Addressing Densified or Thickened Fascia to Address Chronic Pain
Although I have been discussing THICKENED FASCIA on my site for at least 15 years (oftentimes referred to by the scientific community as fascia that has undergone a process of “DENSIFICATION“) there is some very cool new research on the subject. Studies that not only verify the “thickened fascia” hypothesis, but could arguably help you both identify and start to address your CHRONIC PAIN issues if they are related to thickened fascia, which so many painful situations are.
While this does not necessarily mean that you can take care of the FIBROSIS and MICROSCOPIC SCAR TISSUE that’s already there (it’s likely that someone will have to do that for you), how amazing would it be if you were able to halt future thickening and the vicious cycles of pain and degeneration it perpetuates?
Before we delve into the research, I want to take just a moment to review the differences between normal fascia and thickened fascia or what I often times refer to as “FASCIAL ADHESIONS“.
The Differences Between Normal and Thickened Fascia
But your new shoes are worn at the heels
And your suntan does rapidly peel
And your wise men don’t know how it feels
to be thick… as a brick. – Jethro Tull from 1972’s Thick as a Brick
For those of you who have been treating patients via various forms of bodywork for a very long time, you already know this information. At least intuitively. In other words, you don’t necessarily have to understand all the latest science or jargon to know what you have been feeling during your years (or decades) of providing treatment to people who are chronically ill, chronically stressed out, or living with pain. Or in far too many cases, all of the above.
THICKENED FASCIA IS, WELL, THICK:
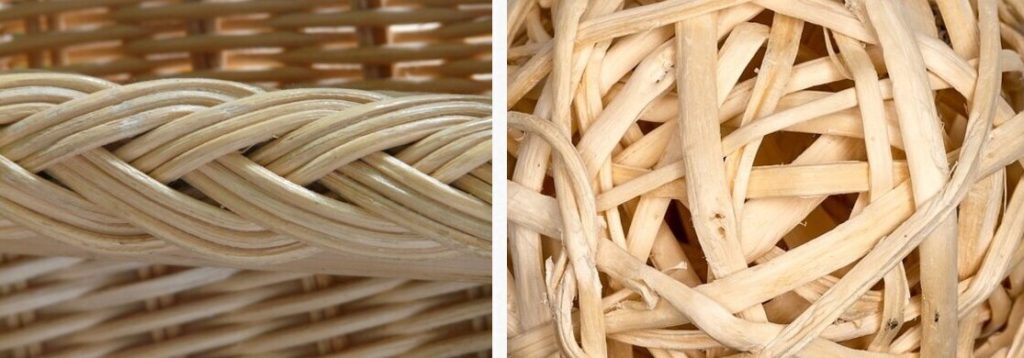
Yeah, I get it. Extremely redundant — a tautology if you will. But it bears repeating. Within the scientific / research portion of the medical community they often use the descriptive term, “densification,” to illustrate what’s going on at the cellular level. Think of it like a piece of paper that’s been crumpled into a ball instead of a nice, flat sheet. In a few areas of the body, and especially in the THORACOLUMBAR FASCIA of younger people (especially athletes), the fascia should actually be thicker. Just remember, however, that in most cases, thicker is not better. Thickened fascia causes problems, including….
THICKENED FASCIA IS LESS ELASTIC:
One of the aspects of fascia that makes it truly amazing in a biomechanical sense is the fact that it is both very strong and very elastic. In most cases (see previous point) a thickened fascia or other connective tissue means that it cannot stretch and elast the way it was created and designed to do. This means that in the case of thickened fascia, whatever the cause of said thickening, there is a strong tendency toward diminished movement. Restriction.
While this protective mechanism can certainly be helpful in the case of acute injuries; in the case of chronic, repetitive injuries, it is not only detrimental, it can literally be catastrophic as far as pain and dysfunction is concerned. Thickened fascia is not only less elastic but……
THICKENED FASCIA IS WEAK:
This is where we can get a vicious cycle churning. It’s really a no-brainer. If thickened fascia is weaker it means that it will always be…..
THICKENED FASCIA IS MORE PRONE TO INJURY OR RE-INJURY:
I speak with the voice of experience here. Not simply from my years of treating patients but because as I will show you in a moment concerning my ankle, it’s an inescapable fact of life that once you have injured a joint — any joint — it will always be easier to injure it again. And again. And again. Yes, there are things you can and must do to slow down this process.
