Does Pain Cause Problems in Fascia, or Do Problems in Fascia Cause Pain?
“You might attribute a painful neck or a backache to tired muscles or stiff joints. But these symptoms can also be caused by a part of your body you probably haven’t heard of: the fascia. Although fascia looks like one sheet of tissue, it’s actually made up of multiple layers with liquid in between called hyaluronan. Healthy fascia is smooth, slippery and flexible. It’s designed to stretch as you move.
But there are certain things that cause fascia to thicken and become sticky. Fascia can become gummy and crinkled up (called adhesion). When it dries up and tightens around muscles, it can limit mobility and cause painful knots to develop.” From Johns Hopkins article, Muscle Pain: It May Actually Be Your Fascia
It’s an old cliche; an argument as old as, well, time itself. Which came first, the chicken or the egg? Although we won’t tackle the PHILOSOPHICAL & THEOLOGICAL IMPLICATIONS of this question today, that debate sounds suspiciously familiar to the title of today’s post. Is your pain due to problems in your fascia, or are the problems in your fascia the result of your pain (ASSUMING THE INTIMATE RELATIONSHIP BETWEEN PAIN AND INFLAMMATION IS ACCURATE)?
I’ve argued previously that according to many experts, FASCIA is not only the most abundant connective tissue in the body, it’s the most pain-sensitive as well. Throw in the fact that it does not image well with standardized testing like MRI, and it can make for a long, miserable day. Add to it that scarring in fascia can make the tissue more than a thousand times more sensitive than normal tissue (HERE), and life can feel downright depressing if you are on the wrong end of this equation.
We will deal more with fascia as we move through this discussion but for now I want to talk about pain. What is pain, what causes pain, and what can possibly done (NON-PHARMACEUTICALLY) to address it successfully? The first thing to understand is that when it comes to pain, it is not all alike.
The Three Types of Pain
- TYPE I PAIN: In Type I pain, the nervous system is working properly and there is no tissue damage present. You bump your knee on a desk, say “ouch,” and shortly thereafter have forgotten about it because it no longer hurts. There are no residuals with this kind of injury, which happens to us all day long.
- TYPE II PAIN: With Type II pain, the nervous system is working properly, but there is at least some degree of tissue damage present. This damage can take many forms. It could be from an acute injury or re-injury (say an ANKLE SPRAIN or a WHIPLASH ACCIDENT or maybe even a SPORTS INJURY). It can also arise from the accumulated damage of old, chronic injuries — the ankle sprain, whiplash, or sports injury that you had 20 years ago, WHICH HAVE BECOME DEGENERATIVE. The problem with Type II pain is that a much too large number of these people advance to……
- TYPE III PAIN: Big problems here. There may or may not be tissue damage present but as far as your pain, it only matters slightly. This is because your brain is perceiving pain even in the absence of tissue damage. Type III pain can take on many forms, including hyperalgia and allodynia (HERE for a complete explanation), as well as full-blown CENTRAL SENSITIZATION.
How Does Inflammation Fit Into this Fasica / Pain Puzzle?
Inflammation is one of the single most misunderstood phenomenon in all of medicine. And although it is not itself “swelling,” it can cause swelling by attracting fluid to it. Inflammation is a large group of chemicals made by your immune system (white blood cells), when activated by tissue damage or foreign invaders.
And while I am not going to go into all the different mechanisms here (we might come back and discuss some of them later), please realize that the metabolic by-products of certain foods have the potential to actually create massive amounts of these inflammatory mediators as well (some of the mechanisms of diet-induced inflammation include AGES, LEAKIES, certain ‘bad news’ FATTY ACIDS, etc). If you want to know more about inflammation, simply take a look at THIS POST.
Fascia, Pain and Inflammation: Putting the Puzzle Together

“Myofascial pain is probably one of the least understood and most frequently misdiagnosed types of pain. It is also one of the most common sources of pain in our population and results in a large number of doctor visits, missed work days, and missed social activities. The word “myofascial” means related to muscle and fascia. Fascia is the connective tissue which surrounds the muscles in the body. So myofascial pain means pain that is coming from muscles and connective tissues.” From the Michigan Headache & Neurological Institute’s article, What is Myofascial Pain?
