trauma… Keloids are frequently associated with pruritus [itching] and pain… The central portion of keloids is severely ischemic [poor blood supply]. The investigators found greater expression of hypoxia-induced factor-1α, as well as less vascular density, in the center of these lesions than on the periphery.”
She also talked at length about the over-expression of various inflammatory mediators (IL-6 and IGF-1) that are thought to cause, “microvascular occlusion and subsequent hypoxia.”
It’s no secret that both hypoxia (poor oxygenation) and ischemia (poor blood supply) are problematic on many levels, including their heightened ability to induce pain.
Scar Tissue is very similar to a Keloid, only less severe in appearance. Part of the difference between Keloids and Hypertrophic Scars is that the later will sometimes improve in appearance over time, while Keloids can actually get worse — in some cases MUCH WORSE. Despite the fact that such scars are supposed to be, according to many sources, non-painful and merely a “cosmetic” issue, it’s easy to find sources and studies that say otherwise.
For example, in Dr. Kokaska’s above-mentioned article, she says of Hypertrophic Scars; “they are associated with adverse wound healing factors…” A 2014 study published in the journal Clinics (Update on Hypertrophic Scar Treatment) had this to say of Hypertrophic Scars….
“Hypertrophic scars are pathological scars resulting from abnormal responses to trauma and can be itchy and painful, causing serious functional disability. These scars are characterized by proliferation of the dermal tissue, with excessive deposition of fibroblast-derived extracellular matrix (ECM) proteins and especially collagen, over long periods and by persistent inflammation and fibrosis.”
For those interested, this study contains a great deal more information (much of it extremely detailed) about the physiology and pathophysiology of Hypertrophic Scars. As for what’s found in the quote above, my site has copious amounts of information on the ECM, FIBROSIS, and INFLAMMATION, as related to CHRONIC PAIN. And as for the last sentence that pertains to burn victims, unfortunately my Tissue Remodeling treatment does not work for burn scars (I’ve tried).
What does the medical community (AND INSURANCE INDUSTRY) say works for treating Hypertrophic Scars? The only real consensus is that nothing works very well. This is due mostly to the fact that surgical treatment almost always results in more of the same, and most of the non-surgical treatments for these types of scars (silicone spray and CORTICOSTEROIDS are both quite popular) cause their own unique problems as well tending to stop working once the treatment is stopped. What seems to work best?
A three year old study from Seminars in Cutaneous Medicine and Surgery (Low-level Laser (Light) Therapy (LLLT) in Skin: Stimulating, Healing, Restoring) touted some of the same benefits of LOW LEVEL LASER THERAPY that I have been talking about for the past decade.
After discussing its mechanism of action (photobiomodulation — see link) the group of seven medical doctors and Ph.D researchers stated, “LLLT has beneficial effects on wrinkles, acne scars, hypertrophic scars, and healing of burns. Inflammatory diseases such as psoriasis and acne can also benefit. The non-invasive nature and almost complete absence of side-effects encourages further testing in dermatology.”
HYPERTROPHIC SCARS AS RELATED TO STRETCHMARKS

What can I tell you about Hypertrophic Scars as related to Stretchmarks? Let me first say that I am not an expert on this subject — all I am giving you is my personal (and limited) experience with Stretchmarks in patients I see with pain. Secondly, this is not something I see lots of — in the almost two decades I have been doing Tissue Remodeling, I’ve probably seen less than 100 cases, although for whatever reason, that number seems to increasing dramatically.
Thirdly, for whatever reason, the oldest person I have seen with this sort of thing is about forty, with most being much younger. Fourthly, the cases I have seen are almost always related to a history of severe impact (falling out of trees, off horses, hit by a metal beam, four wheeler accidents, impact with a railroad track, etc, etc, etc). Some of these led to immediate chronic pain, while with others the pain did not show up until later. Fifthly, some of these scars are indented into the skin or below the surface like the pic directly above, while some are welted off the surface like the pics at the top.
And lastly, the stretchmarks that I have found thus far have always been located in the area of the THORACOLUMBAR FASCIA and occasionally into the mid back. TISSUE REMODELING has helped in most of the cases I’ve treated (the one at the very top of the page left, I just saw yesterday).
Beyond after-the-injury treatment, if you know you are prone to abnormal scarring, what could you do to help prevent it from forming in the first place (or at least slow it down)? Honestly, I would suggest you do what I recommend for nearly everyone — live your life in as anti-inflammatory manner as is humanly possible. Even though these pathological scarring issues have been called genetic; due to something called EPIGENETICS, the anti-inflammatory lifestyle is undoubtedly far more relevant than you ever would have dreamed. As to what some of this looks like, I would recommend you start by READING THIS POST on the subject.
HERE is a super cool testimonial from a young woman who had Hypertrophic Scarring that I treated, but was obviously not the sole source of her pain — she did not get relief until she went on a GFD. As for other hidden causes of inflammation, you might have many. If this is the case, you won’t find real relief from the mechanical issue until you start addressing the underlying chemical issue (inflammation). It’s your lucky day because I show you how to do exactly this (HERE). And for those of you who are particularly interested in fascia, make sure to check out my post with all 145+ articles on fascia organized into a unified post (HERE).
