When I suggest to patients that they should be “hanging,” it immediately conjures up images of the Old West for some of them. This is not the sort of hanging we are going to discuss today! Today I want to show you that there are some truly amazing benefits of hanging (axial traction) that go far beyond simple pain relief, into the realm of helping to actually restore joint function and integrity.
I’ve previously shown you the amazing benefits of INVERSION TABLES — something I am constantly promoting even though I have never sold them. What you must remember, however, is that inversion tables are really designed to target the LUMBAR SPINE (low back). So, even though some of you might get relief from MID-BACK / RIB ISSUES or even CHRONIC NECK PAIN, with inversion, this is not going to be the case for the majority of you. For those of you with neck pain there are a wide array of both simple devices (over-the-door-neck-traction and the DAKOTA DEVICE are two of them) that benefit a significant number of people at a reasonable cost.
So; knowing how beneficial axial traction (stretching the body length-wise) can be for both neck and low back issues, the question we need to be asking is if there is anything that works similarly for the upper spine and shoulders?
The good news is that not only is there something out there that has potential to help those dealing with the LOWER NECK / UPPER BACK (the part of the spine that can cause numbness, tingling, and other “paresthesias” in the upper extremities), but in many cases can provide huge benefit to people with shoulder problems. Let me explain why.
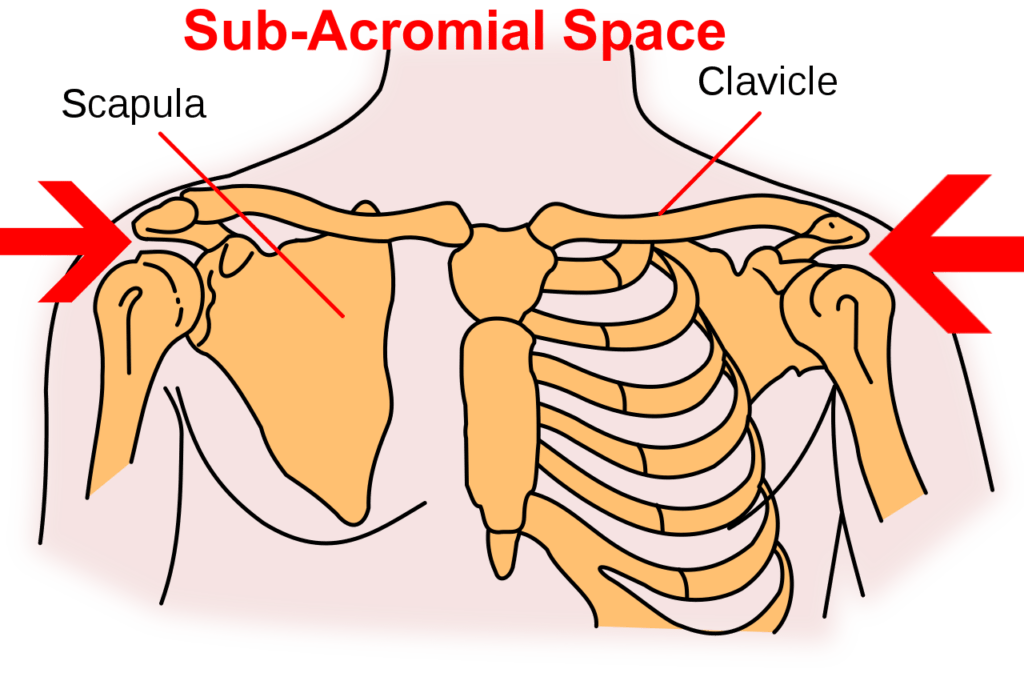
If you feel your shoulder blade you will notice a ridge that runs diagonally upwards towards the shoulder. This is called the “spine” of the scapula and at the distal end (the end farthest away from the center of the body), it turns into a funky-looking contraption called the ACROMION PROCESS. I’ve mentioned the Acromion Process in the past when I showed you what a shoulder separation is (an AC-Separation or ACROMIO-CLAVICULAR SEPARATION). As would make sense, the “sub-acromial space” is the space that lies under the acromion and on top of the humeral head (the ball of the shoulder). Pics below.