What is chronic myofascial pain? Chronic myofascial pain, also called myofascial pain syndrome, is a painful condition that affects the muscles and the sheath of the tissue — called the fascia — that surround the muscles. Chronic myofascial pain can involve a single muscle or a group of muscles. In general, the outlook is good for people with chronic myofascial pain. When properly diagnosed and treated, the pain often can be controlled. From Cleveland Clinic’s article on Chronic Myofascial Pain
Low back pain (LBP) is a major health issue for both women and men. The lifetime prevalence for the general population in most industrialised countries ranges from 60% to 85%. By definition non-specific or idiopathic LBP is characterised by the absence of a specific spinal pathology and is considered the commonest form of LBP. There are indications that the lumbodorsal fascia [thoracolumbar fascia] as well as paraspinal muscles embedded in this fascia (erector spinae muscles) are a contributing factor in the pathogenesis and progression of LBP.
Fascia is not only essential for balancing and transferring forces among muscles but functions as a body-wide mechanosensitive signalling network. This in turn makes it a key player in mechanotransduction, allowing cells such as fibroblasts to perceive and react to mechanical stimuli. Moreover, fascial neuroplasticity — the interplay between fascia, skeletal muscle, and the nervous system — is increasingly being recognised in scientific exploration with regard to musculoskeletal dysfunction such as LBP syndromes. From one of the two studies being discussed at the end of today’s post.
The pathophysiology of myofascial pain is not well understood. Psychological stress, muscle tension, and physical factors, such as poor posture, can cause a latent trigger points to become active. Current research supports sensitization of low-threshold, mechanosensitive afferents associated with dysfunctional motor endplates in the area of the trigger points projecting to sensitized dorsal horn neurons in the spinal cord.
Pain referred from trigger points, as well as latent trigger points, may be mediated through the spinal cord after stimulation of a sensitive locus. In a study by Alonso-Blanco et al, a connection was found in women between the number of active myofascial trigger points and the intensity of the spontaneous pain and widespread mechanical hypersensitivity; nociceptive inputs from these myofascial trigger points may be linked to central sensitization. From Dr. Jennifer Finley’s March 2019 article for MedScape, What is the Pathophysiology of Myofascial Pain?
Breaking down Dr. Findley’s quote to something that can be understood by the general public is a good place to start as far as figuring out the relationship between pain, inflammation and FIBROTIC FASCIA (scar tissue or fascial adhesion) is concerned.
First, as with almost all biochemical physiology, our understanding of precise / exact mechanisms is limited and constantly changing. While this probably doesn’t mean that our treatment approach is wrong (in this case, using bodywork or asking patients to change their diets or lifestyles), it simply means that from time to time we need to re-evaluate the model that we carry around in our minds.
Secondly, look at what can cause latent TRIGGER POINTS to become “active” (the same could be said of FASCIAL ADHESIONS, although as the link reveals, they are two different but intimately related problems). “Psychological stress“. Can anyone say SYMPATHETIC DOMINANCE? I know I beat this drum rather often and rather loudly but it amazes me how many people not only discount this phenomenon, but also discount the amazingly easy ways to address it naturally, without ANTIDEPRESSANTS and ANXIETY MEDS (as well as the class of drugs known as HYPNOTICS, which, for over a decade was the number one class of prescription drug in America).
Findley mentioned muscle tension as well (THINK TENSION HEADACHES HERE as well as any number of others), which is intimately related to injuries of all sorts (CHRONIC OR ACUTE) as well as a problem that computers, phones and stress have made almost ubiquitous in America; CRAPPY POSTURE (this is doubly triplely quadruplely true for anyone who struggles with chronic and severe UPPER BACK / SHOULDER PAIN). Likewise, this “projecting to the dorsal horn of the spinal cord” (the area that senses pain), raises the odds of developing Central Sensitization.
What inflammation does is lowers the amount of stimulus required for pain receptors to meet the threshold for the brain to say, ‘ouch; this is painful‘. The result is that stimuli that should not cause pain, do; and stimuli that should cause a ‘little’ pain, causes a lot (see Type III Pain, allodynia and hyperalgia).
I have seen plenty of research, including from the famous Italian family of fascia researchers (the Steccos) saying that MECHANORECEPTORS (the nerves that sense stretch, position and movement, allowing for something called proprioception — very (very) abundant in fascia) can actually become sensitized to the point they become nociceptors (pain receptors). And here’s where things can potentially slide into free fall.
