STIMULATION OF FIBROBLASTIC ACTIVITY
FOR CHRONIC PAIN, DYSFUNCTION, AND FASCIAL ADHESION
Fibroblasts are dispersed in connective tissue throughout the body, where they secrete a nonrigid extracellular matrix that is rich in type I and/or type III collagen. When a tissue is injured, the fibroblasts nearby proliferate, migrate into the wound, and produce large amounts of collagenous matrix… fibroblasts also seem to be the most versatile of connective-tissue cells, displaying a remarkable capacity to differentiate into other members of the family. From the book Molecular Biology of the Cell
You gotta be cruel to be kind, in the right measure… Nick Lowe from 1979’s Cruel to be Kind
A few days ago I did a post on FIBROBLASTS, what they are, and why understanding them is critical to figuring out why you may be stuck as far as solving your particular CHRONIC PAIN SYNDROME (or maybe even your chronic illness — HERE) is concerned. Which begs the question; what can be done to stimulate these cells? I will get around to answering that momentarily.
But before we address the what part of this question, let’s take just a moment to discuss why. In other words, why would we care whether or not we activate fibroblasts? To understand this better, let’s take a look at FGF’s (Fibroblastic Growth Factors). According to a popular online encyclopedia’s listing, we see that……
“FGFs are important players in wound healing. They are multifunctional proteins with a wide variety of effects; they are most commonly mitogens [having to do with increased tissue proliferation via cell division] but also have regulatory, morphological, and endocrine effects. They have been alternately referred to as “pluripotent” [extremely potent] growth factors and as “promiscuous” growth factors due to their multiple actions on multiple cell types.
One important function of FGF1 and FGF2 is the promotion of endothelial cell proliferation and the physical organization of endothelial cells into tube-like structures. They promote angiogenesis, the growth of new blood vessels from the pre-existing vasculature. FGF1 and FGF2 are more potent angiogenic factors than vascular endothelial growth factor (VEGF) or platelet-derived growth factor (PGF).
FGF1 and FGF2 stimulate the proliferation of fibroblasts that give rise to granulation tissue [new connective tissue and tiny blood vessels] which fills up a wound space/cavity early in the wound-healing process. During the development of the central nervous system, FGFs play important roles in neural stem cell proliferation, neurogenesis, axon growth, and differentiation.”
Think of it this way. Insulin-like Growth Factors (IGF’s) are so powerful that they are considered to be PEDs (Performance Enhancing Drugs) in the athletic community, and due to their extreme anabolic (tissue building) nature, are thus banned. In many ways, FGF’s are even more potent than IGF’s.
As you can gather from the paragraph above, they promote a natural form of PRP, as well as the proliferation of collagen’s “tube-within-a-tube” structure (HERE). And on top of all this, they greatly enhance the body’s ability to build more blood vessels (angiogenesis), meaning there is more available OXYGEN available for tissue repair, regeneration, and healing.
The question now becomes, how can we naturally harness the power of FGF’s, not only for the professional athlete, but for the everyday Joe who has been injured and is living in CHRONIC PAIN? At least in theory, it’s easy. All we have to do is figure out what sort of treatments might cause FGF’s to be manufactured and released in injured cells.
There are any number of brand new studies showing that a wide array of exposures to various forms of electric fields as well as a number of the newer forms of electrical stimulation can stimulate fibroblastic activity and FGF’s. If you read 1985’s amazing Body Electric by the VA’s blacklisted researcher, Robert Becker (MD), you would know that this is nothing new. Likewise, there are a number of studies showing the benefit of LOW LEVEL LASER (both Cold and Class IV) on wound healing and fibroblastic activity.
There are also any number of chemical factors that stimulate fibroblastic activity; many of which are the chemical factors (cytokines, chemokines, interleukins, NO, etc) that are BROADLY CHARACTERIZED AS INFLAMMATION. This is why taking NSAIDS after a workout is counterproductive. It’s also important to remember that there are times when fibroblastic activity can be too strong.
For example, the August 2017 issue of the Journal of Physiology (Human Skeletal Muscle Fibroblasts Stimulate in vitro Myogenesis and in vivo Muscle Regeneration) revealed that, “Accumulation of skeletal muscle extracellular matrix is an unfavourable characteristic of many muscle diseases, muscle injury and sarcopenia.” In other words, there are situations where a PATHOLOGICAL “THICKENING” occurs in injured or diseased tissues. The authors state, however, that “it thus appears, in humans, that fibroblasts exert a strong positive regulatory influence on myogenic precursor cell activity, in line with observations during skeletal muscle regeneration.”