It’s also important to realize that the majority (about 85%) of the population have ‘bent’ or even ‘hooked’ acromions (HERE), meaning these people are starting out at somewhat of a disadvantage, with their anatomy being skewed toward shoulder impingement from the start, which we will discuss at length in a moment.
In order to understand the importance / benefit of hanging, we first need to understand a bit of anatomy. Specifically, we need to know who lives in the sub-acromial space. So, let’s first take a look at a few simple anatomical diagrams showing the acromion process as well as the space underneath.
The Benefits of Hanging: An Anatomical & Physiological Basis
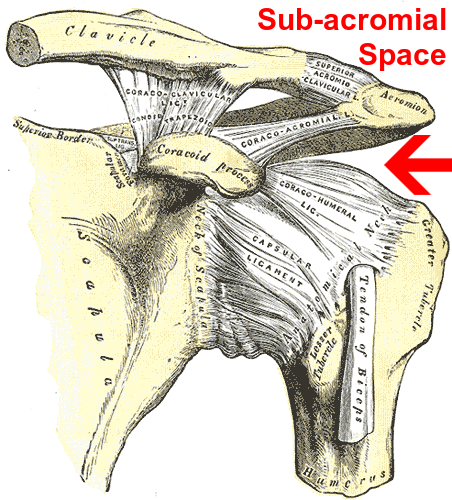
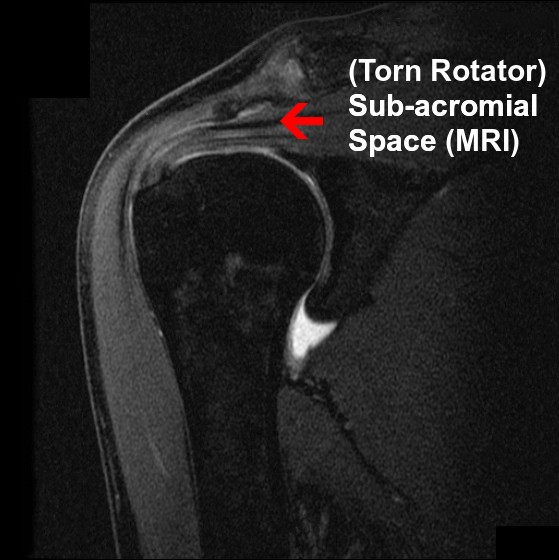
Before we address what is meant by “degenerative changes” in the header above, let’s get back to answering the question, ‘who lives in the sub-acromial space?‘ It’s the abode of three main structures; the TENDON OF THE LONG HEAD OF THE BICEPS, the SUB-ACROMIAL BURSA (the biggest bursa in the body — HERE is a post discussing the difference between these two problems), and several ROTATOR CUFF TENDONS (particularly that of the SUPRASPINATUS, the one of the four that is most-frequently injured or damaged — 95% of the time it’s the culprit). There are also a couple of very important LIGAMENTS that reside in the SAS.
Knowing what you know now, it should not surprise you to learn that the most common diagnosis or reason given for shoulder pain (between 50-70% depending on whose research you feel is most accurate) is something known as sub-acromial impingement. Because little has changed in the past two decades concerning SHOULDER IMPINGEMENT, take a peek at the abstract of a 2003 study from the Journal of Biomechanics (Anatomical and Biomechanical Mechanisms of Subacromial Impingement Syndrome).
Subacromial impingement syndrome is the most common disorder of the shoulder, resulting in functional loss and disability in the patients that it affects. This musculoskeletal disorder affects the structures of the subacromial space, which are the tendons of the rotator cuff and the subacromial bursa. Subacromial impingement syndrome appears to result from a variety of factors. Evidence exists to support the presence of the anatomical factors of inflammation of the tendons and bursa, degeneration of the tendons, weak or dysfunctional rotator cuff musculature, weak or dysfunctional scapular musculature, posterior glenohumeral capsule tightness, postural dysfunctions of the spinal column and scapula and bony or soft tissue abnormalities of the borders of the subacromial outlet. These entities may lead to or cause dysfunctional glenohumeral and scapulothoracic movement patterns. These various mechanisms, singularly or in combination may cause subacromial impingement syndrome.
