Centralized Pain or Not? Why Understanding Chronic Pain and Central Sensitization is Critical in Your Personal Battle with Pain
“For society, the costs are staggering: low back pain is the leading cause of years lost to disability and chronic pain costs billions of dollars through health system expenditures, productivity losses, reduced quality of life, and informal care. Thinking on chronic pain needs to be reset. Patients need reassurance that they will be believed, respected, and supported, and not blamed if a treatment does not work.
Chronic pain is real. It deserves to be taken more seriously The Lancet Series on chronic pain debunks a common misconception of chronic pain as an indicator of ongoing injury, requiring suspension of activity. Instead, chronic pain is often a product of abnormal neural signalling….” CHERRY-PICKED from a study being mentioned today
Nearly 25 years ago “Sally,” a young mother of three, was minding her own business, when a patrol car on the way to a call T-boned her in the driver side at a high rate of speed, essentially destroying her life in the process. She recently headed back home after spending a life-altering week in our Mountain View, Missouri clinic (LOOK FOR HER TESTIMONIAL IN A COUPLE WEEKS — BTW Sally, you are an amazing woman!). Without getting into the nitty-gritty details of her case, part of the quote above, from the latest issue of the renowned medical journal The Lancet (Rethinking Chronic Pain), reminded me of our time together.
One of the recurring themes of my CHRONIC PAIN PATIENTS is that not only are they not believed, but instead treated like scam-artists and / or drug-seekers (or maybe hypochondriacs), who are either crazy or seeking financial gain. Her trip to the world-famous Mayo Clinic provided a prime example. Instead of actually taking time to do a thorough examination (there were LOTS OF HIGH TECH TESTS AND IMAGING THAT REVEAL NOTHING ABOUT THE STATE OF ONE’S FASCIA), she was told she was OBESE, OLD and unwilling to address her POOR POSTURE.
Not only were these not even remotely true (she is fit, young and her posture was surprisingly good), her experience is an ugly example of one of the most common ploys in all of medicine. Instead of saying, “Wow, I’m not really sure what’s going on here,” the opposite happened. As the quote from the top of the page indicates is standard practice, she was blamed when the treatment (DRUGS, SURGERY, and THERAPY) did not work. It’s all your fault you rotten faker!
After reviewing her history, I told Sally, when she decided to come see me, that my ability to help her hinged on answering the question posed at the end of the same quote — whether or not she had “abnormal neural signalling“. It is a question that cannot be fully answered until after I treat a chronic pain patient, and possibly not even then. But let’s back up and answer the question, what is abnormal neural signaling?
Abnormal neural signaling is a simple descriptor for a phenomenon known as CENTRAL SENSITIZATION — people having pain in the absence of visible / tangible tissue or nerve damage. A brand new study from the Journal of Pain Research (Peripheral and Central Pathological Mechanisms of Chronic Low Back Pain: A Narrative Review) helps us understand what happens when pain becomes centralized.
After mentioning various common reasons for CHRONIC LOW BACK PAIN that is not centralized (DISC DEGENERATION, VERTEBRAL DEGENERATION, FACET DEGENERATION, DEGENERATION OF THE THORACOLUMBAR FASCIA, as well as CHRONIC SYSTEMIC INFLAMMATION) the authors began their discussion of the “central pathological mechanism of chronic low back pain“. The ten Chinese authors / researchers summarized this concept thusly….
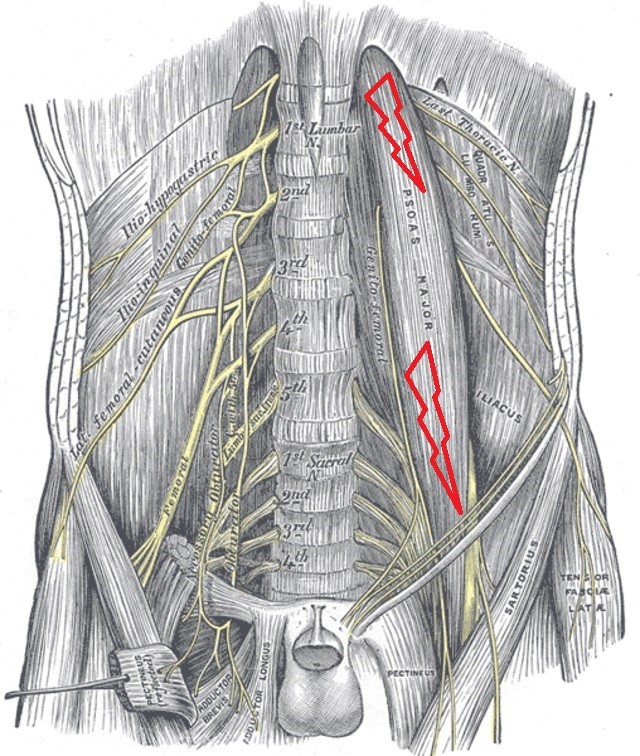
Recent evidence suggests that the nociceptive mechanism of central sensitization, including neuronal hyperactivity in the central nervous system may contribute to the persistent pain in chronic low back pain, in the absence of noxious stimuli. Based on an epidemiology study, there was a high concentration of trigger points in the psoas muscle of chronic low back pain patients, relative to those without chronic low back pain.