As you’ll soon see, there is a fine line between stimulating ECM (extracellular matrix) and cranking out too much ECM. What can be done to drive local (as opposed to systemic) fibroblastic activity in the person who has been injured and is living with either chronic pain or chronic dysfunction? That is the subject of today’s post.
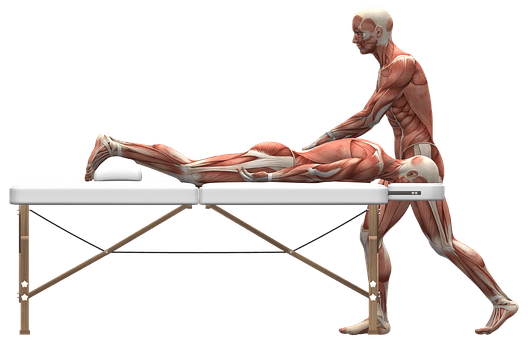
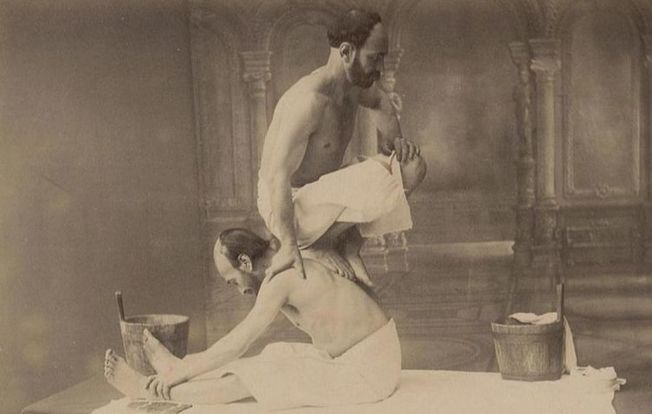
INTENSE BODYWORK: THE DRIVING FORCE IN FIBROBLASTIC ACTIVATION
When there is SCAR TISSUE (the medical name for this is “FIBROSIS“) or fasica that’s characterized as “DENSIFIED” present in the body, it has the potential to present a plethora problems. Many of you have been on the MEDICAL MERRY-GO-ROUND long enough to realize that another MRI or more PAIN PILLS, MUSCLE RELAXERS, NSAIDS, CORTICOSTEROID INJECTIONS, or other forms of “EVIDENCE-BASED MEDICINE” have not, and are not likely to solve your problem.
In fact, these things frequently make things worse because they have a tendency to both weaken connective tissues and cause increased epithelial permeability (THE LEAKIES), thereby increasing SYSTEMIC INFLAMMATION over time.
I mention Systemic Inflammation because it’s critical for you to understand the huge difference between it and Local Inflammation (HERE). In fact, as crazy as it may sound to you now, in many cases we are actually trying to cause local inflammation (HERE). The link reveals why breaking Scar Tissue sometimes has to be intense to get the desired result.
The cool thing is that not only do intense forms of body work (Tissue Remodeling in my office) help break the kind of adhesions found in FASCIA, TENDONS, LIGAMENTS, and MUSCLES, but it heavily promotes fibroblastic activity and proliferation as well. I’ve already shown you that this is a good thing, but as always, let’s dig a bit deeper.
It was Dr. Warren Hammer who stated that, “Mechanical loading is the crux of many methods of soft-tissue treatment.” Although he is certainly correct, this begs yet another question —- what exactly is mechanical loading (sometimes referred to as “TISSUE DEFORMATION” or HERE)? Fortunately, he answers this for us (quote is cherry picked from 2012’s Soft Tissue Treatment Is Another Form of Exercise).
“Mechanical loading is the principal way our body maintains itself, especially with regards to tendons, ligaments, bone, muscle and fascia. Lack of mechanical loading results in atrophy and eventual cell death. Years ago, anyone with acute lower back pain was sent to bed for a week. We now know that as soon as a patient can move with minimal discomfort, they should get out of bed and attempt the movement – i.e., mechanical loading.