But the fact remains that even though it is quite possible to make HUGE DIFFERENCES IN PATIENT’S PAIN LEVELS, it is impossible to get soft tissues back to their original strength and elasticity. Even after seemingly minor injuries. This is why you will sometimes hear the old time docs say, “Johnnie; you’d have been better off breaking the leg than tearing those ligaments!” But it does not stop there…..
THICKENED FASCIA CAN BE INCREDIBLY PAIN-SENSITIVE:
I am fascinated by the work of Chan Gunn, the medical neurologist from Vancouver who did a great deal of pioneering research on scar tissue 25 or so years ago. His ultimate conclusion as far as chronic pain is concerned? Scary stuff to say the least.
According to Dr. Gunn, scar tissue has the propensity to develop abnormally large numbers of immature nerve-buds post-injury — sort of like the hundreds of small twigs you sometimes see sprouting from the cut branches of topped trees. This phenomenon has the potential to make scar tissue over (over) 1,000 times more pain-sensitive than normal tissue (HERE). Now add in the fact that FASCIA ITSELF CAN ACT AS A NERVOUS SYSTEM and you can see a train wreck in the making.
Current Research on Causes of Thickened Fascia

First, there are lots of rather boring studies dealing with the fact that as we age we tend to get stiffer. Age-related Changes in Mechanical Properties of Human Abdominal Fascia from the May 2020 issue of Medical Bioengineering & Computing is one such study that I will spend five seconds on just to make a point. The authors stated…
The purpose of this study is to assess and model age-related changes in the mechanical properties of human fascia. The samples were divided into three age groups: group A, up to 60 years, group B, 61-80 years, and group C, 81-90 years. A uniaxial tensile test was applied to fascia specimens cut perpendicular and parallel to fibers. The secant modulus at 5% strain, the maximum stress, and the stretch at maximum stress were calculated from the stress-stretch ratio curves. The results indicated an increase in the secant modulus with the increased age. The trend is clearer in the longitudinal direction.
First, “secant modulus of elasticity” is from physics and is a way of measuring elasticity. Second, the results were exactly what we would expect; as people got older (or at least as the samples came from older deceased people) they tended to get less elastic, less flexible, and less stretchy.
And lastly, here is the problem with the hundreds upon hundreds of similar studies — they are done “in vitro” meaning outside of their normal biological context (as opposed to the opposite — “in vivo” or ‘in life’). The difference is huge. How is a cadaver or tissue sample going to approximate what is going on in a living organism? Correct. It cannot, which is always the major limitation of cadaver studies. However…..
Although there are plenty of ways to test flexibility and RANGE OF MOTION, what might be a way to test for thickened fascia in in a living subject — a method we touched on in my previous post (THE THORACOLUMBAR FASCIA, NON-SPECIFIC BACK PAIN & NEW IMAGING TECHNOLOGIES)? Can anyone say ‘ultrasound’?
DIAGNOSTIC ULTRASOUND (do not confuse it with the ultrasound machines that some chiros and therapists still treat with) is not only inexpensive and non-invasive, research is showing that it has not been used to even remotely near it’s capacity to image injured or “thickened” fascia. Speaking of thickened fascia, the January 2019 issue of Journal of Anatomy (Fascia Thickness, Aging and Flexibility: is there an Association?) dealt with this very issue in a study by renowned fascia researchers, Wilke and Stecco.
In a study considered the first of its kind, the authors took healthy subjects, both young (early 20’s) and old (70ish), and then took a lot of measurements. Using ultrasound they compared the thickness of various areas of fascia to the range of motion of particular areas / joints. Before we discuss conclusions, listen to what these authors said about ROM. “Range of motion (ROM), the maximal distance over which a joint can be moved, represents a significant hallmark of musculoskeletal health….” Furthermore, these ranges of motion are determined by “international guidelines“.
Why do I bring this up? Because I do not see ranges of motion being checked any more (and when they are, THEY OFTEN PROVIDE EXTREMELY DECEPTIVE RESULTS). Allow me to give you an example of the former.