Moreover, it was shown that prolonged nociceptive input from trigger points can alter brain plasticity and drive the development and maintenance of chronic musculoskeletal pain. Therefore, central pathological changes may be an important factor in the pathogenesis of chronic low back pain.
Although it is not totally and 100% accurate, when you see the word “nociception” think of pain. Thus, what’s happening is that a ramped up or ‘hyperactive‘ nervous system (can anyone say SYMPATHETIC DOMINANCE?) is actually altering brain function to the point that pain occurs even in the absence of ‘noxious stimuli‘ (the thousands of chemical mediators we collectively refer to as INFLAMMATORY OR INFLAMMATION).
While all of this is certainly interesting, it’s not really new or novel. What is new (at least new to me) was learning that the neurological input from CHRONIC TRIGGER POINTS themselves (which we are still not completely sure about what causes them) have the potential to alter neurological function of the brain to the point of chronic pain and Central Sensitization.
Trigger Points, Chronic Pain and Central Sensitization
“Myofascial pain syndrome (MPS) is a type of skeletal pain identified by myofascial trigger points (MTrPs). The formation of MTrPs is linked to muscle damage. The fibroblast growth factor receptor (FGFR1) has been found to cause pain sensitivity while repairing tissue damage.” From the abstract of a June 2020 study (Peripheral FGFR1 Regulates Myofascial Pain in Rats via the PI3K/AKT Pathway) in Neuroscience
“Tension-type headaches (TTH) are a very common condition. The most recent theories on TTH occurrences suggest that a myofascial component, through trigger points (TP), gives rise to pain signals from the periphery to the central nervous system (CNS). This nociception could lead to CNS sensitization and headaches. Studies show that identification and treatment of TP is a valid therapeutic option for TTH.” From the March 2020 issue of the Swiss Medical Review (Myofascial Approach in Tension-type Headache Management: A Scientific Assessment)
“Two concurrent visceral pains from internal organs sharing at least part of their central sensory projection can give rise to viscero-visceral hyperalgesia, i.e., enhancement of typical pain symptoms from both districts. Visceral pain, headache and musculoskeletal pains (myofascial pain from trigger points, joint pain) can enhance pain and hyperalgesia from fibromyalgia. Myofascial pain from trigger points can perpetuate pain symptoms from visceral pain conditions and trigger migraine attacks when located in the referred pain area from an internal organ or in cervico-facial areas, respectively.” From the November 2019 issue of The Journal of Neural Transmission (Co-occurrence of Pain Syndromes)
“Muscle TrPs are associated with both sensory and motor symptoms. For instance, active and latent TrP areas exhibit altered chemical milieus as compared to non-TrP areas. These local biochemical changes, including increased availability of pro-inflammatory substances such as substance P, IL-1β and tumor necrosis factor (TNF)-α, activate muscle nociceptors potentially contributing to peripheral mechanisms by sensitizing nociceptive nerve endings.
Other studies have reported that TrPs also sensitize non-nociceptive large-diameter myelinated afferents nerve endings. Importantly, and many times ignored by several clinicians, TrPs also contribute to motor impairments including altered muscle activation patterns, accelerated muscle fatigability, or increased co-antagonist activation.” From the June 2019 copy of the Journal of Pain Research (Trigger Point Dry Needling for the Treatment of Myofascial Pain Syndrome: Current Perspectives within a Pain Neuroscience Paradigm)
“Widespread pressure pain hypersensitivity was associated with duration of health history conditions, suggesting that long-lasting health complaints may act as a triggering/perpetuating factor, driving sensitization in individuals with chronic neck pain.” From the June 2019 issue of Oxford Pain Medicine (Widespread Pressure Pain Hypersensitivity, Health History, and Trigger Points in Patients with Chronic Neck Pain: A Preliminary Study)
Allow me to break down and summarize these quotes into a few simple paragraphs.
Pain, TYPE II (not chronic ‘centralized’ pain at this point), whether from musculoskeletal sources (that would include FASCIA) or visceral / organ sources, can sensitize sensory nerve endings, lowering their threshold to fire. In other words, in the presence of certain chemical mediators it takes very little stimulus (sometimes no stimulus) to create pain impulses. One of the myriad of sensitizing chemicals is the growth factor that heals damaged FIBROBLASTS (cells that manufacture fibrous connective tissue) in trigger points. Also mentioned specifically were chronic inflammation and some of the chemicals associated with it (“Substance–P, IL-1β and tumor necrosis factor (TNF)-α“).