The literature is replete with studies on mechanical loading and its resultant effects on the extracellular matrix (ECM), especially connective tissue and its collagen, tissue structure maintenance, release of growth factors, metabolic activity, protein synthesis, cell growth and survival, circulation, and gene expression. Mechanical forces that are crucial to the regulation of cell and tissue morphology and function could have both positive and negative effects (overuse, trauma, etc).”
Ten years ago as my family was returning from a day spent with friends on the CURRENT RIVER, we were hit by a drunk. Actually, I hit a drunk as he was in the process of running a stop sign that crossed the highway we were on (junction of M and Old 60) — HERE are some pics of the vehicle. My wife incurred a spiral fracture of her humerus (upper arm) that ran nearly the entire length of the bone. She was put in a “Traction Sling” (more like a few old rags tied together) with the only part touching her body, other than the part around her neck, being her wrist.
The purpose was to put enough mechanical stress on the bone to make it lengthen. The ortho said that if the bone healed “too long” there was no problem, as it would shorten on her own. However, if the bone healed “too short”, it would require some nasty surgeries to lengthen it. Enter Dr. Wolff.
One of the first things I learned about in physiology class was “Wolff’s Law”. Dr. Julian Wolff was a German physician (anatomy professor and surgeon) who, during the halcyon years of his career (the later portions of the 1800’s) noticed something interesting going on with bones. He realized that certain bones or areas of a bone that were mechanically stressed, grew thick and strong, while bones that were not stressed in a mechanical fashion, grew weak and brittle. Thus, Wolff’s Law was born; Bone adapts to the mechanical stresses put on it, whether said stresses are normal or abnormal.
This is how things like STRENGTH TRAINING and WHOLE BODY VIBRATION have the ability to actually improve bone quality and density (and yes, stimulate fibroblastic activity). It’s also how things like bone spurs, calcium deposits, and thin discs occur (DJD). Over time and with better technology, others figured out exactly how this occurs — via a process known as mechanotransduction.
Mechanotransduction is what we call the point where mechanical loads and forces are actually converted to electrical or chemical signals that the brain can understand. Although much of this has to do with PROPRIOCEPTION, there are actually receptors whose specific job is to detect the deformation of fluids and / or mineral crystals.
Due to changes in fluid pressures or deformation of crystalline structures, the body is able to convert the messages to something known as piezoelectricity, which is defined as, “electricity resulting from pressure.” Interestingly enough, a similar phenomenon to Wolff’s Law occurs in Soft Tissues, and goes by the name of Davis’ Law.
Dr. Henry Gassett Davis was a contemporary of Dr. Wolff. As a Yale-trained orthopedic surgeon, he began developing similar theories to Wolff that concerned connective tissues. Davis’ specialty was traction, and he developed numerous tractioning techniques for the orthopedic field, and in fact is considered the “father” of modern orthopedic traction. In 1867, his book, Conservative Surgery, carried this paragraph.
“Ligaments, or any soft tissue, when put under even a moderate degree of tension, if that tension is unremitting, will elongate by the addition of new material. On the contrary, when ligaments, or rather soft tissues, remain uninterruptedly in a loose or lax state, they will gradually shorten, as the effete material is removed, until they come to maintain the same relation to the bony structures with which they are united that they did before their shortening.
Nature never wastes her time and material in maintaining a muscle or ligament at its original length when the distance between their points of origin and insertion is for any considerable time, without interruption, shortened.”
Interestingly enough, this is the basis for the work of the brilliant (late) Chiropractor and Mathematician, Dr. Donald Harrison (HERE), and the technique he started; Chiropractic Biophysics (CBP). As science progresses, we are not only learning how important POSTURE is, but how important the PROPER CURVE IN THE NECK is as well.
In fact, it is this principle of Davis’ Law that has led me to believe that no matter how beneficial CHIROPRACTIC ADJUSTMENTS are, true spinal corrections are difficult to make without the application of some sort of continual mechanical stress (traction — HERE is an excellent example of this).
It is also the reason that huge numbers of adjustments given in a proverbial vacuum (without any form of mechanical tractioning (HERE and HERE are a couple more examples), are not only overkill, but not nearly as effective as they could be (HERE). In other words, even though people in my profession talk a lot about “maintenance,” what they are referring to is actually nothing of the kind (HERE).