First, we learn that this problem is common — dog common. Second, it is a major cause of TENDINOSIS (often mistaken for tendinitis) of both the biceps and rotator cuff muscles. Third, much of grief associated with impingelent is based on “INFLAMMATION,” which means that there are lifestyle changes that can be undertaken to help address it. Fourth, thanks to our tech-based sedentary society, underlying factors such as “muscular weakness / tightness” and “postural dysfunctions of the spinal column” are not going away any time soon. And lastly, the authors mention degenerative changes.
When we speak of skeletal degeneration, we are talking about three major categories; bone spurs & calcium deposits, thinning joint spaces, and destruction of articular cartilage or disc. I should probably throw in one more — THICKENING. This thickening is not only something that happens to bone, but also commonly occurs in connective tissues such as ligaments, tendons, and even FASCIA (sometimes the scientific community refers to this as “DENSIFICATION“). Remember, all three of these tissues reside in and around the sub-acromial space.
What’s very interesting is that a number of studies showed that this thickening is to a large degree considered a “normal” finding in athletes and those using their shoulders intensely — even at very young ages. Furthermore, these changes did not correlate well to symptoms even though they are often associated with varying degrees of diminished sub-acromial space. I am not surprised and though I will not re-hash the topic here, suffice it to say that this is the very reason I stopped taking x-rays in my clinic a decade ago, and why I warn people to temper their expectations when getting an MRI or CT (HERE).
While there are any number of exercises and stretches that physical therapists, chiros, AT’s, etc will utilize to help take pressure off the structures in the sub-acromial space, the medical community’s standbys never seem to change — meds (THE BIG FIVE) and surgery (arthroscopic acromioplasty / decompression — shaving, trimming and grinding away thickened, calcified or degenerative structures).
While the surgery is typically “effective” (most sources claim around 80% efficacy), realize that full recovery is going to take the better part of a year, with the first month or three being extremely difficult and painful. There was also evidence that as many as 1 in 5 are left with persistent shoulder pain, and the same number were shown to have an increased propensity for frozen shoulder syndrome (adhesive capsulitis). Whether this is the result of the surgery or simply something that the surgery was unable to solve, probably depends on the individual case.
For those of you who can’t afford to be off work for several months (or simply do not want to have surgery), what sort of DIY alternatives can be done at home and without great expense or large segments of time blocked off for said rehab? Even though we are not going to discuss them today here, I would suggest you head over to YouTube as there are many many videos pertaining to shoulder impingement exercises and stretches. Today we are going to discuss one of the simplest and increasingly popular forms of shoulder rehab — hanging.
Benefits of Hanging on Degenerative Changes that Occur at the Shoulder and Sub-Acromial Space
Hanging is one of those things that sounds ridiculously simple — almost too good to be true. This is because the majority of the people who follow Dr. K’s protocol, no matter how weak or messed up they are as far as their shoulders and arms are concerned, are going to see positive results.
A few years ago a good friend of mine, an MD with a world-wide FUNCTIONAL MEDICINE clinic, sent me a little paperback book by orthopedic surgeon, Dr John Kirsch. The book, A SMALL PAPERBACK, is called Shoulder Pain? The Solutions and Prevention. All I can say is that this little book is a gold mine if you struggle with CHRONIC SHOULDER PAIN.
From his decades of experience doing bone and joint surgery, Dr. Kirsch realized that for any number of reasons, not only do people develop “degenerative changes” in their shoulders, but the acromion process actually changes as well. For reasons discussed but not completely understood, over time the acromion actually drops and/or curves downward, causing diminished sub-acromial space.
Dr. Kirsch has used studies with advanced imaging to show that grabbing onto something overhead and hanging increases this space by using the humeral head as a lever. To see just how effective this simple modality is, read the comments in HIS SHORT VIDEO. How does hanging work and why have more doctors not promoted it?
As to the second question, since when does the fact that something works mean that the medical community is going to promote it? For the most part, they promote things that they can do for you, as opposed to EMPOWERING YOU to find solutions and resolve your situation(s) on your own. As I mentioned earlier, drugs and surgery. As to the first question, it works because of something known as Wolff’s Law.