Fascia, Fibrosis, and Pain: The 30:1 Nerve Ratio
Clear back in the early 90’s I was attending a Whiplash Conference taught by one of my profession’s most brilliant and academically well-rounded leaders (Dr. Dan Murphy), where he presented some almost mind-bending research, the results of which, when combined with what we’ve just discussed, has the potential to wreak havoc on anyone who has lost mobility or joint / tissue function for any number of reasons.
First, recall that one of the most common reasons for diminished mobility is “THICKENED” FASCIA. When fascia is ‘embarrassed‘ (a medical word meaning something ‘bad’ has happened to it), it thickens, tangles, twists and essentially “TETHERS” itself in a manner which both causes restriction and prevents NORMAL RANGES OF MOTION.
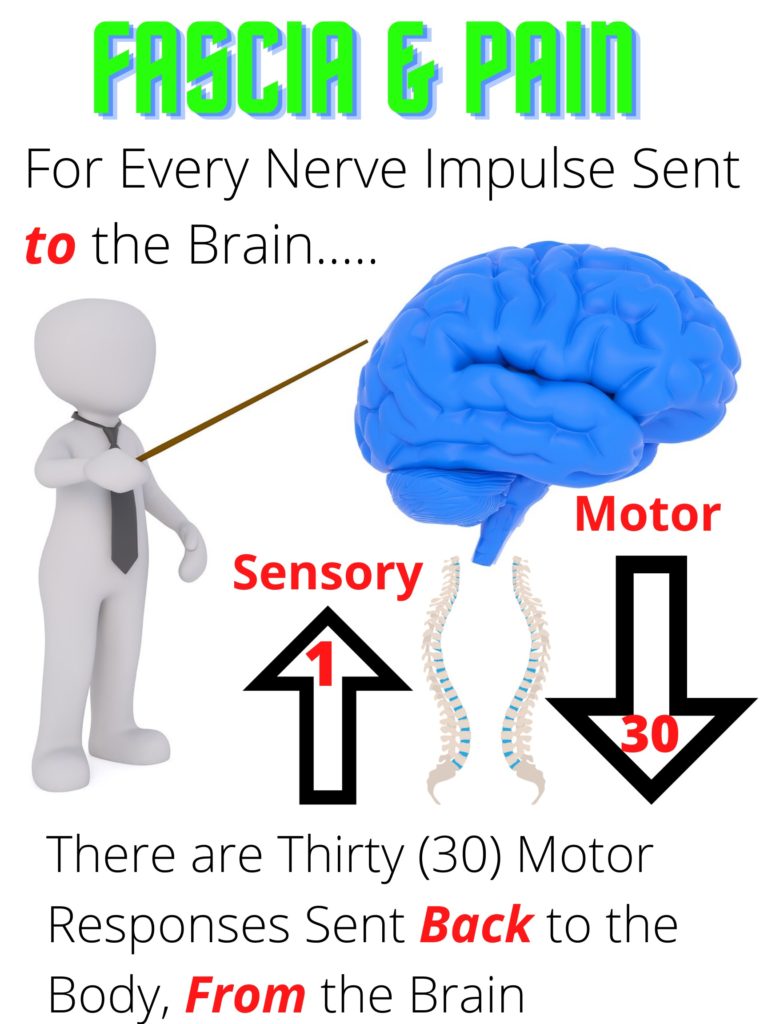
According to Dr. Murphy, who backs everything he says or teaches with studies (plural); for every nerve impulse that goes up to the brain (sensory or afferent responses, THINK PROPRIOCEPTION HERE, not just nociception / pain), the result should be that a gate of sorts is opened, allowing thirty motor responses (efferent responses) to return back from the brain to the body, allowing it to function normally.
Re-read that again so that you really understand it.
These are the impulses that control every single function of your body, both mechanical and chemical. What this means in English is that when tissues or joints don’t function properly, (the latter is true WHETHER SEGMENTAL OR SECTIONAL motion is affected, although they are certainly not the same) the result is a subtle or not so subtle loss of neurological function of muscles, glands, tissues, organs, etc, etc…. And pain.