The August, 2013 issue of the medical journal PLoS One (Electrical Stimulation Promotes Wound Healing by Enhancing Dermal Fibroblast Activity and Promoting Myofibroblast Transdifferentiation) used electrical stimulation to increase fibroblastic activity, which worked exceedingly well.
“It is well known that the endogenous electrical field (EF) in the human body plays several critical physiological roles, including the electrical activation of the nervous system and the muscles. During the skin wound healing process, fibroblasts, epithelial cells and endothelial cells are actively involved in extra cellular matrix production (ECM). In normal human tissue, fibroblasts contribute to tissue homeostasis by regulating the turnover of extracellular matrix (ECM).
Multiple strategies have been used to promote wound healing, including vacuum-assisted wound closure, shock-wave therapy, and local warming, to name a few. ES has been used as an adjunct to increase tissue blood flow and promote wound healing. This study demonstrated that constant ES… promoted skin fibroblast growth, enhanced cell migration, increased FGF-1 and FGF-2 production and induced fibroblasts to myofibroblasts transdifferentiation. It is also demonstrated that such modified cellular behaviors were inherited by the cells up to 3 days in culture. Our overall findings thus suggest the beneficial effect of ES on wound healing processes.”
While certainly cool, this is not really much different than Becker’s work back in the 1970’s. As a side note; the type of electrical stimulation they were doing is not the same as a TENS Unit or something similar. It’s also important to realize that stimulating Fibroblastic Activity does not mean simply CRANKING OUT MORE ECM, which happens to be the number one cause of death in the US.
There are any number of similar experiments using things other than electric current to accomplish the same thing. For instance, a 1997 issue of the International Journal of Biochemistry and Cell Biology showed that when you simply inject the fluid from wounded tissue into a tissue culture, the results, “demonstrate that the wound environment contains high molecular weight protein(s) that promote fibroblast functions, essential for the healing process.”
A year prior, the Journal of Investigative Dermatology showed that injecting the growth factors (GF’s), “like TGF-beta and CTGF can induce connective tissue cell proliferation and extracellular matrix synthesis.” Even Vitamin C has been shown to do this (1991’s Collagen Synthesis in Human Skin Fibroblasts is Stimulated by a Stable Form of Ascorbate, 2-O-oc-D-Glucopyranosyl-L Ascorbic Acid). But the grandaddy — the king of the hill when it comes to promoting fibroblastic activity —- is still the same. Mechanical stress helps create an environment that promotes healing.
In another of his articles, It’s the Fascia Stupid, Dr. Warren Hammer reveals that, “Fascial adhesions occur due to inflammation, immobility and micro-injuries caused by overloading.” And although he did not say it in this sentence, the most obvious reasons for FASCIAL ADHESIONS to occur is via trauma (CAR WRECKS, SPORTS, ABUSE, etc, etc) or REPETITIVE INJURIES. (my post called HOW DOES FASCIA TEAR?) Like wounds, tissue injury (consider it a “wound” on a cellular basis) causes fibroblastic activity. So; what if we could create an intense mechanical load on said tissue in order to promote healing? I’m already ahead of you. Let me show you a few examples of this from peer-review.
Back in our bicentennial year, the journal Science, revealed exactly what they were accomplishing via their study’s title (Cyclic Stretching Stimulates Synthesis of Matrix Components by Arterial Smooth Muscle Cells in Vitro).
“Rabbit aortic medial cells were grown on purified elastin [collagen] membranes, which were then subjected to repeated elongation and relaxation or to agitation without stretching. Cells remained attached to the membranes, and cyclic stretching resulted in a two- to fourfold increase in rates of collagen, hyaluronate [Hyaluronic Acid], and chondroitin 6-sulfate synthesis over those in agitated or stationary preparations. Synthesis of types I and III collagen was increased to the same degree. The model system devised to demonstrate these effects provides a means for relating various modes of mechanical stimulation to cell metabolism.”