This sets up a vicious cycle where the inflammation-sensitized nerve endings can cause trigger points, but also where the trigger points can likewise cause inflammation via their healing process. And not only is this entire process related to CHRONIC ILLNESSES / CONDITIONS, but related in a linear fashion to duration of said illness or condition. In other words, the longer you’ve had (insert disease of choice here — THYROID ISSUES, DEPRESSION, DIABETES, HEART PROBLEMS, etc etc etc) the greater the chance of developing a brain-based pain syndrome characterized by “abnormal neural signalling” (Central Sensitization).
And lastly, we see that this process not only effects the sensory side of the nervous system, it affects the motor side as well — something that is clearly seen in THIS SHORT SERIES OF ANIMATIONS on the origins of chronic trigger points. What does this do? It perpetuates trigger points to other parts of the body via chemical mediators but also via BIOMECHANICALLY COMPENSATORY (ABERRANT) PATTERNS OF MOVEMENT AND TENSION. And while it is clear that chronic trigger points can be found almost anywhere, what I notice from research is that they are most likely to be found in the base of the HEAD / SKULL, the UPPER BACK & NECK, and FACE (TMJ).
Let’s go one step further while looking at the link between chronic pain and central sensitization as pertaining to chronic trigger points….
What I’ve noticed after thirty years in practice and the last twenty being immersed in TISSUE REMODELING for DENSIFIED, THICKENED, or FIBROTIC fascia (FASCIAL ADHESIONS and the microscopic scar tissue associated with), is that while trigger points are certainly not uncommon (especially the dreaded levator trigger point, which I would argue is the most common of all TP’s — see upper back link above), they are not remotely as common as fascial adhesions. Again, in the people I see on a day to day basis, fascial adhesions are infinitely more common than trigger points.
Why is this important to know? Because with a serious myofascial trigger point issue, at least you have something visible / tangible to show for it — the painful and palpable knots of muscle. With the far more common ‘fascial adhesion,’ there is usually nothing to show for it besides pain. Scratch that; you must look for the appropriate down-stream symptoms if you hope to help those with chronic pain due to fascial adhesions from becoming ‘centrally sensitized’ (i.e, not only help those who are Type II Pain solve their pain, but prevent them from becoming Type III).
In plain English this means that even though fascial adhesions will not image with currently used standard testing (the testing that insurance companies actually pay for), it is extremely easy to find simply by looking for the clues of its presence. The number one clue? Easy; RESTRICTED RANGES OF MOTION — particularly in the cervical spine (neck) and SHOULDER GIRDLE.
However, because this post is looking at a study pertaining to chronic low back pain, the same phenomenon seen in the neck are true for the low back as well (go back and look at my link on the thoracolumbar fascia or look at THIS VERY SHORT POST that will clarify what I am saying via two 10 second videos).
Chronic Pain and Central Sensitization: Back to Today’s Study

“Between 80% and 90% of low back pain patients complain of non-specific low back pain. Based on several ongoing investigations on the pathological mechanism(s) of chronic low back pain, few aspects of this disease are known. For instance, most lumbar spine structures may serve as the potential origin of pain. This includes the sensory innervation in the intervertebral disc (IVD), facet joints, muscles, tendons, ligaments, fascia, synovium, joint capsule, etc. Moreover, lumbar pain can be brought on by factors such as inflammation, degeneration, or injury.”
If you struggle with any kind of chronic pain issue, this paragraph is of critical importance because we could substitute the NECK, SHOULDER, KNEE, etc, etc, for the low back and basically still be accurate and honest. For example, I stopped taking x-rays a decade ago because I came to this conclusion independently of current research (research that is now considered “current,” although it was much more controversial then) — that it is all but impossible to correlate patient’s spinal x-ray findings to their complaints in the vast majority of cases.
Thus, the fact that the experts (not me, I’m the class dunce with my nose in the corner) continue to say that (gulp) 90% OF ALL LOW BACK PAIN IS NON-SPECIFIC. In other words, the cause of low back pain is rarely able to be determined even if you RUN EVERY TEST IN THE BOOK. It’s why I have heard more than one MD admit in candid personal conversations, “don’t bother getting an MRI until you are ready for surgery”. Why? Dr James Andrews famous in-house study says it all as he inadvertently spills the beans on his profession (HERE).