I had a woman almost the exact age as me (mid-fifties) in the office this week. I had seen her ten years ago for long-standing HEADACHES and NECK PAIN that no one else had been able to help her with. After a decade her headaches and neck pain were back so she decided to come see me again. The range of motion of her neck was literally between a quarter and a third of normal. In other words, it was grossly deficient. Dangerously deficient. This is despite just having just had her YEARLY PHYSICAL EXAMINATION (not her OB/GY “ANNUAL”).
Although it certainly does not surprise me that her neck ranges of motion were ignored (checking them takes all of 20 seconds if you are slow), considering that her doctor would have been should have been aware of this for a very long time, I have to shake my head.
The authors came to some interesting, but certainly not unanticipated conclusions. Here we go, in cherry-picked fashion.
Recent research has revealed an association between increased fascia thickness and reduced joint flexibility in patients with chronic pain. In addition to other factors (e.g. hydration status and contractile cell activity), the tensile stiffness of a tissue is dependent on its cross‐sectional area. A thicker fascia might, therefore, be associated with restricted ROM. Such a relationship has been found in neck patients. The present study aimed to investigate the possible association of fascia thickness and flexibility in a healthy population. As decreased flexibility and increased fascial stiffness have been reported in old individuals, the additional hypothesis was tested that older adults display a higher fascial thickness.
Systematic between‐group differences of fascia thickness and variable associations (i.e. fascia thickness and flexibility) were detected. Young adults exhibited higher fascia thickness of the anterior and posterior lower leg, anterior thigh and abdominal wall (+12.3–25.8%). Conversely, older participants showed higher thickness in the lumbar spine (+40.0–76.7%). Correlations of both body mass and fascia thickness, as well as flexibility and fascia thickness were found. Age‐related changes in fascia thickness may be a contributing factor of restrictions in joint range of motion. Further study delineating the cause–effect triangle of body mass index, flexibility and fascia thickness is necessary.
Remember this because in a moment I am going to show you how to leverage these conclusions so that you can help your cause in DIY fashion! Also realize that these authors finished by suggesting that ultrasound could easily and inexpensively be incorporated into examinations for the multitudes of you trying to cope with unrelenting pain. “In sum, fascia thickness may become a valuable outcome parameter in the prevention and treatment of musculoskeletal disorders, such as neck or back pain….” Unfortunately there is just too much money to be made using technology clinics already have in-house (MRI, x-ray, CT).
Sports Injuries Cause Thickened Fascia
In another Italian study involving the Steccos, this one from the February 2021 issue of Diagnostics (Ultrasound Imaging of Crural Fascia and Epimysial Fascia Thicknesses in Basketball Players with Previous Ankle Sprains Versus Healthy Subjects) we see much the same thing — that injured connective tissues, whether FASCIA, TENDONS or LIGAMENTS heal in a “thickened” manner. This study looked at basketball players with a history of recurrent ankle injuries (interesting to me because I am that person) as compared to age-matched healthy controls.
Fascial layers may play an important role in locomotor mechanics. Recent researches have revealed an association between increases of fascia thickness and reduced joint flexibility in patients with chronic pain. Ankle sprains are one of the most common injuries caused by physical activity during sports or activities of daily living, and usually happen during dynamic movement. Over 50% of all ankle injuries cause a ligament injury. When ankle injury occurs, the mechanical receptors in the joint become damaged, leading to functional instability.
The authors spent a lot of time talking about what “functional instability” looks like. Some of the things that were mentioned include loss of balance, loss of coordination, as well as chronic instability or a feeling of sagging, weakness or looseness in the joint, along with any number of others. They also talked about “DAMAGED MECHANICAL RECEPTORS“. When these receptors (mechanoreceptors) are damaged it leads to fouled up proprioception, which, if not dealt with properly, always leads to degenerative changes in the affected joint (bone spurs, calcium deposits, thinning cartilage joint space).
The biggest problem is not only that this process is a cycle that actually feeds itself, but it seems that few people are addressing these injuries properly to begin with (“chronic ankle instability mostly comes about due to an inappropriate treatment following an initial injury…“).
Although I am getting ahead of myself; after breaking my ankle the second of three times playing basketball (and of course tearing the associated ligaments along with the avulsions), I used a TRAMPOLINE for rehab. And after still ending up with chronic foot pain, found resolution in the hands of lower-body biomechanic expert, SHAWN ENO (the only person I am aware of who builds 100% custom orthotics specifically for those of us with crazy-high arches). Anyway, the authors concluded that…..