The endgame is that some people will wind up with pain — in some cases, severe pain — that seemingly has no cause. Or at least not the obvious cause(s) that the medical community equates with pain. This means that if you don’t have a “reason” for your pain, you are quite likely to be labeled a hypochondriac or drug-seeker. Or simply told you have FIBROMYALGIA, whether it’s accurate or not. For some people, however, the resultant “endgame” can be much different, and in many ways, potentially worse (or at least as bad). Let me give you an example of this phenomenon in action, keeping in mind the 30:1 neurological ratio.
The very first Chiropractic Adjustment was given by a magnetic healer (DD Palmer of Davenport, Iowa) to a janitor (Harvey Lillard) in his building. As the story goes, Lillard had injured his upper back or neck, and very shortly after that went deaf. Palmer made an adjustment to the area of Lillard’s neck that he palpated as “out of place” and low-and-behold, Lillard’s hearing returned in miraculous fashion.
Palmer, ever the showman, started a massive advertising campaign that brought people from far and wide for these miraculous new “adjustments”. And while there probably were not as many cases of restored hearing as Palmer was hoping to see, there were miraculous results nonetheless. How does this relate to the 30:1 motor to sensory nerve ratio? Stay with me for just a moment and we’ll get thru this rabbit hole together.
For a very long time the chiropractic profession has used a simple analogy — an analogy that is incorrect in the vast majority of patients. “You see Mrs Jones, the reason you have (insert problem of choice here) is because you have a bone ‘pinching a nerve’ in your neck that is choking off the electric impulses in the same way that a kinked garden hose shuts off the flow of water.” However, just like we talked about earlier, the fact that this aspect of the model is incorrect has absolutely no bearing on the way the adjustment is delivered or the results the patients receives or doesn’t receive.
The result of this information (the 30:1 nerve ratio) is that each and every chiropractor who has been in practice for any length of time can tell you wild stories about “curing” their patients of (insert problem of choice here). I’ve seen more than a few that have happened to my patients over the years. We’ve had cases of people being adjusted for NECK PROBLEMS get their THYROID FUNCTION back.
I’ve seen more cases of DIGESTIVE ISSUES of every shape, size and kind being resolved thru adjusting the spine than you can imagine. A patient who had been (erroneously) diagnosed with both MS and a stroke was CURED WITH A SINGLE ADJUSTMENT. And in similar fashion to Harvey Lillard, a 42-year case of deafness was likewise solved with a single adjustment (HERE).
While curing deafness is certainly not “the norm” in my clinic, astounding results are happening in every chiropractic clinic with some degree of regularity, always leading me to wonder just how many people are living with problems that could be solved easily? And at least chiropractically speaking, it’s because every single mechanoreceptive impulse that is being inhibited from firing due to the fact it is not being moved or cannot move, is in response, inhibiting thirty nerve impulses coming from the motor side of the equation (from the brain).
An Example of the Fascia or Pain, Pain or Fascia Phenomenon in Action
A brand new study from Japan and published in the March issue of the Journal of Physical Therapy Science (Effect of Low Back Pain on the Muscles Controlling the Sitting Posture); while not mentioning the 30:1 ratio, showed how the sensory side of the nervous system affects the motor side.
This study looked at the relationship between NON-SPECIFIC BACK PAIN (the number one reason for back pain; according to the experts as much as 90%), the THORACOLUMBAR FASCIA (the “Christmas tree” in the small of the back), and something known as the flexion-relaxation phenomenon (FRP). What is the FRP?
The flexion-relaxation phenomenon is exactly what it sounds like. When a person bends forward at the waist (trunk flexion), the activation of the abdominal muscles “silences” or shuts off activation of the muscles of the low back (spinal errectors and thoracolumbar fascia).
This reflex can go awry a couple different ways. Either by living in a “slouched” posture, usually caused by sitting too much, or by chronic pathological activation of the afore-mentioned muscles (spasms, tension, pathological tightness). Clear back in 2005, the Journal of Manipulative & Physiological Therapeutics put it this way (The Biomechanical and Clinical Significance of the Lumbar Erector Spinae Flexion-Relaxation Phenomenon: A Review of Literature).
A number of studies have shown differences in the FRP between patients with chronic low back pain and healthy individuals. Persistent activation of the lumbar musculature among patients with back pain may represent the body’s attempt to stabilize injured or diseased spinal structures via reflexogenic ligamentomuscular activation thereby protecting them from further injury and avoiding pain.