Two years later, the journal Nature published a study (The Control of Cell Division by Tension or Diffusion) that showed something similar. “there is already much observational evidence that suggests that mechanical stress may lead to increased division. We provide experimental evidence that mechanical tension may stimulate the cell cycle in vertebrate cells.” In 1998, the Proceedings of the Institution of Mechanical Engineers published a study called Fibroblast Responses to Mechanical Forces, revealing that…
“The repair and maintenance of connective tissues is performed predominately by a mesenchymal cell known as a fibroblast. The activity of this cell is regulated, in part, by changes in the mechanical environment in which it resides. An in vitro model, the ‘culture force monitor’, and its derivative, the tensioning culture force monitor have been developed enabling quantitative investigations to be performed on fibroblasts in a collagen lattice. Application of a physiologically similar mechanical load has shown that fibroblasts change cellular morphology in a predictable manner and biochemically modify their resident environment.“
A study from this past February’s edition of Scientific Reports (Stretching Fibroblasts Remodels Fibronectin and Alters Cancer Cell Migration) showed similar things going on in CANCER PATIENTS.
“Most investigations of cancer-stroma interactions have focused on biochemical signaling effects, with much less attention being paid to biophysical factors [i.e, stretching, loads, and other things that cause mechanotransduction]. In this study, we investigated the role of mechanical stimuli on human prostatic fibroblasts….. Results show that mechanical stretching of normal tissue-associated fibroblasts (NAFs) alters the structure of secreted fibronectin [fibronectin binds extracellular matrix components such as collagen].
Unstretched NAFs deposit and assemble fibronectin in a random, mesh-like arrangement [can you say “Scar Tissue”?], while stretched NAFs produce matrix with a more organized, linearly aligned structure.” T
his is why the mechanical loads created by stretching, exercise, etc, are critical for healing to occur.
The rubber met the road in last year’s study in BioMed Research International (Effects of Synergistic Massage and Physical Exercise on the Expression of Angiogenic Markers in Rat Tendons).
“Physical exercise and massage are regarded as key factors in regulating tendon structure. In this study, we attempted to define the impact of these two activities on rat tendons by using morphological and molecular techniques, determining the expression of VEGF-A, FGF-2, and CD34 in the tendons of rats subjected to 10 weeks of physical exercise (running) with massage of varied duration.
The group of rats that was trained and massaged during the entire study was characterized by the highest expression of these markers…. The results of this study could point to the synergistic impact of simultaneous massage and physical exercise on the expression of angiogenesis markers in rat tendons.”
I could almost have shown you the entire study (not to mention it’s extensive bibliography) but I will leave you with one more paragraph.
“On this basis, the increase in angiogenesis and fibroblast activity induced by mechanical stimulation (massage) of a tendon may be expected to prevent the transient tendency for its structure to weaken. This may decrease the development of lesions within tendons during their long-term overload in the course of running. The obtained results may point indirectly to a beneficial effect of massage conducted during long-term intense physical effort on tissue metabolism in the tendon.
Moreover, the increased metabolism in the tendons may exert a protective effect in situations where there is an increased risk of tendon damage from unfavorable structural alterations developing during long-term high-intensity physical effort, such as running. However, further studies on the molecular and structural levels are required to fully clarify the mechanisms behind the changes developing in tendon tissue subjected to massage in the course of strenuous physical effort.”
The truth is, I could go on almost indefinitely as there are more studies on this topic all the time. Mechanical stress, wound healing, STRETCHING, and EXERCISE are all known to increase vascularization (angiogeneis), the amount of the various growth factors (GF’s) being produced, the number of fibroblasts being produced, an increase in the amount of collagen being produced, the quality of the COLLAGEN being produced, the alignment of the collagen being produced, the quality of the HYALURONIC ACID, as well as any number of other factors.
The problem is, for many of you struggling with chronically adhesed fascia, putting the cart ahead of the horse (trying to do heavy strength training before breaking said adhesion) simply does not work, and in many cases can act to tighten the knot instead of loosening it (HERE).
As you can see from THIS POST, my goal has been to create a unified treatment protocol that includes remodeling Scar Tissue, Fascial Adhesion, Tendinosis, and LOCALIZED FIBROSIS. There are always going to be those who simply cannot tolerate any degree of intensity in their manual treatment. For the most part, these are folks whose pain has become, or is becoming, CENTRALIZED (the allodynia / hyperalgia that I talk about at length on my site). But for many of you, you can’t really know if your pain has become “Central Sensitization” without at least trying (HERE).
When you add it altogether, it’s why SOLVING SOFT TISSUE INJURIES can often be equated to PLAYING CARNIVAL GAMES. To see a few of our VIDEO TESTIMONIALS, click the link. And if you know people who need to hear this message, FACEBOOK is a great way to reach them.