Study results confirm that ultrasound imaging is an important tool for assessing the fascial layers of the leg, providing excellent anatomical definition. The posterior compartment of crural fascia was thicker than the anterior compartment, probably due to a postural reason in both groups. Moreover, they showed an increase in thickness of the epimysial fascia in basketball players with previous ankle sprains.
Another study, this one from the October 2019 issue of the Exercises and Sports Science Review (Overuse Injury: The Result of Pathologically Altered Myofascial Force Transmission?) looked not at “traumatic” injuries but at “repetitive” injuries. What have I showed you in the past? Which one, all things equal, tends to be ‘worse’? OVERUSE — breaking the body down faster than it can recover and heal.
The authors specifically mention four (4) problems that make up as much as 90% of all sports injuries. PLANTAR FASCIITIS, TENDINOPATHY / TENDINOSIS, ITB-SYNDROME, and STRESS FRACTURES (I guess that this is an appropriate place to discuss stress fractures considering that Levin has made the case that BONE IS CALCIFIED FASCIA). I feel they should have included PATELLO-FEMORAL SYNDROME here as well.
There are two things that make this study particularly relevant to both athletes and non-athletes alike, beyond the fact that work can cause many of the same type of repetitive injuries as sports. The first is that according to these authors, a whopping 4 out of 10 athletes complain of “musculoskeletal pain of unclear origin” every year month (gulp) week. Secondly, the author correctly “argue that the location of symptoms, which is often the site of treatment, may represent an area of compensation rather than the origin of an overuse pathology.”
This is something I am not only reminded of every day in practice, but something that increasing numbers of studies are proving out. Speaking of studies, the authors of this one point out four distinct pathways that subsequent “thickening” and / or “stiffness” discussed in the quote below can occur. These can “act separately or in concert“.
Myofascial force transmission may lead to an overuse pathology. At first, a local stiffness increase can originate from different causes: muscle contraction in hypertonicity transmits radial stress to the fascia and tensions specific parts of it through direct fiber insertions. Chronic stress activates intrafascial myofibroblasts, and immobility induces changes in the water content of the connective tissue. If these processes are pronounced enough to sufficiently stiffen the soft tissue bridge to the neighboring structure, force is transferred, and over time, pain and dysfunction develop adjacently.
When we think of these sorts of injuries — overuse injuries — we almost always think along the lines of physical or mechanical stresses. But guess what. This team of researchers specifically mentioned stress as it relates to the autonomic nervous system. “Contraction of myofibroblasts… has been identified in numerous fascial tissues, and… is largely governed by the autonomic nervous system. Hence, if conditions that disturb the interplay between the sympathetic and parasympathetic nervous systems are present, myofascial stiffening may occur over time due to concerted cellular contraction.”
And while it is certainly possible for people to be dominant on the parasympathetic side of their autonomic system, the reality is that SYMPATHETIC DOMINANCE is almost ubiquitous in Western society.
When I read this study’s conclusions, it not only made me glad that I learned some of these concepts a very long time ago, but helps explain why therapies like BIG DONNIE THOMPSON’S MOTHER-IN-LAW METHOD can be so incredibly effective when used as a regular part of one’s post-workout regimen; similar to foam-rolling but arguably far more effective.
Therapists and health professionals should consider treating soft tissue structures adjacent to typical locations of overuse injury symptom manifestations if traditional local interventions have failed. Because of the structural linkage of the skeletal muscle via collagenous connective tissue [fascia], it is assumed that persisting local stiffness increases may over time affect neighboring and adjacent tissues.
In fact, for a variety of pathologies including plantar fasciitis, LBP, groin pain, ITB syndrome, and chronic shoulder pain, nonlocal abnormalities (altered mechanical tissue properties) distant to the area of symptom localization can be observed. Yet, there is a paucity of intervention studies examining the effectiveness of remote exercise in the treatment of these overuse injuries.
Thickened Fascia and Connective Tissues as Related to Consumption of Sugar / High Glycemic Carbohydrates
First, I have covered this previously IN DETAIL. But with our national per-capita sugar consumption continuing its upward trend (another 10% increase over the past few years), we will look briefly at new studies on the effects of consuming SUGAR & JUNK (HIGH GLYCEMIC) CARBS on connective tissues such as fascia. Before we get going on fascia itself, I want to quickly discuss two recent bone studies simply because of the increasingly popular hypothesis that bone is calcified fascia (see earlier link).