The study’s authors went on to discuss the way that chronic systemic inflammation actually causes epithelial barriers to start leaking, causing alterations of the blood-brain barrier (A PHENOMENON THAT AFFECTS ANY NUMBER OF OTHER ORGANS, AND THAT I REFER TO AS “THE LEAKIES”), which leads to GLIAL CELL / MICROGLIAL ACTIVATION affecting attacking the brain itself. Honestly, if you are a chronic pain sufferer, particularly one who struggles with chronic low back pain, I would strongly suggest you at least read this study as it’s free online.
Finally, the authors provided an absolutely shocking conclusion to these findings. If you are dealing with chronic low back pain, you need to be about the business of addressing it because if it goes on for just a single year, your chances of Central Sensitization explode.
“Moreover, once the chronic low back pain or late persistent low back pain brain characteristics develop, they remain stable and unchanged for the next 10 years. This study suggests that the brain forms a state of chronic pain within the first year of low back pain. Therefore, the first year is a critical period for brain alterations in back pain patients. Moreover, this period remains consistent with the clinical definition of the transition of standard pain to chronic pain and is assumed to be between 3 and 12 months.”
In other words, once you make that transition from Type II Pain to Type III Pain, all bets are off. Why? Because once the pain is locked into the brain (not “in your head” pain that is psychosomatic, but locked into your brain’s circuitry and playing on a continuous loop), actually resolving this situation is one heck of a challenge. Which brings me to my final point. Don’t despair if you’ve had your pain a very long time. Do not automatically assume your pain is Type III or Centralized.
Although I routinely see Type II patients that have had their pain for decades (HERE, HERE, HERE, HERE, HERE and HERE are examples), I actually find Type III Pain to be fairly rare in the chronic pain community that I treat; possibly because I try to weed out Type III patients before they come see me (HERE, HERE and HERE are more examples of long-term Type II Pain that never became Type III).
Don’t take this sort of verbiage (“weeding out“) personally; I simply do not want to take advantage of people that I do not believe I have a legitimate shot at helping (ALTHOUGH I COULD EASILY DO IT IF I WANTED TO THE TUNE OF MILLIONS OF DOLLARS A YEAR). However, realize that in many cases (think “Sally” here) if I am not really sure whether they have “centralized” their pain yet, I simply give them the choice (HERE).
Endless adjustments are not needed; Rest assured, you will be able to tell in a treatment whether or not this approach will be beneficial. Just look at our TESTIMONIAL PAGE to see that this is true. Furthermore, whether Type II or Type III pain, your free gifts (plural) from me are first, A POST ON SOLVING CHRONIC BACK PAIN IN DIY FASHION, and secondly, A POST ON SUCCESSFULLY ADDRESSING CHRONIC PAIN AND CHRONIC CONDITIONS.
If you are not willing to step outside the box containing little else besides THE BIG FIVE and surgical solutions (this includes RFA and other similar), forget about it. Speaking of outside of the box solutions, here is one I thought I would mention to my readers simply because it was brought to my attention by a long-term patient just the other day.
New Solutions for Chronic Low Back Pain: Spinal Stem Cell Therapy

I do want to briefly mention one more option that might intrigue some of you — stem cell therapy. Semi-retired Poplar Bluff orthopedic surgeon, Dr. Gene Hansborogh (father of the TYLER HANSBOROUGH) has been doing stem cell therapy from various local clinics for quite some time. However, he does not work on the spine.
A patient of mine who was decimated with chronic low back pain and chronic severe spinal degeneration told me just Friday about her experience with the BLUETAIL MEDICAL GROUP in St. Louis (bluetail, as in the skink lizards we see around here that can regrow their tails). Her results were not only amazing but occurred within 72 hours. BTW, they used her own stem cells taken from what she described as her hip / buttock area. Definitely something to at least contemplate prior to surgical intervention.
If you are wanting to reach the people you love and value most with incredible and potentially life altering information about preventing or at least addressing chronic pain and central sensitization, liking, sharing or following on FACEBOOK is a great way to make sure they at least get a peek.

One Response
wow, I’ve really seen myself and my issues in reading two of your pieces about chronic pain!!/ at age 86, I’m gradually starting to feel better -fibromyalgia-= joint pain- knees ++ other stuff /what I do when I get those ambient pain stabbings=I just pinch that pain spot if it is coming from no where i.e. no injury or fall or specific reason/ guess what/ very often the pain doesn’t return to the spot I pinched/ such as my legs or even toes )gout)/ crazy but the advice to look within when trying to heal is great advice!! thank you so much/ SE please do not publish my name or e-mail/ p.s. I remembered how my Italian grandmother used to pinch me if I was getting on her nerves so I applied her remedy to my own pain /who knows but I’m feeling better/ am doing a lot with my diet, meditation, avoiding all of the stress and crazy scenes going on now/ STRESS always has been my biggest trigger!!