The myoelectric silencing of the erector spinae muscles in the trunk flexion posture is indicative of increased load sharing on passive structures, which tissues have been found to fail under excessive loading conditions and shown to be a source of low back pain. The studies that show differences in the presence of the FRP among patients and control subjects.”
Did you catch that SHAGGY? A slouching posture can cause “passive structures” (basically, soft-tissues other than muscles) “to fail“. This “failure” can be catastrophic, with tissues being completely torn or torn away from the bone (avulsions) or, more likely and far more common, microscopically catastrophic, leading to the cycle of abnormal function and pain we’ve been discussing.
Think about it like this. As I stated earlier, the most abundant connective tissue in the body (fascia) neither images on MRI, nor is ever really discussed as a potentially injured tissue, when looking at potential causes for your pain. Yet research shows that it commonly “fails” in these abnormal conditions — conditions that have become so normalized in our society we look at them as normal. In other words, pain itself has the ability to inhibit the normal firing of neuro-musculo-fascial reflexes (MAKE SURE YOU REMEMBER THAT FASCIA IS NOT REALLY “PASSIVE”), which will lead to more of the same — a vicious cycle if you will.
The study being discussed carried these cherry-picked conclusions concerning people who slump when they sit….
“In patients with nonspecific low back pain, the thoracolumbar extensor is hyper-contracted, and the FRP disappeared. The disappearance of the FRP is associated with the exacerbation of LBP. The slump sitting position greatly flexes the spine and spinal column in a forward bending motion, and for the muscles of the trunk, it is a typical posture for relaxation. Alternatively, it is an abnormal posture inducing back pain. Based on studies on slump sitting and the FRP, slump sitting may decrease lower back muscle activity.
This study showed that slump sitting was associated with reduced muscular activation of the thoracic erector spinae, lumbar erector spinae, lumbar multifidus, external oblique, internal oblique, upper portions of the gluteus maximus, and iliopsoas in the non-LBP group. These findings suggest that slump sitting is a pain-inducing position rather than a relaxing position for patients with recurrent LBP.”
Not surprisingly the authors went on to discuss things like LOWER CROSSED SYNDROME and UPPER CROSSED SYNDROME. It’s why I look at the hips and pelvis of most of my patients; even those only complaining of neck pain.
“The most prevalent musculoskeletal pain conditions transitioning to chronicity and contributing to the global burden of disease include low back pain and neck pain. In many cases of low back pain, no skeletal cause is obvious; thus, this type of chronic pain is often considered nonspecific. Such musculoskeletal pain conditions are favorably affected by increased bodily activity.”
Increased bodily activity. It’s a no-brainer both as a cause and as a solution. Movement / motion, while not always easy, is always beneficial in the long run. This study went on to look at whether or not problems arising from from fascia manifested themselves as body surface pain. The authors used the TEMPORAL FASCIA as the test, looking to see if stimulus to the fascia caused measurable pain on the skin in certain populations.
The research team “demonstrated that fascia stimulation at a sufficient stimulus intensity elicited significant cross-tissue facilitation (referred hyperalgesia), a hallmark sign of nociceptive central sensitization.” In other words and for reasons that were not always well understood, the authors discovered the early stages of Central Sensitization; the phenomenon where pain gets locked into the brain and played on a loop, sort of like the old days of cassette tapes playing on auto-reverse until you turned them off.
So; Whether Pain / Inflammation Caused the Fascial Adhesion or the Fascial Adhesion Caused the Pain / Inflammation, What Can Be Done For Relief?

During a treatment, the provider will assess any possible movement limitations associated with the fascia. Then, they will use their hands or special instruments to apply pressure to the fascia. Sometimes, fascia manipulation can be uncomfortable or painful, especially if the fascia tension is deep and requires a lot of pressure. You may notice a decrease in pain and an increase in mobility after just one treatment…. From Vanessa Caceres’ article, What is Fascia Manipulation? in the February 19, 2021 issue of USA Today
I’m hoping that you have had a chance to look at my TESTIMONIAL PAGE as well as at least a few of our hundreds upon hundreds of VIDEO TESTIMONIALS. Our goal is always to provide as much relief of pain as is possible in one visit. It’s what allows me to tell many most of my patients up front, “if I can help you with this particular problem, you will know within a day or two.” The videos show that many people know immediately. Or in Caceres’ words, “after just one treatment“. Speaking of immediately….