First realize that bone actually creates hormones “whose influence goes way beyond its own physiology” (Bone Regulation of Insulin Secretion and Glucose Homeostasis from last October’s issue of Endocrinology). Furthermore….
“The risk of fragility fracture increases for people with type 2 diabetes mellitus (T2DM), even after controlling for bone mineral density, body mass index, visual impairment, and falls…. In summary, worsening glycemic control was associated with… degraded macroscale skeletal integrity. These data are the first evidence of progressive alteration of bone tissue composition with worsening glycemic control in humans.”
In other words, blood sugar dysregulation is going to affect bones. How does it cause thickened fascia?
Although sugar is both HIGHLY ACIDIC and HIGHLY INFLAMMATORY, it is its propensity to result in AGES (Advanced Glycation Endproducts) that’s the biggest culprit in the thickening and subsequent stiffening of connective tissues. The June 2019 issue of the Journal of Medical Ultrasound (Sonographic Evaluation of the Achilles Tendon and Plantar Fascia of Type 2 Diabetics) helped confirm this yet again with these conclusions. After comparing the relative thicknesses of the tendons in both diabetics and non-diabetics that were matched for both age and sex, the authors concluded (I included quite a bit here, even though it is cherry-picked)….
Diabetes mellitus (DM) is an endocrine disease with a prevalence of 5.1% worldwide… Diabetic neuropathy occurs in 50% of individuals with long-standing DM. Plantar ulcers are characterized by the triad of neuropathy, infection, and ischemia; also known complications of DM. The global incidence of DM foot is estimated to be 15%, and 12%–24% of individuals with diabetic foot ulcers require amputation. Amputation risks in diabetic patients are about 15–40 times higher than in nondiabetic patients, and the risk of lower extremity amputation increases by a factor of 8 once an ulcer develops.
DM predisposes to plantar fasciopathy, a disorder characterized by thickened plantar fascia (PF), and loss of the normal organized fascial architecture. PF is one of those tissues that may change their physiology and biomechanical function in the presence of chronic hyperglycemia. Studies have revealed that the PF actively contributes to influence the pressure acting on the metatarsal heads.
The pathophysiology of the plantar fascia and Achilles tendon in DM can be summarized as running the following course: sustained hyperglycemia promotes increased glycosylation of proteins, resulting in accumulation of “advanced glycosylation end products” in patient’s soft tissue and in thickening and vascularization of the affected tissues. Increased Achilles tendon thickness and plantar fascia thickning in DM have been considered an expression of soft-tissue damages.
Among the diabetics, 46.3% had normal BMI, 32.4% were overweight, and 21.3% were obese. The Achilles tendon and plantar fascia of diabetics are significantly thicker [than non-diabetics]. The presence of diabetic neuropathy worsens the thickness of the Achilles and plantar fascia among diabetics. BMI is significantly related to thickening of the Achilles and plantar fascia among apparently healthy controls but not in diabetics.
What sticks out to me most is not the conclusion itself (we all expected it), but the fact that almost 50% of all the diabetics had a ‘normal BMI‘. In other words, darn near half of all the diabetics in this study were not fat — or at least did not appear so to the casual observer.
What this does is slam us in the face with the concept of “skinny fat” or something known in the medical community as MONW (Medically Obese, Normal Weight). These are the individuals who do not look at all overweight… Until you see them in minimal clothing or draw blood. Instead of having blood markers in line with their bathroom scale is telling them, they appear to be obese — something I am seeing with great regularity in my clinic, similar to increasingly seeing high school kids diagnosed with T2D (I recently saw my first 8th grader who had been diagnosed). As you can guess, this bodes poorly for future muscluloskeletal health and one’s ability to exert oneself.
This month’s issue of Endocrinology, Diabetes and Metabolism (Fibro-proliferative Disorders and Diabetes: Understanding the Pathophysiologic Relationship Between Peyronie’s Disease, Dupuytren Disease and Diabetes) hit us over the head with this relationship yet again — the relationship between blood sugar dysregulation and thickening of connective tissues.