This easy-to-understand principle is based on the fact that even though it does not happen overnight, bone is an adaptable, dynamic and moldable / maleble tissue. Discovered by Dr. Wolff back in the mid-1800’s, his law states that bone will grow or remodel itself according to mechanical stresses placed on it, whether these stresses are normal or abnormal. It’s how traction casts work. It’s the principle that orthodontists use to straighten teeth. It’s also why people develop thickening or spurs at points of extreme (abnormal) biomechanical stress.
Dr. Kirch, using dynamic MRI, put the shoulder under axial traction and imaged it, realizing that not only was he not causing impingement as has been the standard mantra for decades, but that if he could direct a superiorward pressure for a long enough time, he could actually change the physical shape and appearance of the acromion process. Thus, using the head of the humerus to push the acromion upwards can actually, given a bit of time, “lift” the acromion off of the impinged structures and help restore the diminished sub-acromial space.
MY BROTHER used it to dramatically improve a shoulder problem he had dealt with for the better part of thirty years, and I have had numerous patients use it to great effect and benefit, in several cases avoiding surgery in the process.
Russ’s Rules for Hanging
Before I get started, I want to first say that I am not going into any real detail here — purchase Dr. K’s short book. Last I saw it was a measly ten bucks. I also suggest that as with all forms of self-therapy, make sure your doctor determines that you are physically able. Finally, this is not meant to diagnose or treat shoulder conditions, but is simply a formula I personally follow and have promoted to many patients who I thought met the criteria. Start slow and easy and build from there.
WHERE YOU SHOULD HANG: While this seems quite easy for many readers, some of you will have to figure out where to hang. There are any number of devices that can be purchased online, which are designed for this very purpose (chin-up bars that fit in doorways are one example). Or you can rig something up yourself. Or maybe even hang from a tree branch in your yard. The possibilities are endless (I have one patient who grabs the edge of the treads on his open stairway). Just make sure that what you do is safe (re-read this sentence before continuing).
HOW LONG YOU SHOULD HANG: The beauty of hanging is that for most people, little time is required. A few minutes a day. And it need not be done all at once. If all you can manage at first is 10 seconds; beautiful! It’s a starting point. Realize, however, that the longer you hang, the more you are putting Dr. Wolff to work for you! On the other hand, don’t proceed so fast that you cause yourself great distress (pain).
WHAT IF I CAN’T HANG? Not strong enough? Can’t get your arm(s) over your shoulder / overhead? You don’t have to hang your entire body-weight to achieve great benefits. Again, read the book and start very slowly. As a side note, I use “weight lifting wrist hooks” because my grip gives out before my shoulders (you do the search as I do not want to give Amazon more business than they already have).
TISSUE REMODELING FIRST: While this is certainly not a hard and fast rule (many of you will do fine without), many of you will find it difficult to hang simply because of the amount of SCAR TISSUE / FIBROSIS surrounding the shoulder. HERE is an example of why seeing me first might be in your best interest.
For more information on this topic, see my post on SHOULDER IMPINGEMENT. If you are interested in seeing a very cool (and short) shoulder testimonial, HERE IT IS. And for those of you looking for something more than simple pain relief, I created a protocol for addressing a wide variety of chronic conditions (found on THIS POST). Oh; and if you know someone with shoulder problems who might possibly benefit, be sure to get the information in front of them. FACEBOOK is still a good way to accomplish this!

One Response
I have been hanging for about 2 weeks now, I was diagnosed with shoulder impingment a few months ago, and about 6 months, I had a slight tear in my rotator cuff. I hve built up to doing about a 90 second hang, and can do 10 sets of 30 seconds. How long should it take before I can feel results. I have a lot of impingment signs still, when moving wrong. Also for about the last 4 months, I have been having tightness in my neck, with a cracking noise. Can the two(shoulder and neck) be related. And I am patiently waiting for shoulder impingment to end, and I am hoping that my neck will feel better as well. People who know little about hanging are trying to tell me to see a PT, but I am trying to avoid the expense. any suggestions or Ideas would be greatly appreciated. the tightness in neck and upper traps are on the same side of the shoulder injury. thanks a lot.