Just the other day the Journal of Clinical Biomechanics published a study titled Immediate Effects of Myofascial Release on Neuromechanical Characteristics in Female and Male Patients with Low Back Pain and Healthy Controls as Assessed by Tensiomyography: A Controlled Matched-pair Study, while the International Journal of Environmental Research and Public Health recently (last month) published a study titled Effects of a Massage Protocol in Tensiomyographic and Myotonometric Proprieties.
There are a host of takeaways, both for those who treat musculoskeletal-based chronic pain, as well as for those who cope with it daily. And as a side note: the “Myofascial Release” used in these studies appeared to me more like manual stretching than something that would be done by ultra-skilled practitioners, which would actually accentuate the study’s conclusions when extrapolated to the clinical setting, where people are typically treated by experienced and adept clinicians / therapists.
For starters, both studies talked about evaluating the efficacy of bodywork via a test called “Tensiomyography” (TMG). TMG is a method for measuring a host of subsets of muscle contractions, including ‘stiffness,’ and speed of contraction that you can read about HERE. After talking about a host of issues, including athletic performance and non-specific back pain, a few of the things mentioned specifically by these studies included….
- “……improving the performance of athletes and reducing the risk of injury.“
- “….causes local hyperemia, which leads to an increase in the supply of oxygen to the tissues on which it is applied…” (HERE), and “...improves microcirculatory homeostasis….” (HERE).
- “…..increase in contraction time and maximal displacement variables, as well as a reduction in stiffness and tone.“
- “…significant immediate effects in neuromechanical characteristics of the lumbar spinal errector muscles in patients with LBP following a single myofascial release intervention. The acute post-interventional adaptations were particularly evident in the velocity of contraction.“
The immediate responsiveness on muscle contractile dynamics following myofascial release in the LBP group may have been mediated by several interconnected pathways. For instance, an accumulation of hyaluronan between the layers of deep fascia and the underlying epimysium has been associated with non-specific pain syndromes. This may alter the tissue’s density, and consequently, compromise the entire lumbar myofascial structures…..
Considering these aspects, it seems plausible that pressure applied during myofascial release altered hyaluronan viscosity, and, in turn, enhanced the sliding ability between myofascial tissue layers. As a consequence, improved fluid dynamics and more compliant tissue viscoelastic behaviour might have had an impact on the mechanoreceptors’ sensitivity in that zone.
As you can see from this cherry-picked quote, not only is “fascial neuroplasticity” something we should be striving to better understand and study in greater detail, it is something that shows evidentially that bodyworkers are on the right path and have been for, well, millennia.
Far more so than modern medical practitioners, who RUSHEDLY MEET WITH PATIENTS WITHOUT REALLY LISTENING TO THEM or truly EXAMINING THEM; instead, running a myriad of WORTHLESS TESTS and then, in far too many cases, TREATING THEM IN A MANNER NOT SUPPORTED BY THE “BEST EVIDENCE,” (TREATMENTS THAT ARE OFTEN DANGEROUS — OR EVEN DEADLY). Repeat.
Furthermore (and here is the biggest takeaway from this research), we can see that by increasing mechanoreceptor sensitivity via improvement of fascial function from bodywork (IN MY CASE, TISSUE REMODELING), we are increasing proprioception, or the body’s ability to better sense where it is at in space (DR. CARRICK TALKS A LOT ABOUT THIS PHENOMENON). The end result or goal of said treatment is moving the individual back toward that ideal 30:1 ratio mentioned earlier, as opposed to their steadily moving away from it, which is exactly where they will go without addressing the adhesed fascia.
So, to answer the question posited in the beginning of today’s post — is your pain due to problems in your fascia, or are the problems in your fascia the result of your pain? — the answer is a resounding “yes”. As many of you knew from the beginning, the pathways to destruction are many and bidirectional. Multi-directional might be a better word in many cases.
If you are interested in starting the process of regaining your health; you’ll have to own up to the realization that no matter your circumstances (and I very much realize some of you are in circumstances not of your own making), your health is largely up to you. And while bodywork is fantastic; NECESSARY, IN FACT, IF YOU WANT TO ACHIEVE AND MAINTAIN HEALTH, there are any number of steps you need to be taking to move the process forward. I’ve CREATED A LIST of just a few of them for you.