In this case, the relationship is to “Peyronie’s disease and Dupuytren disease, fibroproliferative disorders of the tunica albuginea of the penis and fascia of the hand, respectively.” When we see the term “fibro-proliferative,” we must realize that the world’s #1 leading cause of death, FIBROSIS, is ‘proliferating’. In other words, there is a pathological increase of something known as the ECM or Extracellular Matrix.
Fibrosis in people with diabetes can affect almost every organ in the body, including the heart, eyes, liver, kidney, skin and vascular system. Many people with diabetes have arthropathies, such as thickened skin and limited mobility of the joints of the hands and fingers, leading to flexion contracture(s). Endocrinologists may overlook limited joint mobility in people with diabetes or may not consider it a diabetes‐related complication.Chronic hyperglycaemia due to diabetes mellitus can also lead to tissue injury and fibrosis. A meta‐analysis has shown a relationship between Dupuytren disease and diabetes.
So, beyond some sort of LOW CARB APPROACH TO EATING (I’m a fan of a PALEO/KETO MASHUP), the question in everyone’s mind should be whether or not bodywork has the potential to successfully address the thickening and increased density that occurs in damaged soft tissues, whatever the cause.
Bodywork and Its Potential Effects on Thickened Fascia
OK. We are finally down to rubber-meets-the-road time. Thickened fascia and other connective tissues really are a thing, but the question on everyone’s mind is, “What can be done about them?” Scratch that. Multitudes of people already know that bodywork is incredibly helpful in the war against thickening and densification. Let’s look at what peer-review says concerning this topic. Not because I (or any of you other bodyworkers reading this) somehow need a pat on the back, but it’s always nice to see that science is proving out what we do.
Let’s spend some time dissecting a study from the Journal of Bodywork and Movement Therapies (Evaluation of Hyaluronan Content in Areas of Densification Compared to Adjacent Areas of Fascia). But before we do, I want to take a few moments to discuss Hyaluronan or Hyaluronic Acid (HA).
Hyaluronan was discovered in 1934, and less than a decade later people were trying to use it commercially — as an egg substitute (the whites) in COMMERCIAL BAKING APPLICATIONS. Interestingly, HA would remind you of egg whites, only much slicker and less sticky. So it’s not surprising that it has been in use since the early 1990’s as a NATURAL SUBSTANCE THAT BECAME A PATENTED “DRUG” made from rooster combs (many companies have their own ‘patented’ version) — the shots people have injected into their knees trying to stave off REPLACEMENTS for a year or two (or in some cases, maybe more).
Great stuff (especially when compared to CORTICOSTEROID INJECTIONS), but…. If insurance companies are going to pay big bucks for HA injections, they should be paying for stem cell. Also realize that there are untold numbers of HA supplements on the market, mostly to improve joint function / arthritis pain and as beauty aids (skin, hair and nails). But I regress.
Let’s get back to our study and see why discussing hyaluronan is of importance.
Epimysial fascia is a type of deep fascia that ensheaths muscles and helps to define their shape and structure. It is continuous with the tendon, allowing it to transmit forces. There are three layers… and between each layer is areolar connective tissue rich in hyaluronan. HA is a polysaccharide in the extracellular matrix that provides both lubrication and resistance to compression. Under normal physiological conditions, HA is responsible for normal gliding motion between components of fascia, muscle, nerves, lymphatics and blood vessels.
No wonder HA is popular. But the question remains as to whether or not there is hard evidence of how it is affected (or affects) thickened fascia and other connective tissues (notice how it is “continuous with the tendon“). Connective tissues are rich in HA, which allows the moving parts glide smoothly and effortlessly on each other. This study shows how too much of a good thing can become a bad thing.
Thickened fascia and densified connective tissues actually contain increased amounts of HA, leading to molecular clumping, which in turn leads to a change (thickening) in the consistency of the fluid lubricant. As you might suspect, this has potential to cause both dysfunction and pain.
Let’s slightly shift gears again.
Back in 2004 the patriarch of the Italian family renowned for fascia research and treatment (Luigi Stecco) published a book (Fascial Manipulation for Musculoskeletal Pain) in which he discussed a structure / phenomenon he coined as “Centers for Coordination”. These points, usually distant from the pain (remember what we saw earlier), correspond to convergences of tension found in normally functioning fascia.
Stecco taught that these centers (there are 14 of them just as I believe there are 14 muscle meridians in Meyer’s ANATOMY TRAINS) are, according to his method of treatment, the prime site(s) for treatment. How important are these Centers of Coordination in the Stecco Method? Basically they are everything.
They are the points of muscle convergence, where movement actually originates. They also correspond to areas where muscle becomes tendon. They are also said to help regulate the ways that muscles “pennate” or slightly change their line of pull so that they have better mechanical advantage.
Stecco taught that if the fascia around the muscle spindle (found in the ENDOMYSIUM) does not glide well, sensory nerves become inflamed and irritated, which will always reflex back to the motor side of the equation. Repeat cycle. Furthermore, Stecco taught that while not the same as, these Centers of Coordination are related to both TRIGGER POINTS and acupuncture points.
This is why Stecco taught that most of the musculoskeletal pain people have is caused by fascia rather than coming from the joint itself. The idea of Centers of Coordination begins to make sense once you start to realize that pain does not always follow nerves but instead tends to be seen in the body’s motor control pattern sequencing, or the loss thereof. With this as our background, back to the study.
Changes in concentration and molecular structure of HA in Centers of Coordination result in a restriction of gliding termed “densifications”. When subjected to increased stresses involving mechanical, pH or temperature changes, HA polymerizes to form long-chain molecules and becomes more viscous. Polymerized HA is thought to provide increased structural protection to myofibrils undergoing stress by creating a densification at Centers of Control.
While this entanglement of HA protects the myofibrils, it restricts the glide and normal motion, creating dysfunction. There are both myelinated and non-myelinated nerve fibers distributed throughout the deep fascia which may become sensitized during dysfunctional motion of fascia and contribute to a variety of myofascial pain syndromes.
Let’s unpack this paragraph. First, things like pH (think about how acidic the S.A.D is), heat/friction, and mechanical dysfunction cause the body to undergo a protective mechanism. In the same way that calcium deposits and bone spurs are a negative effect of WOLFF’S LAW, so likewise is thickened fascia. The result is pain and abnormalities in motion / movement patterns brought on by the fact that the nerves themselves can become “embedded” in this densified, fibrotic, microscopically disorganized mess of “thickened fascia“.
We call these ENTRAPMENT NEUROPATHIES and the more of them I treat, the greater my realization of why ADJUSTMENTS, THERAPY and STRETCHING are, in many cases, useless in addressing them. At least without addressing the thickened fascia first.
In this experiment, the authors looked at samples of cadaver fascia taken from a specific lower extremity Center of Coordination known as La-Cx, and compared the way that the thickened fascia from the sample took certain stains to the way that surrounding tissues took the same stains (the stains attached themselves to the “polymerized” HA that’s one of the hallmarks of thickened fascia).
The differences were remarkable and easy to see under the microscope. While the study certainly had its share of limitations (after all, it was a cadaver study) and does not “prove” anything about bodywork being able to resolve thickened fascia or other thickened / densified connective tissues, it shows that there is a very distinct difference between such tissues. Which brings me to the finale….
Resolution of Pain and Dysfunction Caused by Thickened Fascia

Are you ready to step out of the box that is standardized medical care? For many of you, it’s your only hope. That would be only as in “only“. Not only are the drugs not working, but I could provide you with examples of each and every one of the BIG FIVE actually causing the very problems they are supposed to be solving. Corticosteroids are the most obvious as they actually deteriorate / degenerate collagen-based tissues (virtually all of the tissues that make up joints). Due to time constraints I will leave you with one other; THE UGLY RELATIONSHIP BETWEEN PRESCRIPTION DRUGS AND DEPRESSION.
I’m not suggesting for one moment that you abandon your doctor or whatever medical care you are currently undergoing or receiving. I am suggesting that you research everything (that would be everything as in ‘everything‘) that they tell you or suggest you do; that would include me as well.
The nice thing for my readers is that I have created a DIY SOLUTIONS FOR CHRONIC PAIN / CHRONIC ILLNESS PAGE that has the potential to help most of you reading this significantly. And if you have friends or loved ones swimming in this sea of pain, be sure to turn them on to our FACEBOOK PAGE, where all of my posts eventually end up.
